Our Previous Samples
Nursing Informatics Paper DiscussionIntroductionNursing informatics is a recent ...
Nursing Informatics Paper Discussion
Introduction
Nursing informatics is a recent but critical specialty in nursing. It is a specialty that combines nursing science with nursing information technology to develop systems that improve patient care while reducing medical errors. Patient medical data has emerged as a critical factor in reducing medical errors and improving patient outcomes. Nursing informatics is a branch of technology that allows health facilities to efficiently collect patient data/information leading to improved safety, quality of care, and patient outcomes. Nursing informatics is a critical information management system in the medical field as it is the driving force behind development, improvements, decision-making, and clinical outcomes.
Role of Nursing Informaticists
Nursing informatics is a highly technical role that needs nursing professionals with high skills and knowledge of data and technology. Nursing Informaticists have numerous responsibilities as elaborated below.
Data Collection and Analysis
In the United States of America, over 95% of all healthcare facilities use some kind of certified health record system. These systems are the backbone of the operations of these facilities as they change the way healthcare is delivered and managed. However, these traditional health record systems are plagued with rampant inefficiencies leading to numerous medical errors. Furthermore, the inefficiency of these traditional health record systems impacts the provision of quality care for patients and the general patient experiences.
Nursing informaticists help to eradicate the rampant inefficiencies of the traditional health record systems. One of the critical issues that healthcare facilities have had to deal with is the problem of medical errors-mostly occasioned by wrong customer data/information. Nurses, physicians, and other medical professionals rely on patient data/information to make critical decisions on patients’ health, intervention, and outcomes.
Wrong information captured in these traditional health record systems automatically results in wrong decisions by nurses and doctors. The role of nursing informatics specialists is to reduce or eradicate errors related to patient information by transitioning patient records/data from paper form to digital format. A transition from the manual entry of information in paper form to digital records greatly reduces any chances of errors. The nursing informatics specialists must ensure that patient records/data are errorless.
Nursing Informatics must align nursing best practices with patient outcomes and clinical care. The most critical objective of nursing informatics is to improve clinical care and patient outcomes through the adoption of best practices. To achieve excellent clinical care, nursing informatics specialists are critical to processes such as the review of clinical workflow, process designs, creating effective treatment plans based on patient information and data, and developing new diagnostics (Ng et al., 2018). All the processes mentioned above have a direct impact on the quality of care given to patients. Working in collaboration with other medical professionals, nursing informatics specialists create the best course of action for patients that lead to value-based and patient-centered care.
Nursing informatics specialists work to improve protocols, policies, procedures, and processes. Data is the lifeline of any medical facility because all decisions are made using data/information (Jabour et al., 2021) Available data/information are used by healthcare facilities to make critical decisions about patients and the direction of growth of such facilities. Most importantly, information is used to evaluate and measure the performance of all protocols, procedures, policies, and processes in caregiving facilities.
For example, it is the responsibility of nursing informaticists to measure the way all specific parts of a healthcare organization are performing with emphasis on patient outcomes. Based on the performance of each part, nursing informaticists can initiate changes to specific parts to streamline activities. Emphasis is put on eliminating bottlenecks, reducing inefficiencies, and improving the overall care and safety for patients.
Nurse Informaticists and Other Health Care Organizations
I researched the experience of other health care organizations with nurse informaticists and there were many cases of success and a few challenges. The integration of the nurse informaticists into the team is done by creating a distinct position for the role. The nurse informaticists are at the center of communication and information within a hospital setting (Mosier, 2018). One of the major roles that the position holder will play is training team members on how CPRS works.
As a trainer, the nurse informaticists work closely with other staff such as doctors, fellow nurses, lab technicians, and the administrative staff to ensure that patient information is accurately captured and contained in the system. Secondly, the nurse informaticists must ensure that there is a smooth flow of communication between different healthcare professionals as far as patient records are concerned (Sipes, 2016). The creation of a special office for the nurse informaticists helps him/her to effectively liaise and coordinate with other team members.
Impact of Full Nurse Engagement in Health Care Technology
Data Privacy is guaranteed when using nursing informatics. The disadvantage with the paper-based system of health records is that anyone can access patient data or sensitive data belonging to a healthcare facility. Using nursing informatics, the security, privacy, and confidentiality of health information are guaranteed. To begin with, the systems of health records created by nursing informaticists are only accessible to authorized personnel. For example, only health professionals that deal with a patient are privy to their data/information. This fact means that for anyone to access a patient’s health records, they must have the relevant authority and clearance to do so. This way, the technologies adopted restrict unauthorized access to sensitive hospital and patient information.
Nursing informatics leads to better patient outcomes. Patient records have a direct impact on a patient, the intervention method chosen, the treatment plan, the provision of quality care, and the overall outcome. Through nursing informatics, the chances of medical errors are minimal due to improved accuracy it confers in capturing patient data. Secondly, the role of nursing informatics promotes interprofessional cooperation of different health professionals within a facility which improves the quality of care given to patients. In particular, nursing informatics improve patient safety, precision in diagnosis, communication, and overall effectiveness of patient care (McGonigle, 2017). In the past, the healthcare facility I work for has witnessed some cases of patient misdiagnosis occasioned by incorrect patient information/data.
Opportunities and Challenges
Nursing informatics provides the best chance to reduce medical errors. Nursing informatics can reduce nursing errors by up to 80% compared to the traditional health record systems. Reduced medical errors have a positive impact on the quality of care for patients, improves patient safety, and helps to improve overall patient care. For hospitals, reduced medical errors mean improved reputation, good customer relations, and reduced cost of operations. For example, medical errors cost hospitals millions of dollars every year-money that would be used on other critical ventures. Nursing informatics allows healthcare facilities to increase the level of quality provision as well as cutting down the costs of operations.
One of the challenges for many healthcare facilities concerning the implementation of nursing informatics is a cost factor. The creation of the position of a nursing informaticists is a costly venture because it is a role that is highly integrated with other roles. Every health professional is expected to acquire information from a centralized point within a facility when using nursing informatics. It requires a lot of money to create and develop technological and communication channels between professionals (Mosier et al., 2019). Doing so requires creating friendly user-interfaces for all professionals that need access to health records. The initial investment in creating a smart digital health record platform is expensive. Besides, there must be highly trained professionals to run the project. The cost of running and maintaining the project may be inhibitive for some health facilities.
Conclusion
Nursing informatics plays a critical role in the nursing field. Today, the term patient outcomes is a critical feature that defines and shapes how medicine is practiced. Nursing informatics is at the core of improving the quality of healthcare for patients. It also impacts patient experiences meaning that patient outcomes depend on nursing informatics. Most importantly, nursing informatics nursing informaticists help to eradicate the rampant inefficiencies of the traditional health record systems. One of the critical issues that healthcare facilities have had to deal with is the problem of medical errors-mostly occasioned by wrong customer data/information.
Nursing Informatics Paper Discussion References
- Jabour, S. M., Chander, G., Riekert, K. A., Keruly, J. C., Herne, K., Hutton, H., Beach, M. C., Lau, B., Moore, R. D. & Monroe, A. K. (2021). The Patient Reported Outcomes as a Clinical Tool (PROACT) Pilot Study: What Can be Gained by Sharing Computerized Patient-Reported Mental Health and Substance Use Symptoms with Providers in HIV Care? AIDS and Behavior. https://doi.org/10.1007/s10461-021-03175-2
- McGonigle, D. (2017). Nursing Informatics and the Foundation of Knowledge. [MBS Direct]. Retrieved from https://mbsdirect.vitalsource.com/#/books/9781284142990/ https://doi.org/10.1016/j.outlook.2008.09.010
- Mosier, S., Roberts, W., & Englebright, J. (2019). A systems-level method for developing nursing informatics solutions. JONA: The Journal of Nursing Administration, 49(11), 543–548. https://doi.org/10.1097/nna.0000000000000815
- Ng, Y., Alexander, S., & Frith, K. H. (2018). Integration of mobile health applications in health information technology initiatives. CIN: Computers, Informatics, Nursing, 36(5), 209–213. https://doi.org/10.1097/cin.0000000000000445
- Sipes, C. (2016, January 1). Project Management: Essential Skill of Nurse Informaticists. Walden Library. https://eds-a-ebscohost-com.ezp.waldenulibrary.org/eds/pdfviewer/pdfviewer?vid=2&sid=d7e0961a-b9f5-48db-b31c-74719f7bace7%40sdc-v-sessmgr01
Also Read: Responding to Ethical and Legal Issues Example
READ MORE >>
Nursing Leadership Discussion 2IntroductionMedical errors have serious impacts o ...
Nursing Leadership Discussion 2
Introduction
Medical errors have serious impacts on patients, healthcare givers, and healthcare facilities. The most pronounced impacts include emotional, legal, and financial consequences. The government requires that grievous medical errors be reported for investigations and analysis. For nurses who make a medical error, consequences range from dismissal from a job, disciplinary action, possible criminal or civil lawsuits, and mental anguish. This paper is based on case studies 9-2 about a nurse who committed a grievous medical error leading to the death of a patient.
Steps To Take With the Nursing Staff to Stabilize their Emotions about the Situation
Causing the death of a patient accidentally causes tremendous mental anguish to nurses that find themselves in such situations. From the case study, the nurse is an emotional wreck and deeply regrets the incident. As her supervisor, I would get her to calm down by assuring her of the support from the facility. In the short term, the nurse would need to calm down and take control of her emotions. However, in the long term, the nurse would require professional counseling to deal with her emotional and mental anguish and trauma from the event. Judy also needs to stabilize the emotions of other nurses in the unit because they are devastated to see their senior colleague that they look up to go through so much pain. The nurses know that the mistake could have happened to any one of them which is the reason their share deep emotional pain with the nurse that committed the error. Consequently, it is essential to also get other nurses from the unit to control their emotions.
Steps to Heal the Brokenness on the Unit and to Prevent a Reoccurrence
Being one of the best nurses in the unit that committed the fatal medical error, the mental anguish and emotional pain run deep throughout the unit. To begin with, the nurse has always maintained an impeccable ethical record and is also one of the best and senior nurses in the hospital. Her track record makes her a role model for the other nurses in the unit as they look up to her. All the nurses in the unit are affected by this mishap because of the feeling that it could have happened to any one of them. Even more distressing to the unit is that the incidence happened to one of the best nurses among them.
As the manager, I would call for professional counseling for all members of the unit to help them deal with the emotional and mental trauma (Kellog et al., 2018).Concerning preventing future occurrences of such errors, I would organize a retraining session with all nurses to remind them of the common mistakes that lead to medical errors. For example, I would stress to the nurses that consulting a patient’s armband is a mandatory practice that must happen each time a nurse visits a patient. Additionally, I would stress the importance of reading a patient’s records to know their status and the course of action needed.
Steps to take on the Nurse
This situation is a difficult one for everyone involved which makes it even more difficult to decide on the steps to take on the nurse. On the one hand, the nurse is one of the best with a sterling performance and observance of ethics. On the other hand, the family of the deceased need to see a firm decision made since they lost their loved one due to the nurse’s error. Additionally, the error has prompted a serious investigation of the facility by the health department. Matters are exacerbated by the fact that the media has already made public the news of the unfortunate incident. Like Judy, I would advocate for some form of compensation for the grieving family to help ease their pain (Lee, 2018). For the nurse, I recommend some form of punishment such as some time off from work with half pay and mandatory therapy sessions. It is my view that the nurse should not face the rest of her life paying for the mistake. This is not in any way meaning that the error is to be downgraded.
What to Do To Help the Hospital Recover from the Incidence
The facility’s management must work tirelessly to reclaim the hospital’s dented image through active public relations. The hospital must convince the public they have put in place measures to ensure that another regrettable incidence of the same nature never occurs (Robertson, & Long, 2018). One of the best ways to engage the public is to show them the changes that have been introduced to curb medical errors at the facility. Additionally, the hospital can engage in social corporate responsibility activities to win their trust.
Conclusion
From the case study, the healthcare facility and everyone involved is devastated by the incident. The hospital risks bad reputation and public relations as well as possible litigation. On the other hand, the nurse at the center of the error risks losing her license amid the mental trauma she suffers from the ordeal. As the manager, I would advocate for some form of compensation for the grieving family to help ease their pain. For the nurse, I recommend some form of punishment such as some time off from work with half pay and mandatory therapy sessions.
References
- Kellogg, M., Knight, M., Dowling, J., & Crawford, S. (2018). Secondary Traumatic Stress in Pediatric Nurses. Journal Of Pediatric Nursing, 43, 97-103. https://doi.org/10.1016/j.pedn.2018.08.016
- Lee, E., 2017. Reporting of medication administration errors by nurses in South Korean hospitals. International Journal for Quality in Health Care, 29(5), pp.728-734.
- Robertson, J. and Long, B., 2018. Suffering in Silence: Medical Error and its Impact on Health Care Providers. The Journal of Emergency Medicine, 54(4), pp.402-409
READ MORE >>
Nursing Research and Evidence Based Practice SampleEvidence-based practice in nu ...
Nursing Research and Evidence Based Practice Sample
Evidence-based practice in nursing has been proven to result in quality patient care. The goal of nursing research, on the other hand, is to enable nurses to apply their education to discover new advancements and promote evidence-based practice. Acquisition of knowledge and interventions for evidence-based practice is an elemental skill required by nurse practitioners in any clinical encounter. The evidence-based practice further requires that a health practitioner possess boundless background information about diseases and potential interventions along with the necessary experience to properly examine specific foreground information vital in making clinical decisions. In this piece of writing, I will extensively examine hypertension as a risk factor for stroke using the PICOT format and leveraging extensive literature search.
The PICOT Question
In elderly hypertensive patients, how does well control of hypertension compared to poor control of hypertension affect the incidence of stroke? Hypertension defined as blood pressure> 120/80mmHg (Wajngarten & Silva, 2019) despite being the identified clinical health problem also provides an opportunity for improvement of health outcomes since it is a modifiable risk factor. The role of hypertension as an independent risk factor for stroke has vividly been elaborated in literature (Wajngarten & Silva, 2019). In addition, hypertension is also a risk factor for various health problems among them renal impairment and myocardial infarction (Benetos et al., 2019). Benetos et al. (2019) in the journal of Circulation Research further states that long-term management of hypertension is critical for the reduction in mortality and morbidity. Hypertension further is a problem as its incidence rises with aging as a result of arteriole stiffening that comes with aging. Poorly controlled hypertension can be a consequence of a multitude of factors including non-adherence to antihypertensive, inadequate therapy, inappropriate therapy, resistant hypertension, drugs, obesity, and diet (Wajngarten & Silva, 2019). Nevertheless, well-controlled hypertension reduces the risk of stroke which is the second and third cause of mortality and disability worldwide respectively (Wajngarten & Silva, 2019). Therefore, this clinical problem when controlled through antihypertensives and lifestyle modification in conjunction with patient education contributes to an overall enhancement of health.
Literature Search
A literature search is an elemental skill that all nurse practitioners need to have. For my literature search, I used keywords including elderly, stroke, uncontrolled hypertension, controlled hypertension, and elderly to search databases such as Google, Google Scholar, CINAHL, MEDLINE, Trip, PubMed, and ProQuest. I specifically looked for peer-reviewed articles that were closely related to my PICOT question that had been published within the last five years. Subsequently, a total of five articles discussed below were selected.
Sarfo et al. (2020) in the Journal of the Neurological Sciences did research to assess the association between lower BP target and incident stroke risk in geriatric Ghanaians with hypertension. This retrospective evaluation of prospectively collected data of 1365 hypertensive patients over 18 months was analyzed using multivariable logistic regression models and the finds showed that 45.8% had uncontrolled hypertension. The incident of stroke was 0 stroke events/100py for BP?<?120/80?mmHg, 1.98 for BP between 120 and 159/80-99?mmHg, and 2.46 events/100py at BP?>?160/100?mmHg. Ultimately, a conclusion of the low incidence of stroke with well-controlled hypertension was made.
Han et al. (2017), concerned with the greatest burden of stroke in China, carried out research to assess the impact of suboptimal controls of hypertension on the incidence of stroke. In this population-based 10-year prospective cohort study, out of 1646 participants with hypertension, 55.4% were previously undetected, 7.0% detected but not treated, 27.5% treated but not controlled while only 7.7% were controlled. An incidence of 211 cases of stroke was recorded. Compared to normotensive cohorts and those with controlled hypertension, the multivariate-adjusted health risk for stroke increased by 1.63 in the undetected, 2.21 in the untreated, and 3.34 in the uncontrolled. This research concluded that a substantial number of people could be saved with the appropriate management of hypertension.
Lee et al. (2017) on the other hand researched to investigate the effect of adherence to antihypertensive medication on stroke incidence. This population-based retrospective cohort study using Poisson regression analysis by generalized estimating equation models found that among 38?520 patients with hypertension, the incidence of stroke was 957 (2.5%). Non-adherence to medication was significantly associated with a higher risk of stroke (intermediate adherence: adjusted relative risk (aRR)=1.13 to 1.21; poor adherence: aRR=1.27, to 1.38). This study concluded non-adherence to antihypertensives contributes significantly to the incidence of stroke and encouraged healthcare providers to adopt strategies to enhance patient adherence to medications.
Ishii et al. (2017) in the American Journal of Hypertension, conducted research to look into the relationship of hypertension and systolic blood pressure (SBP) with the risk of stroke or bleeding in atrial fibrillation patients. This community based prospective survey found out that hypertensive high blood pressure group (n=305) SBP > 150mmHg was associated with increased risk of stroke (hazard ratio =1.74) and major bleeding (hazard ratio= 2.01) compared to the hypertensive low blood pressure group (SBP<150 mmHg) and the control normotensive group. This research concluded that the incidence of stroke is higher in hypertensive individuals with SBP>150 mmHg.
Li et al. (2017) also conducted a study to investigate the optimal blood pressure trajectories for risk prediction of both intracerebral hemorrhage and cerebral infarction. This large prospective cohort study in China after statistical analysis documented 1034 incident cases of cerebral infarction and 187 cases of intracerebral hemorrhage out of 79 385. In addition, Individuals in stage 2 hypertension-stable systolic BP trajectory (175–179 mm Hg) had the highest risk of intracerebral hemorrhage (adjusted hazard ratio of 12.4) and cerebral infarction (adjusted hazard ratio of 5.07), relative to the normotensive-stable group. This study concluded that BP trajectories were associated with an increased risk of stroke.
The article that best supports nursing interventions for hypertension is the article by Han et al. (2017) which assesses the impact of suboptimal control of hypertension on the incidence of stroke. Han et al. (2017) urge the healthcare providers particularly the nurses to detect hypertension early through screening. Furthermore, emphasis on the treatment of already diagnosed hypertension is unquestionably elaborated in this article. The article further encourages nurses to adequately treat hypertension through various interventions to ensure that it is well controlled to reduce the incidence of adverse events such as stroke. In contrast, the article by Lee et al. (2017) only stresses the need to adhere to antihypertensives to prevent stroke while the articles by Sarfo et al. (2020), Li et al. (2017), and Ishii et al. (2017) all concentrate on demonstrating the impact and overwhelming evidence of the significant contribution of uncontrolled hypertension to development of stroke.
Conclusion
A literature search is a vital skill in clinical practice. Existing literature undoubtedly associates uncontrolled hypertension with an increased incidence of stroke. Nurses play an indispensable role in reducing the burden of hypertension through early detection, adequate treatment of established cases, and patient education. All these along with strategies to facilitate adherence to antihypertensive medications reduce the incidence of stroke and its associated morbidity and mortality.
References
- Benetos, A., Petrovic, M., & Strandberg, T. (2019). Hypertension management in older and frail older patients. Circulation Research, 124(7), 1045–1060. https://doi.org/10.1161/CIRCRESAHA.118.313236
- Han, T. S., Wang, H. H.-X., Wei, L., Pan, Y., Ma, Y., Wang, Y., Wang, J., Hu, Z., Sharma, P., & Chen, R. (2017). Impacts of undetected and inadequately treated hypertension on incident stroke in China. BMJ Open, 7(10), e016581. https://doi.org/10.1136/bmjopen-2017-016581
- Ishii, M., Ogawa, H., Unoki, T., An, Y., Iguchi, M., Masunaga, N., Esato, M., Chun, Y.-H., Tsuji, H., Wada, H., Hasegawa, K., Abe, M., & Akao, M. (2017). Relationship of hypertension and systolic blood pressure with the risk of stroke or bleeding in patients with atrial fibrillation: The Fushimi AF registry. American Journal of Hypertension, 30(11), 1073–1082. https://doi.org/10.1093/ajh/hpx094
- Lee, H. J., Jang, S.-I., & Park, E.-C. (2017). Effect of adherence to antihypertensive medication on stroke incidence in patients with hypertension: a population-based retrospective cohort study. BMJ Open, 7(6), e014486. https://doi.org/10.1136/bmjopen-2016-014486
- Li, W., Jin, C., Vaidya, A., Wu, Y., Rexrode, K., Zheng, X., Gurol, M. E., Ma, C., Wu, S., & Gao, X. (2017). Blood pressure trajectories and the risk of intracerebral hemorrhage and cerebral infarction: A prospective study. Hypertension, 70(3), 508–514. https://doi.org/10.1161/HYPERTENSIONAHA.117.09479
- Sarfo, F. S., Mobula, L. M., Adade, T., Commodore-Mensah, Y., Agyei, M., Kokuro, C., Adu-Gyamfi, R., Duah, C., & Ovbiagele, B. (2020). Low blood pressure levels & incident stroke risk among elderly Ghanaians with hypertension. Journal of the Neurological Sciences, 413(116770), 116770. https://doi.org/10.1016/j.jns.2020.116770
- Wajngarten, M., & Silva, G. S. (2019). Hypertension and stroke: Update on treatment. European Cardiology, 14(2), 111–115. https://doi.org/10.15420/ecr.2019.11.1
READ MORE >>
Nursing Roles Graphic Organizer NUR 513 Week 2Topic 2 Nursing Roles Graphic Orga ...
Nursing Roles Graphic Organizer NUR 513 Week 2
Topic 2 Nursing Roles Graphic Organizer NUR 513 Week 2
Advanced registered nurses work in highly collaborative environments and must collaborate with interdisciplinary teams in order to provide excellent patient care.
Besides knowing the role and scope of one’s own practice, it is essential to understand the role and scope of other nurse specialties to ensure effective collaboration among nurses, the organization, and other professionals with whom advanced registered nurses regularly interact.
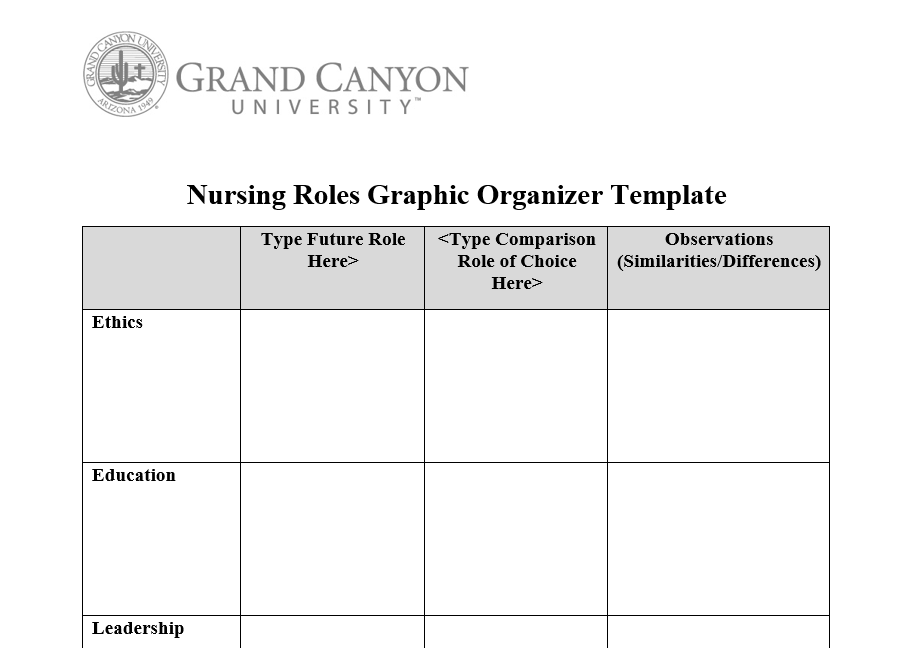
Use the “Nursing Roles Graphic Organizer Template” to differentiate how advanced registered nurse roles relate to and collaborate with different areas of nursing practice.
Compare your future role with one of the following: nurse educator; nurse leader; family nurse practitioner; acute care nurse practitioner; graduate nurse with an emphasis/specialty in public health, health ca. re-administration, business, or informatics; clinical nurse specialist; doctor of nursing practice. Indicate in the appropriate columns on the template which roles you are comparing.
https://nursingbay.com/wp-content/uploads/2020/11/Nursing-Roles-Graphic-Organizer.mp4Make sure to compare the following areas of practice in your graphic organizer:
- Ethics
- Education
- Leadership
- Public Health
- Health Care Administration
- Informatics
- Business/Finance
- Specialty (e.g., Family, Acute re)
Include any regulatory bodies or certification agencies that provide guidance or parameters on how these roles incorporate concepts into practice Nursing Roles Graphic Organizer Template NUR 513 Week 2.
You are required to cite three to five sources to complete this assignment. Sources must be published within the last 5 years and appropriate for the assignment criteria and nursing content.
While APA style is not required for the body of this assignment, solid academic writing is expected, and documentation of sources should be presented using APA formatting guidelines, which can be found in the APA Style Guide , located in the Student Success Center.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
NUR 513 Week 2 Nursing Roles Graphic Organizer Template
Ethics
Clinical nurse specialists demonstrate moral judgment expertise and assist public health nurses in dealing with specific moral quandaries.
Furthermore, the Code of Ethics rules for Nurses with Interpretive Statements form the basis for CNS practice (Fulton, Lyon, & Goudreau,2014).
Furthermore, CNSs value honesty and independence and may advocate for both clients and public health nurses Nursing Roles Graphic Organizer Template NUR 513 Week 2. Last, CNSs participate in civic activities and education addressing ethical concerns such as advance directives and end-of-life care.
The stewards of nursing ethics for nurses and nursing students are nurse educators, on the other hand. Their responsibility requires them to ensure that nurses and students adhere to ethical standards (DeNisco & Baker, 2014). Additionally, these nurses use evidence-based techniques to encourage the adoption of moral standards across the ethical spectrum.
Both CNSs and nurse educators are custodians of ethical codes of conduct in nursing practice. The two advanced nursing specialties inspire and guide nurses regarding the application of ethical standards to various situations Nursing Roles Graphic Organizer Template NUR 513 Week 2.
Whereas the role of nurse educators is limited to the practice setting and the classroom, the CNSs influence the adoption of the ethical standards at the community level in addition to practice setting.
Education
As advanced nurse practitioners, all clinical nurse specialists are required to hold a Master’s of Science in Nursing degree. Moreover, one may also become a CNS if they possess other graduate level program preparation relevant to the CNS role. However, the above qualification needs to have the authorization of the ACEN (Accreditation Commission for Education in Nursing) or CCNE (Commission on Collegiate Nursing Education) (DeNisco & Baker, 2014).
In addition, they need to have the latest license as registered nurses. Lastly, they also should have competed over 500 hours that are supervised in their specialty area. Some CNSs may also have doctorate degrees but this requirement is not mandatory.
The basic requirement for becoming a nurse educator is a certification as RNs. A majority of these nurses have a Master’s in Nursing degree; but various universities require them to have a doctorate degree to qualify as nurse educators (Bastable, 2019). Further, having a post-master’s degree or certificate in nursing may be necessary but not mandatory. Nurse educators also need to have certification in their area of practice.
The two specialties share the necessity for RN licensure and Masters of Science in nursing as the minimum requirements Nursing Roles Graphic Organizer Template NUR 513 Week 2. Further, they can also acquire doctorate degrees in their respective specialties. However, the need for over 500 hours in practicum experience does not apply for nurse educators since they mostly handle the academic stuff.
Leadership
Clinical Nurse Specialists are role models, mentors, and leaders in practice. They aid the nursing personnel in accomplishing supreme levels of professional advancement. They work extremely hard to impact the legislative and decision-making bodies to enhance client care Nursing Roles Graphic Organizer Template NUR 513 Week 2. Thus, CNSs offer leadership and direction to enhance staff participation in professional development activities, enhance client outcomes, and improve healthcare efficacy (Mayo et al., 2017).
Through their teamwork with staff as well as the fact that they encourage their participation, CNSs initiate and also revise and initiate guidelines that are intended to improve evidence-based practice in care settings, address contemporary issues in health care and also embody accepted changes in the management of care (Fulton, Lyon, & Goudreau,2014). Lastly, via formal and informal mentoring and teaching, CNSs disseminate nursing care and practice information, which impacts practice change and also enhances health outcomes.
Leadership forms an important part of nurse educators’ job description. Leadership requirements of certain nurse practices are manifested through their ability to influence change processes (DeNisco & Baker, 2014) Nursing Roles Graphic Organizer Template NUR 513 Week 2. To this end, nurse educators influence the development of nursing curriculum via examining, updating, revising, and implementing the reviewed curriculum.
Further, their leadership role is also evident through their mentoring effect on nursing students, which influences the nursing theories adopted by the latter. Lastly, nurse educator leadership is similarly evident when they influence and guide the adoption of evidence-based practice in care settings so as to enhance patient outcomes.
The similarities between nurse educators and CNSs as relates to leadership is found in their ability to influence change in the practice setting. Their competence in evidence-based practice and change initiatives make them prime candidates to guide these changes.
Further, their leadership credentials also enable them to act as mentors to their subordinates both at the practice setting and school. However, while CNSs ensure the development of staff through taking part in professional development exercise, nurse educators only use their curriculum changes to influence professional development.
Public Health
Clinical nurse specialists play an important function in ensuring that the public enjoys their holistic view of wellness and health Nursing Roles Graphic Organizer Template NUR 513 Week 2. As part of their job description, CNSs enhance access to wellness and preventative care via early identification of community members predisposed to the causative agents of diabetes, and heart failure, among other chronic conditions.
In addition, CNSs offer care to ensure that such people are healthy so as to cushion them against chronic conditions (DeNisco & Baker, 2014). Also, CNSs play a crucial role in ensuring that communities understand the concept of ethical dilemma so that they can arrive at an ethically correct decision in matters such as end-of-life care.
Nurse educators participate in public health undertakings as a component of a multidisciplinary team. Their role is to use evidence-based practice to establish and deliver public health interventions for various health issues affecting communities (Bastable, 2019).
They accomplish this in their role as change agents in society.Further, nurse educators also participate in public health activities through interprofessional collaboration with public health professionals so as to formulate, back and examine clinical practice via proper frameworks. They also accomplish the above through the formulation of an apt environment regarding public health emergencies.
Both specialties ensure that the wellness of communities receives the necessary attention. They achieve this through acting as change agents. Nevertheless, whereas CNSs participate in public health activities, nurse educators participate through educational interventions. Also, nurse educators do not enlighten the community regarding ethical matters as is the case with CNSs.
Health Care Administration
Clinical nurse specialists serve as supervisors over their nursing colleagues at care facilities. In order to function optimally, CNSs need management roles such as executing clinical practice solutions, leading CNS clinics and increasing caseloads (Fulton, Lyon, & Goudreau,2014).
In addition, CNSs identify gaps in their areas of specialization and offer solutions to the same. However, the CNS will undertake these leadership roles while still doing their specialist functions.
Nurse educators also have a role in health care administration though to a limited extent. Essentially, they use their competence in evidence-based practice to support the execution of multifarious initiatives at either the practice or academic settings (DeNisco & Baker, 2014).
In addition, they are members of administrative committees whose roles include handling of departmental challenges, academic issues, and institutional policies.
As administrators, both CNSs and nurse educators act as change agents. However, whereas CNSs enjoy actual administrative duties, the nurse educators only handle delegated functions in care settings Nursing Roles Graphic Organizer Template NUR 513 Week 2. It is also worth noting that the administrative roles of nurse educators encompass both practice settings and academic institutions whereas CNSs only functions as administrators in health care facilities.
Informatics
CNSs improve the practice environment as well as the standard of care through the application of technology in a creative manner. An informatics clinical nurse specialist plays an essential role in ensuring that nurses embrace the usage of technology in practice settings including public health settings (Fulton, Lyon, & Goudreau, 2014). The roles of these CNSs also ensure supporting nurses and aid in the management of health care information systems.
Nurse educators use informatics to disseminate information from their evidence-based research. During this process, analytical science informatics as well as information management systems become useful to them (Toppping et al., 2015). Indeed, they also utilize cutting edge informatics technology to convey information in their various classes.
Both sets of nurses leverage the use of informatics to enhance the quality of care. However, whereas CNSs are focused on ensuring that facilities or environments embrace technology and information management systems, nurse educators use informatics systems to release pertinent information to relevant audiences.
Business/Finance
The development and implementation of cost-effective and innovative care delivery strategies so as to maximize on profits forms one of the fundamental administrative roles of CNSs (Mayo et al., 29017). They achieve the above objective via evaluation of factors associated with efficacy, safety, and cost and availability of resources when electing between options that may lead to the same outcomes (Fulton, Lyon, & Goudreau,2014). In addition, they may identify cost-cutting practice undertakings so as to improve the financial health of a care facility. Thus, possessing business knowledge is fundamental to CNSs.
Summers (2017) posits that nurse leaders need competence in business and finance areas to support some of the decisions that they make Nursing Roles Graphic Organizer Template NUR 513 Week 2. As formulators and implementers of curriculum and evidence-based practice solutions, having financial and business knowledge will enable them to deliver cost-effective measures.
Both nursing practices need financial/business acumen to as to make relevant decisions that will ensure cost-effectiveness. Further, the financial/business competences for the two nursing specialties are applied when implementing innovative solutions at their practice areas.
Specialty (e.g., Family, Acute Care)
Clinical Nurse Specialists’ opportunities for specialization are limitless. Virtually every area of nursing has a clinical nurse specialist. However, some of the most important specializations include: Public and Community Health, Pediatrics, Home Health, Gerontology, Diabetes Management, Child/Adolescent Psychological and Mental Health, Adult Psychiatric and Mental Health and Adult health among others.
Nurse educators are specialist nurses at various sections of the profession. The specialties for nurse educator spans family nursing, acute care nursing, among others (Bastable, 2019). Essentially, nurse educators specialize in all nursing specialties.
Both areas of nursing have limitless opportunities for specialization. The difference in these specializations may involve the functions.
Regulatory Bodies or Certification Agencies That Provide Guidance or Parameters on How These Roles Incorporate Concepts Into Practice
The American Nurses Credentialing Center (ANCC) administers the national examination for the CNS Core as well as the attendant specialty areas. The certification for CNSs requires renewal every five years as dictated by the ANCC (DeNisco & Baker, 2014).
In addition, various State Boards of Directors also offer CNS certifications. During this period, the CNSs will be assessed on their competence regarding the incorporation of the specialty’s roles into practice Nursing Roles Graphic Organizer Template NUR 513 Week 2.
The certification of Nurse Educators come from the American Association of College of Nursing. The role of the AACN is to ensure the presence of quality across the nursing education spectrum (DeNisco & Baker, 2014). In addition to AACN, the State Boards of Directors also participate in licensing nursing educators.
The certification for both the nurse educators and CNSs is influenced by State Boards of Directors. However, nationally, the ANCC certifies and credentials the former while the AACN is responsible for the latter.
Nursing Roles Graphic Organizer NUR 513 Week 2 References
- Bastable, S. B. (2019). Nurse as educator: Principles of teaching and learning for nursing practice. Burlington, MA: Jones & Bartlett Learning.
- DeNisco, S., & Barker, A. M. (2016). Advanced practice nursing: Essential knowledge of the profession. Burlington, MA: Jones & Bartlett Learning.
- Fulton, J. S., Lyon, B. L., & Goudreau, K. A. (2014). Foundations of clinical nurse specialist practice. New York, NY: Springer Publishing Company.
- Mayo, A. M., Ray, M. M., Chamblee, T. B., Urden, L. D., & Moody, R. (2017). The advanced practice clinical nurse specialist. Nursing administration quarterly, 41(1), 70-76. https://doi.org/10.1097/naq.0000000000000201
- Summers, J. A. (2017). Developing competencies in the novice nurse educator: An integrative review. Teaching and learning in Nursing, 12(4), 263-276.
- Topping, A., Bøje, R. B., Rekola, L., Hartvigsen, T., Prescott, S., Bland, A., … & Hannula, L. (2015). Towards identifying nurse educator competencies required for simulation-based learning: A systemised rapid review and synthesis. Nurse Education Today, 35(11), 1108-1113.
Nursing Roles Graphic Organizer NUR 513 Week 2 Rubric
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are not required to submit this assignment to LopesWrite.
Top of Form
Please Note: The assignment will not be submitted to the faculty member until the “Submit” button under “Final Submission” is clicked.
New Attempt
Nursing Roles Graphic Organizer Template NURS 513 Rubric Detail
100.0% Nursing Roles Graphic Organizer Criteria
10.0% Comparison of Roles in Relation to Ethics
A comparison of roles in relation to ethics is not included.
A comparison of roles in relation to ethics is present, but it lacks detail or is incomplete. A comparison of roles in relation to ethics is present.
A comparison of roles in relation to ethics is clearly provided and well developed. A comprehensive comparison of roles in relation to ethics is thoroughly developed with supporting details.
10.0% Comparison of Roles in Relation to Education
A comparison of roles in relation to education is not included.
A comparison of roles in relation to education is present, but it lacks detail or is incomplete. A comparison of roles in relation to education is current.
A comparison of roles in relation to education is clearly provided and well developed. A comprehensive comparison of roles in relation to education is thoroughly developed with supporting details.
10.0% Comparison of Roles in Relation to Leadership
A comparison of roles in relation to leadership is not included. A comparison of roles in relation to administration is present, but it lacks detail or is incomplete. A comparison of roles in relation to leadership is current.
A comparison of roles in relation to leadership is clearly provided and well developed. A comprehensive comparison of roles in relation to leadership is thoroughly developed with supporting details.
10.0% Comparison of Roles in Relation to Public Health
A comparison of roles in relation to public health is not included. A comparison of roles in relation to public health is present, but it lacks detail or is incomplete.
A comparison of roles in relation to public health is current. A comparison of roles in relation to public health is clearly provided and well developed. A comprehensive comparison of roles in relation to public health is thoroughly developed with supporting details.
10.0% Comparison Roles in Relation to Health Care Administration
A comparison of roles in relation to health care administration is not included. A comparison of roles in relation to health care administration is present, but it lacks detail or is incomplete.
A comparison of roles in relation to health care administration is present. A comparison of roles in relation to health care administration is clearly provided and well developed Nursing Roles Graphic Organizer Template NUR 513 Week 2. A comprehensive comparison of roles in relation to health care administration is thoroughly developed with supporting details.
10.0% Comparison of Roles in Relation to Informatics
A comparison of roles in relation to informatics is not included. A comparison of roles in relation to informatics is present, but it lacks detail or is incomplete. A comparison of roles with regard to informatics is present.
A comparison of roles in relation to informatics is clearly provided and well developed. A comprehensive comparison of roles in relation to informatics is thoroughly developed with supporting details.
10.0% Comparison of Roles in Relation to Business or Finance
A comparison of roles in relation to business or finance is not included. A comparison of roles in relation to business or finance is present, but it lacks detail or is incomplete.
A comparison of roles in relation to business or finance is present. A comparison of roles in relation to business or finance is clearly provided and well-developed. A comprehensive comparison of roles in relation to business or finance is thoroughly developed with supporting details.
5.0% Comparison of Roles in Relation to Specialty
A comparison of roles in relation to specialty is not included. A comparison of roles with regard to specialty is present, but it lacks detail or is incomplete. A comparison of roles in relation to specialty is current.
A comparison of roles in relation to specialty is clearly provided and well developed. A comprehensive comparison of roles in relation to specialty is thoroughly developed with supporting details.
5.0 % Required Sources Sources are not included
The number of required sources is only partially met. Number of sources needed is met, but sources are outdated or inappropriate. Number of required sources is met.
Sources are current, but not all sources are appropriate for the assignment criteria and nursing content Nursing Roles Graphic Organizer Template NUR 513 Week 2. Number of required resources is completed. Sources are current, and appropriate for the assignment criteria and nursing content.
5.0% Visual Appeal There are few or no graphic elements.
No variation in layout or typography is evident. Color is garish or typographic variations are overused and legibility suffers. Background interferes with readability. Understanding of concepts, ideas, and relationships is limited. Minimal use of graphic elements is evident. Elements do not consistently contribute to understanding concepts, ideas, and relationships.
There is some variation in type size, color, and layout. Thematic graphic elements are used but not always in context. Visual connections mostly contribute to understanding concepts, ideas, and relationships. Differences in type size and color are used well and consistently. Appropriate and thematic graphic elements are used to make visual connections that contribute to understanding concepts, ideas, and relationships. Differences in type size and color are used well and consistently.
5.0% Presentation The piece is not neat or organized and does not include all required elements.
The work is not neat and includes minor flaws or omissions of necessary elements.
The overall appearance is general, and major elements are missing Nursing Roles Graphic Organizer Template NUR 513 Week 2. The overall appearance is generally neat, with a few minor flaws or missing elements. The work is well presented and includes all required elements. The overall appearance is neat and professional.
5.0% Mechanics of Writing
(includes spelling, punctuation, grammar, and language use) Surface errors are pervasive enough to impede meaningful communication. Inappropriate word choice or sentence construction is employed.
Frequent and repetitive mechanical errors distract the reader. Inconsistencies in language choice (register) or word choice are present. The sentence structure is correct but not varied.
Some mechanical errors or typos are present, but they are not overly distracting to the reader. Correct and varied sentence structure and audience-appropriate language are employed. Prose is largely free of mechanical errors, although a few may be present. The writer uses a variety of effective sentence structures and figures of speech. The writer is clearly in command of standard, written, academic English.
5.0% Documentation of Sources
(citations, footnotes, references, bibliography, etc., as appropriate to assignment and style) Sources are not documented. Documentation of sources is inconsistent or incorrect, as appropriate to assignment and style, with numerous formatting errors.
Sources are documented, as appropriate to assignment and style, although some formatting errors may be present.
Sources are documented as appropriate to assignment and style, and format is mostly correct. Sources are completely and correctly documented, as appropriate to assignment and style, and format is free of error.
100% Total Weightage
Resources
American Nurses Association
Explore the American Nurses Association (ANA) website.
URL: http://nursingworld.org/
Nursing Overview
Explore the Nursing Overview links on the Explore Health Careers website.
URL: http://explorehealthcareers.org/en/Field/6/Nursing
NUR 513 Topic 2 DQ 1
Identify at least three regulatory bodies or industry regulations that specify certification, licensure requirements, or scope of practice for your specialty. Discuss the way these bodies or regulations influence the educational requirements and experiences for your specialty. Advanced practice registered nurses must incorporate the APRN consensus model in their response.
The Alaska Board of Nurses is a “practice-specific board or commission” of the Alaska Department of Commerce, Community, and Economic Development: Division of Corporations, Business, and Professional Licensing, and both “are government agencies that regulate each profession with the goal of protecting the public” (DeNisco & Barker, 2016, pg 252, para 1).
The Alaska Senate, where legislation becomes law to govern the practice, would be a third regulatory body.
Because of the potential for harm and the intimate nature of nursing care, states are well known for protecting the public by establishing laws to regulate the professions (Russell, 2012). As a result, “laypersons cannot ordinarily judge the competency of a health professional, or whether the care delivered to them meets acceptable and prevailing standards of care” (Russell, 2012).
There is an acute “lack of awareness exists within healthcare services on the differences between the roles of advanced nurse practitioner (ANP) and clinical nurse specialist (CNS)” (Cooper, McDowell & Raeside, 2019, para 1).
For this reason, there remains a level of vagueness with their individual scopes of practice. Both roles are similarly valuable in the effect that they are based in clinical yet include aspects of “education, leadership and research components”, “where “CNS roles are specialist, ANP are more likely to be generalist. (Cooper, McDowell & Raeside, 2019, para 1).
The differences arise “where there is regulation and governance the role of the ANP is clearly defined and structured; however, a lack of governance and regulation is evident in many countries” (Cooper, McDowell & Raeside, 2019, para 1). As a group we need to advocate for better nationwide standardization of these specialties so that we can work to our educational levels.
References:
Cooper, M.A.; McDowell, J. & Raeside, L. (2019) The similarities and differences between advanced nurse practitioners and clinical nurse specialists. British Journal of Medicine 28(20): 1308-1314. DOI: http://dx.doi.org.lopes.idm.oclc.org/10.12968/bjon.2019.28.20.1308
DeNisco, S. & Barker, A. (2016) Advanced Practice Nursing: Essential Knowledge for the Profession. (3rd ed.)Burlington: Jones & Bartlett Learning
Russell, K. A. (2012). Nurse practice acts guide and govern nursing practice. Journal of Nursing Regulation, 3(3), 36–42. Retrieved from: https://www.ncsbn.org/2012_JNR_NPA_Guide.pdf
READ MORE >>
Welcome to the exciting world of nursing education! As you prepare to embark on ...
Welcome to the exciting world of nursing education! As you prepare to embark on your journey at the university’s College of Nursing, it’s important to understand that the new student orientation is mandatory for all incoming nursing students. This article will review what to expect and how to prepare for this crucial introduction to your academic journey.
General Guidelines
Before getting into specific recommendations, there are some general guidelines to keep in mind when planning your orientation outfit:
- Err on the side of being overdressed rather than underdressed. It’s better to look more formal and professional than casual.
- Make sure your clothes are clean, pressed, and in good condition. Avoid garments with rips, stains, excessive wrinkles, or other signs of wear and tear.
- Choose clothes that fit well. Avoid anything too tight or overly loose/baggy. You want to look polished and put together.
- Go for a more conservative, understated look. Avoid anything too flashy, revealing, or distracting, such as plunging necklines, short skirts, or loud prints and colors.
- Make sure you will be comfortable sitting and walking around campus for an extended period in your clothes and shoes. You don’t want to be distracted by physical discomfort.
Now let’s get into more detailed outfit recommendations:
What Tops to Wear
A good top selection rule is a classic, professional look. Here are some top options that are perfect for orientation:
- Button-down Shirts: A crisp, button-down collared shirt in a neutral color like white, light blue, or pale pink is always a safe bet. Make sure it is pressed and fits well through the shoulders and sleeves. Avoid any gaping between the buttons.
- Blouses: A nice blouse can also work well for orientation. Choose one in a solid, neutral color, or a subtle print. Make sure it is not too low-cut or sheer. A silky material can elevate a blouse, but avoid anything too clingy.
- Cardigans/Sweaters: Layering a cardigan or pullover sweater over a shirt or blouse is a great option, especially if orientation is in an air-conditioned building or occurs in cooler months. Go for a solid, neutral color like black, gray, or navy.
- Polo Shirts: A neutral-colored polo shirt can work if your orientation is more casual or takes place in a warm location. Make sure it fits well and is not too tight or baggy.
Whatever style you choose, make sure it covers your shoulders and midriff and hits around your hips. Avoid cropped, sleeveless (unless layered), or graphic tees with slogans or busy images.
What Bottoms to Wear
When it comes to pants or skirts, here are some guidelines:
- Pants: Dress pants, khakis, or neutral-colored slacks are all appropriate for orientation. Choose a fabric with some structure, like cotton, wool, or a blend. Avoid denim, leggings, joggers, or overly tight fits. Make sure the pants are hemmed properly and not dragging on the ground.
- Skirts: If you opt for a skirt, go for a knee-length or slightly below the knee. An A-line or pencil skirt can work well. Avoid anything too short, tight, or flowy. Stick with neutral, solid colors like black, gray, or navy.
- Dresses: A professional dress can also be a great choice for orientation. Choose one that is around knee-length with a higher neckline. A sheath or shirt dress style can work well. Avoid sundresses, strapless styles, or overly formal dresses. Stick with solid, neutral colors.
Whichever bottom you choose, make sure it fits well, isn’t see-through, and that you can comfortably sit and move around in it. Avoid shorts, capris, or anything overly trendy or distracting. Combine your bottom with your chosen top, and ensure the combination looks polished and professional.
Footwear
When it comes to shoes, prioritize comfort and professionalism. You’ll likely be walking around campus for a fair time during orientation. Avoid open-toed shoes, casual styles like flip flops or sneakers, or shoes with high heels. Here are some good options:
- Flats: Simple, closed-toe flats in a neutral color like black or beige are a great, comfortable choice. Make sure they have some cushioning and traction.
- Low Heels: If you prefer a shoe with a heel, stick with something around 2 inches or lower. A low pump or heel in black or nude can work well. Make sure you can walk comfortably in them.
- Loafers: A loafer-style flat can also be used for orientation and provides more structure and support than a ballet flat. Go for a neutral color.
Avoid scuffed, worn-out shoes, distracting colors, or hard-to-walk-in shoes. If you wear pants, your socks should be solid and dark. If you’re wearing a skirt, consider nude hosiery or trouser socks.
Accessories
Keep accessories simple and professional for orientation. Here are some guidelines:
- Jewelry: Choose simple, classic pieces, such as stud earrings, a delicate necklace, or a simple bracelet. Avoid anything overly flashy, jangly, or distracting.
- Watch: A professional watch with a metal or leather band can be a nice accessory for tracking time during orientation. Avoid digital or sporty styles.
- Bag: Bring a large bag to hold essentials like your wallet, keys, phone, notebook and pen, and orientation materials. A structured shoulder bag, tote, or messenger bag can work well. Avoid overly large bags, casual styles like backpacks, or evening bags.
Keep any makeup natural and understated. Keep your hair neat and styled to keep it out of your face. Avoid strong perfumes or scents. If you wear nail polish, ensure it is conservative and not chipped.
Other Considerations
In addition to the clothing elements, here are a few other things to consider for orientation day:
- Dress in Layers: Layers will allow you to adjust if orientation spaces are hot or cold. A cardigan, pullover sweater, or blazer are all good options to put on or take off easily.
- Check Orientation Information for Any Requirements: Read any orientation information thoroughly in case any specific clothing requirements are outlined. Some schools require students to wear their nursing uniform or lab coat at orientation.
- Bring a Small Umbrella: If there is any chance of rain on orientation day, bring a compact umbrella in case you have to walk between buildings.
- Wear Deodorant/Antiperspirant: You’ll meet many new people at orientation, so wear deodorant or antiperspirant to control sweat and avoid body odor.
- Bring Breath Mints or Gum: Similarly, you’ll be doing a lot of talking during orientation, so you may want to bring breath mints or gum to freshen your breath throughout the day.
- Comfortable Undergarments: Wear comfortable undergarments that don’t show lines under your clothes and that you can wear all day without being uncomfortable or self-conscious.
- Get a Good Night’s Sleep: Get a restful night’s sleep before orientation so that you are alert, energized, and focused during the day’s events. Being well-rested will help you make the best impression.
Outfit Examples
To put this advice together, here are some sample outfit combinations that would work well for nursing school orientation:
- White button-down shirt + black slacks + black flats + simple stud earrings + black tote bag
- Light blue blouse + gray pencil skirt + gray low heels + delicate silver necklace + nude hosiery + gray shoulder bag
- Beige sweater + navy dress pants + navy loafers + simple watch + navy messenger bag
- Pale pink polo shirt + khaki pants + brown flats + small gold hoop earrings + brown leather tote
- Navy sheath dress + black low heels + simple bracelet + black structured shoulder bag
Use the guidelines to create an outfit that makes you feel confident, comfortable, and professional.
Can You Wear Scrubs to Nursing School Orientation?
Some nursing programs may specifically require or encourage students to wear scrubs to orientation. They may want to familiarize students with the dress code from the start or take pictures of the incoming class in their scrubs. If your school has provided such instructions, follow them.
However, nursing schools do not typically require students to wear scrubs to orientation. Orientation is usually a more formal event where business casual attire is more appropriate. Scrubs are work attire for clinical settings, and orientation is not typically a clinical event.
If your school hasn’t provided specific guidance, avoiding being slightly overdressed rather than underdressed for orientation is generally better. Professional business casual attire like slacks or a skirt with a button-down shirt or blouse is a safe choice. It shows that you are taking your nursing education and profession seriously.
Closing Thoughts
While the first week of nursing school can feel stressful, remember that orientation is designed to help you transition smoothly into your new role as a nursing student. The faculty and staff are there to support you and want you to succeed. This is the first step in what will be a challenging but rewarding educational journey.
We look forward to welcoming you to our nursing program. If you have any questions before orientation, please contact the Office of Student Affairs. Good luck, and we can’t wait to meet our incoming nursing students.on the right foot with a great first impression will set you up for success in nursing school and beyond.
READ MORE >>
While an old DUI may not automatically disqualify you from getting into nursing ...
While an old DUI may not automatically disqualify you from getting into nursing school, the impact on your nursing school prospects can vary depending on:
- The severity and circumstances of the offense
- The length of time since the conviction
- The policies of the specific nursing schools and programs you are considering
- The state in which you are seeking licensure and employment
Some nursing schools may have stricter policies regarding criminal backgrounds, while others may be more open to considering applicants with a DUI on a case-by-case basis.
Research the schools’ policies you are interested in and be transparent about your situation when applying. In some cases, exploring legal options, such as having the DUI expunged from your record, might be feasible, potentially improving your chances of being accepted into a nursing program.
How to Get into Nursing School with a DUI
If you have a DUI on your record and are determined to pursue a nursing education, there are several steps you can take to improve your chances of admission:
- Address any substance abuse issues: If your DUI was related to alcohol or drug abuse, it is essential to demonstrate that you have taken steps to address and overcome these issues. This may include completing a substance abuse treatment program, attending support groups, and maintaining sobriety.
- Be honest and proactive in your application: When applying to nursing schools, be upfront about your DUI and provide a clear, concise explanation of the circumstances, what you have learned from the experience, and how you have grown and changed since then. Demonstrating accountability, remorse, and personal growth can work in your favor.
- Emphasize your strengths and qualifications: While your DUI may concern some schools, it is important to highlight your academic achievements, relevant experience, and personal qualities that make you a strong candidate for nursing school. Focus on your passion for nursing, your commitment to helping others, and any volunteer or healthcare-related experience you have.
- Provide strong references and recommendations: Secure recommendations from professionals, such as professors, employers, or volunteer supervisors, who can speak to your character, work ethic, and suitability for the nursing profession. These endorsements can help counterbalance any concerns raised by your DUI.
- Consider alternative paths: If you face challenges getting into traditional nursing programs due to your DUI, explore alternative options such as community college programs, vocational schools, or online programs that may have more flexible admission policies. These can serve as stepping stones to further education and career advancement.
How a DUI Affects Future Nursing Jobs
While getting into nursing school with a DUI is possible, it is important to understand that a criminal record can also impact your future employment prospects as a nurse. Many healthcare employers conduct background checks and may have policies against hiring individuals with certain convictions, including DUIs.
However, the extent to which a DUI affects your nursing career can vary depending on factors such as:
- The nature and severity of the offense
- The length of time since the conviction
- The specific policies of the employer or healthcare facility
- The state in which you are seeking licensure and employment
Some states have more stringent regulations regarding criminal backgrounds for healthcare professionals, while others may consider individual cases. It is essential to research the policies of the state board of nursing and potential employers in your area to understand their stance on DUIs and other criminal convictions.
In some cases, nurses with a DUI may face restrictions on their practice, such as being prohibited from administering certain medications or working in specific settings like home health or hospice care. It is crucial to be transparent with potential employers about your background and work with them to determine any necessary accommodations or limitations.
How a DUI Affects Taking the NCLEX Exam
To become a licensed nurse, you must pass the National Council Licensure Examination (NCLEX). While a DUI does not automatically disqualify you from taking the NCLEX, it can complicate the process and raise concerns with the state board of nursing.
When applying for licensure, you must typically disclose any criminal convictions, including DUIs. The state board of nursing will review your case to determine your eligibility to take the NCLEX and become licensed. Factors they may consider include:
- The nature and severity of the offense
- The length of time since the conviction
- Any evidence of rehabilitation and personal growth
- Your overall moral character and fitness to practice nursing
Sometimes, the board may request additional information, documentation, or a personal interview to assess your situation. They may also impose conditions on your licensure, such as requiring you to complete a substance abuse treatment program or submit to random drug testing.
It is essential to proactively address any concerns the board may have and demonstrate your commitment to personal and professional integrity. Consulting with a legal professional experienced in nursing licensure issues can also help you navigate the process and protect your rights.
Getting a DUI When you are a Nurse
If you are already a practicing nurse and receive a DUI conviction, the consequences can be more severe and immediate. Nurses are held to high ethical and professional standards, and a DUI can be seen as a violation of the trust placed in them by patients, employers, and the public.
The specific consequences of a DUI for a practicing nurse can vary depending on factors such as:
- The severity and circumstances of the offense
- The policies of your employer and the healthcare facility where you work
- The regulations of the state Board of Nursing
In many cases, nurses must self-report criminal convictions, including DUIs, to their employer and the state board of nursing within a certain timeframe. Failure to do so can result in additional disciplinary action.
Consequences of a DUI for a practicing nurse may include:
- Suspension or revocation of your nursing license
- Termination of employment
- Mandatory substance abuse treatment or monitoring programs
- Restrictions on your scope of practice or the settings in which you can work
- Damage to your professional reputation and future employment prospects
It is crucial for nurses who receive a DUI to take immediate steps to address the situation, such as seeking legal counsel, notifying the appropriate parties, and proactively engaging in any required interventions or rehabilitation programs. Demonstrating accountability, remorse, and a commitment to personal and professional growth can mitigate the long-term consequences of a DUI on your nursing career.
Worst Case Scenario For Nurses Who’ve Had a DUI
In the worst-case scenario, a DUI conviction can lead to the loss of your nursing license and the end of your nursing career. This is more likely to occur in cases involving severe aggravating factors, such as:
- Multiple DUI offenses
- DUI resulting in injury or death to others
- DUI while on duty or in a healthcare setting
- Refusal to comply with substance abuse treatment or monitoring requirements
- Other serious ethical or professional violations in addition to the DUI
Losing your nursing license due to a DUI can have devastating personal and professional consequences. It can result in the loss of your livelihood, financial instability, and damage to your reputation and future prospects in the healthcare field.
In some cases, nurses who have lost their licenses due to a DUI may have the opportunity to petition for reinstatement after a certain period and upon meeting specific requirements, such as completing a substance abuse treatment program and demonstrating a sustained period of sobriety and rehabilitation. However, the reinstatement process can be lengthy, complex, and uncertain without guaranteeing success.
The best approach for nurses is to prioritize prevention and avoid any behavior that could lead to a DUI in the first place. This includes:
- Never driving under the influence of alcohol or drugs
- Using designated drivers, taxis, or ride-sharing services when drinking
- Seeking help for any substance abuse or mental health issues that may contribute to risky behavior
- Maintaining high standards of personal and professional conduct at all times
By making responsible choices and upholding the ethical and professional standards of the nursing profession, you can protect your nursing career and your ability to make a positive difference in the lives of your patients.
Does DUI affect medical school admission?
Yes, a DUI (Driving Under the Influence) can affect medical school admission. Medical schools look for students with strong ethics and responsibility, so a DUI may raise concerns about your judgment and behavior. However, it doesn’t automatically disqualify you. Schools will likely consider the circumstances, how you’ve handled the situation, and whether you’ve shown growth or taken responsibility. Being honest about it in your application and explaining how you’ve learned from the experience can help your chances.
READ MORE >>
Nursing-Sensitive Indicators Assignment 12Nursing-Sensitive Indicators Assignmen ...
Nursing-Sensitive Indicators Assignment 12
Nursing-Sensitive Indicators Assignment 12
To prepare for this week’s discussion, read this article on nursing-sensitive value-based reimbursement by Cleveland, Motter, and Smith (2019). In your discussion response, please address each of the following:
(To access the article, click the URL: https://ojin.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Vol-24-2019/No2-May-2019/Affordable-Care.html)
- Explain how health care provider reimbursement is related to nursing-sensitive indicators.
- Describe how you observe your organization addressing nursing-sensitive indicators.
Please be sure to support your discussion with a scholarly source. Please also respond to at least two peers this week to achieve full participation points.
This activity aligns with:
- Course Outcome ? 1. Describe the impact of healthcare policies on nursing practice and healthcare work environments to determine the financial and regulatory influences on patient care.
- AACN BSN Essential V.1: Demonstrate basic knowledge of healthcare policy, finance, and regulatory environments, including local, state, national, and global healthcare trends.
- AACN BSN Essential V. 5: Describe state and national statutes, rules, and regulations that authorize and define professional nursing practice.
ORDER THROUGH BOUTESSAY
Nursing-Sensitive Indicators Assignment 12 Instructions
Read over your paper – in silence and then aloud – before handing it in and make corrections as necessary. Often it is advantageous to have a friend proofread your paper for obvious errors. Handwritten corrections are preferable to uncorrected mistakes.
Use a standard 10 to 12 point (10 to 12 characters per inch) typeface. Smaller or compressed type and papers with small margins or single-spacing are hard to read. It is better to let your essay run over the recommended number of pages than to try to compress it into fewer pages.
Likewise, large type, large margins, large indentations, triple-spacing, increased leading (space between lines), increased kerning (space between letters), and any other such attempts at “padding” to increase the length of a paper are unacceptable, wasteful of trees, and will not fool your professor.
The paper must be neatly formatted, double-spaced with a one-inch margin on the top, bottom, and sides of each page. When submitting hard copy, be sure to use white paper and print out using dark ink. If it is hard to read your essay, it will also be hard to follow your argument.
ADDITIONAL INSTRUCTIONS FOR THE CLASS
Discussion Questions (DQ)
- Initial responses to the DQ should address all components of the questions asked, include a minimum of one scholarly source, and be at least 250 words.
- Successful responses are substantive (i.e., add something new to the discussion, engage others in the discussion, well-developed idea) and include at least one scholarly source.
- One or two sentence responses, simple statements of agreement or “good post,” and responses that are off-topic will not count as substantive. Substantive responses should be at least 150 words.
- I encourage you to incorporate the readings from the week (as applicable) into your responses.
Weekly Participation
- Your initial responses to the mandatory DQ do not count toward participation and are graded separately.
- In addition to the DQ responses, you must post at least one reply to peers (or me) on three separate days, for a total of three replies.
- Participation posts do not require a scholarly source/citation (unless you cite someone else’s work).
- Part of your weekly participation includes viewing the weekly announcement and attesting to watching it in the comments. These announcements are made to ensure you understand everything that is due during the week.
APA Format and Writing Quality
- Familiarize yourself with APA format and practice using it correctly. It is used for most writing assignments for your degree. Visit the Writing Center in the Student Success Center, under the
- Resources tab in LoudCloud for APA paper templates, citation examples, tips, etc. Points will be deducted for poor use of APA format or absence of APA format (if required).
- Cite all sources of information! When in doubt, cite the source. Paraphrasing also requires a citation.
- I highly recommend using the APA Publication Manual, 6th edition.
Use of Direct Quotes
- I discourage overutilization of direct quotes in DQs and assignments at the Masters’ level and deduct points accordingly.
- As Masters’ level students, it is important that you be able to critically analyze and interpret information from journal articles and other resources. Simply restating someone else’s words does not demonstrate an understanding of the content or critical analysis of the content.
- It is best to paraphrase content and cite your source.
LopesWrite Policy
- For assignments that need to be submitted to LopesWrite, please be sure you have received your report and Similarity Index (SI) percentage BEFORE you do a “final submit” to me.
- Once you have received your report, please review it. This report will show you grammatical, punctuation, and spelling errors that can easily be fixed. Take the extra few minutes to review instead of getting counted off for these mistakes.
- Review your similarities. Did you forget to cite something? Did you not paraphrase well enough? Is your paper made up of someone else’s thoughts more than your own?
- Visit the Writing Center in the Student Success Center, under the Resources tab in LoudCloud for tips on improving your paper and SI score.
Late Policy
- The university’s policy on late assignments is 10% penalty PER DAY LATE. This also applies to late DQ replies.
- Please communicate with me if you anticipate having to submit an assignment late. I am happy to be flexible, with advance notice. We may be able to work out an extension based on extenuating circumstances.
- If you do not communicate with me before submitting an assignment late, the GCU late policy will be in effect.
- I do not accept assignments that are two or more weeks late unless we have worked out an extension.
- As per policy, no assignments are accepted after the last day of class. Any assignment submitted after midnight on the last day of class will not be accepted for grading.
Communication
Communication is so very important. There are multiple ways to communicate with me:
- Questions to Instructor Forum: This is a great place to ask course content or assignment questions. If you have a question, there is a good chance one of your peers does as well. This is a public forum for the class.
- Individual Forum: This is a private forum to ask me questions or send me messages. This will be checked at least once every 24 hours.
READ MORE >>
Nursing Sensitive Quality Indicators Sample PaperIntroductionNursing Sensitive Q ...
Nursing Sensitive Quality Indicators Sample Paper
Introduction
Nursing Sensitive Quality Indicators (NSQI) describe the key values and elements used to measure the impact and the contribution of nurses on patients’ health outcomes. Today, patient satisfaction is a critical factor in assessing patient outcomes. The American Nurses Association has identified about ten critical NSQIs that are used in acute care settings. The quality indicator that I have chosen to discuss is patient satisfaction with pain management.
Patient Satisfaction with Pain Management.
One of the most critical issues for patients is managing pain. Consequently, pain management has become an essential measurement tool for patient satisfaction. Being a subjective issue, healthcare facilities are judged by how satisfied patients are in terms of pain management. In acute settings, healthcare facilities employ numerous ways of managing pain such as using opioids. The use of opioids in chronic pain management, according to Miclette et al., (2018), elicits mixed reactions among those who support its use and those who oppose it.
He same applies to other drugs and substances used in pain management, such as medicinal marijuana. One of the most advanced theories that have been used to explain as well as provide an effective framework for pain management is the Brain Theory of Social Attachment, BOTSA. This theory provides that managing physical and emotional pain can be achieved by managing social connections, and subjective experiences of patients within the healthcare setting.
For instance, the dilemma that exists for patients who use marijuana medicinally is that in as much as half of the States in America have legalized the use of marijuana medicinally even with the doctor’s approval, the United States Code section 844 expressly outlines that possession of a controlled substance of any amount is a crime (Dougherty et al, 2013, P. 207). Therefore, in as much as State Laws permit the use of marijuana for medicinal purposes, it is still possible for one to get prosecuted criminally under Federal laws.
The Federal Government, through its many Federal agencies particularly the Drug enforcement Administration DEA, has made their intentions clear to stop the distribution of medical marijuana through strict enforcement of Federal drug laws. The DEA argues that there is no binding consensus in medicine that marijuana really helps patients. In 1970, the Congress enacted laws prohibiting the use of marijuana based on this argument that the drug has no proven medical effect or value.
According to Inagaki (2018), BOTSA theory holds that strong social connections or attachments can lead to reduced pain in patients. This means that patients or people under opioid treatment are encouraged to always be in the presence of friends or loved ones rather than live in separation (Scarborough & Smith, 2018). Staying in isolation increases the urge in patients to use more opioids as a way of responding to social stressors. Thus, Brain Theory of Social Attachment asserts that social connection is related to wellbeing.
The Brain Theory of Social Attachment provides a clear framework for the treatment of opioid addiction. In this case, the issue of stopping opioid addiction is dependent on the allegiances or strong bonds formed by addicts (Inagaki, 2017, p. 4). However, this process would require an effective grieving and or mourning process such as losing a loved one. The social connection process is considered therapeutic and can help in the healing process among opioid addicts. However, this theory works on the assumption that for every addict, there will be a sufficient grieving process that may never occur (p. 149). On the other hand, even without the grieving process, the strong connections and bonds formed by addicts and their loved ones may be sufficient to control their opioid intake.
Importance of Pain Management in Patient satisfaction
Nurses must have an ethical responsibility for pain management to reduce patient suffering. If not managed well, pain adversely affects patients psychologically and physically. Based on this analogy, nurses must bear the responsibility of helping patients to find relief from their pain. Apart from physical pain, other adverse effects of pain in patients include depression and anxiety. Poor pain management by nurses have numerous adverse effects for both patients and healthcare facilities, hence the need for pragmatic interventions.
Poor pain management may put nurses/physicians at the risk of legal suits. The joint Commission on Accreditation of Healthcare Organizations (JCAHO) clearly stipulates that pain in patients must be managed and addressed promptly. Poor pain management may make patients to perceive it as neglect (Bonnie et al., 2019). The fact that there are set standards for pain management make hospitals more vulnerable to lawsuits from patients. It is the responsibility of healthcare facilities to have in place effective mechanisms for pain management.
Poor pain management may result in poor reputation for hospitals. Patient satisfaction is directly tied to their experiences with pain. Higher levels of pain is often associated with poor patient satisfaction. When a healthcare facility fails to effectively manage pain in patients, the facility quickly loses reputation as many patients begin to avoid it (Wood, Simel, & Klimas, 2019). The reputation of a hospital is based on the experiences of patients during their stay. Proper pain management boosts customer satisfaction which also directly affects profits and reputation.
Cheatle (2015), after a critical assessment of pain management, asserts the need to maintain the rights of patients receiving pain management by the use of relevant mechanisms (P.6). Cheatle further asserts that patients with acute pain should not be denied access to opioids based on the fears about risks of addiction. According to Cheatle, administering opioids to patients should be accompanied by therapeutic management to help reduce addiction to opioids. The shortcoming with Cheatle’s assertion is that he advocates for the continued use of opioids while completely ignoring the issue of dependency, neither does he provide a way out for a safe and effective alternative.
According to Bolliger and Stevens (2019), there is a need to recognize that dependency on opioids is a serious health hazard that practitioners ought not to ignore. Citing a study by WHO on efforts to reduce opioid addiction, Bolliger and Stevens assert that the more a person is on opioids, the higher the chances of becoming dependent on the drug, a factor that should not be taken for granted if the millions of Americans currently addicted to the drug is anything to go by.
Conclusion
Pain management is a critical tool in measuring patient satisfaction. Nurses/physicians have a duty to help in pain management for patients. There are different techniques that healthcare facilities can employ in patient pain management. One of the best but controversial methods of pain management is using opioids or medical marijuana. Yet, since patient satisfaction is directly tied to their experiences with pain, higher levels of pain is often associated with poor patient satisfaction. When a healthcare facility fails to effectively manage pain in patients, the facility quickly loses reputation as many patients begin to question their approach to pain management.
References
- Bonnie, R. J., Schumacher, M. A., Clark, J. D., & Kesselheim, A. S. (2019). Pain Management and Opioid Regulation: Continuing Public Health Challenges. American Journal of Public Health, 109(1), 31–34. doi: 10.2105/ajph.2018.304881
- Miclette, M. A., Leff, J. A., Cuan, I., Samet, J. H., Saloner, B., Mendell, G., Bao, Y., Ashburn, M. A., Bachhuber, M. A., Schackman, B. R., Polsky, D. E., & Meisel, Z. F. (2018). Closing the gaps in opioid use disorder research, policy and practice: conference proceedings. Addiction Science & Clinical Practice, 13(1). doi: 10.1186/s13722-018-0123
- Wood, E., Simel, D. L., & Klimas, J. (2019). Pain Management With Opioids in 2019-2020. JAMA, 1. doi: 10.1001/jama.2019.15802
- Scarborough, B. M., & Smith, C. B. (2018). Optimal pain management for patients with cancer in the modern era. CA: A Cancer Journal For Clinicians, 68(3), 182-196. https://doi.org/10.3322/caac.21453
READ MORE >>
Laughter is the best medicine, and as a nursing student, you’ll need plenty of ...
Laughter is the best medicine, and as a nursing student, you’ll need plenty of it to get through the rigorous coursework and clinical rotations. To help you stay motivated and keep a positive outlook, we’ve compiled a list of funny quotes that will make you laugh, inspire you, and remind you of the importance of your chosen career path.
- “I’m not saying nursing school is easy. It’s like trying to eat an elephant while unicycling on a tightrope.”
- “Nursing school: where coffee is a food group and sleep is a luxury.”
- “I traded my social life for a stethoscope and a mountain of textbooks. No regrets!”
- “Nursing school is like a box of chocolates. You never know what you’re going to get, but it’s guaranteed to be stressful.”
- “I’m not a morning person, but nursing school has taught me that 5 AM is just a suggestion.”
- “Nursing school: where you learn to speak in acronyms and measure liquids in mL.”
- “I’m pretty sure my blood type is now caffeine positive.”
- “Nursing school is like a never-ending game of ‘What’s that body fluid?'”
- “I’m not saying nursing students are competitive, but I once saw two of them fighting over a vein.”
- “Nursing school: where you learn to appreciate the little things, like a bathroom break and a full night’s sleep.”
How Laughing Improves Mental Health
As a nursing student, you’re under much stress, and finding healthy ways to cope is essential. Laughter is one of the best ways to reduce stress, improve mood, and boost overall mental health. Here are some benefits of laughter:
- Reduces stress hormones
- Increases endorphins (natural painkillers)
- Improves heart health
- Boosts immune system
- Enhances resilience
- Strengthens relationships
- Promotes creativity and problem-solving
- Provides a temporary escape from reality
- Increases overall sense of well-being
- Helps you maintain a positive outlook
Funny Quotes for Nursing Students
Nursing school can be overwhelming at times, but these funny quotes will remind you that you’re not alone in your struggles:
- “Nursing school: where you learn to survive on caffeine, dry shampoo, and pure adrenaline.”
- “I’m not saying nursing school is hard, but I once saw a textbook make a grown man cry.”
- “Nursing school is like a marathon, except instead of water stations, there are coffee stations, and instead of a finish line, there’s the NCLEX.”
- “I’m pretty sure my nursing school motto is ‘Sleep, study, repeat.'”
- “Nursing school: where you learn to function on minimal sleep and maximum stress.”
- “I’m not saying nursing students are busy, but I once saw one trying to eat, study, and do CPR at the same time.”
- “Nursing school is like a rollercoaster ride. It has its ups and downs, but in the end, it’s totally worth it.”
- “I’m pretty sure my blood type is now ‘textbook and tears.'”
- “Nursing school: where you learn to appreciate the value of a good pair of compression socks.”
- “I’m not saying nursing school is stressful, but I once saw a student use their stethoscope as a stress ball.”
Funny Nursing Student Life Quotes
Life as a nursing student can be hectic, but these funny quotes will remind you to find humor in the chaos:
- “I’m not saying nursing students are obsessed with hand sanitizer, but I once saw one use it as perfume.”
- “Nursing school: where your social life consists of study groups and clinical rotations.”
- “I’m pretty sure my wardrobe now consists entirely of scrubs and compression socks.”
- “Nursing school is like a reality TV show. There’s drama, tears, and the occasional mental breakdown.”
- “I’m not saying nursing students are competitive, but I once saw two of them race to put on sterile gloves.”
- “Nursing school: where you learn to appreciate the value of a good pair of shoes and a strong bladder.”
- “I’m pretty sure my mom thinks I’m dead because I haven’t called her in weeks. Thanks, nursing school.”
- “Nursing school is like a never-ending game of ‘How many cups of coffee can I drink before my heart explodes?'”
- “I’m not saying nursing students are paranoid, but I once saw one try to take their own blood pressure during a test.”
- “Nursing school: where you learn to appreciate the little things, like a moment of silence and a clean pair of scrubs.”
Inspirational Nursing School Quotes
When the going gets tough, these inspirational quotes will remind you of why you chose to pursue a career in nursing:
- “Nurses dispense comfort, compassion, and caring without even a prescription.” – Val Saintsbury
- “Nursing is not for everyone. It takes a very strong, intelligent, and compassionate person to take on the ills of the world with passion and purpose and work to maintain the health and well-being of the planet. No wonder we’re exhausted at the end of the day!” – Donna Wilk Cardillo
- “The character of the nurse is as important as the knowledge she possesses.” – Carolyn Jarvis
- “Nurses are the heart of healthcare.” – Donna Wilk Cardillo
- “Nursing is one of the fine arts: I had almost said, the finest of fine arts.” – Florence Nightingale
- “Nursing is not a profession; it’s a calling. You don’t become a nurse because you want to, you become a nurse because you have to.” – Unknown
- “Nurses are the hospitality of the hospital.” – Carrie Latet
- “Nurses are angels in comfortable shoes.” – Unknown
- “Nursing is an art: and if it is to be made an art, it requires an exclusive devotion as hard a preparation as any painter’s or sculptor’s work.” – Florence Nightingale
- “Nurses are the backbone of the healthcare system.” – Unknown
Motivational Quotes For Nurses
When you need a little extra motivation, these quotes will remind you of the importance of your work as a nursing student:
- “Hardships often prepare ordinary people for an extraordinary destiny.” – C.S. Lewis
- “The only way to do great work is to love what you do.” – Steve Jobs
- “Believe you can and you’re halfway there.” – Theodore Roosevelt
- “Success is not final, failure is not fatal: it is the courage to continue that counts.” – Winston Churchill
- “The future belongs to those who believe in the beauty of their dreams.” – Eleanor Roosevelt
- “The best way to predict the future is to create it.” – Abraham Lincoln
- “Strive not to be a success, but rather to be of value.” – Albert Einstein
- “You miss 100% of the shots you don’t take.” – Wayne Gretzky
- “The only limit to our realization of tomorrow will be our doubts of today.” – Franklin D. Roosevelt
- “The greatest glory in living lies not in never falling, but in rising every time we fall.” – Nelson Mandela
Short Funny Nursing Student Quotes
When you need a quick laugh, these short and sweet quotes will do the trick:
- “I’m not a doctor, but I play one in clinicals.”
- “Nursing school: where caffeine is a food group.”
- “I’m a nurse. What’s your superpower?”
- “Nursing school: where ‘free time’ is just a myth.”
- “I can’t brain today. I have the dumb.”
- “Nursing school: where procrastination meets panic.”
- “I’m not bossy. I just have better ideas.”
- “I’m a nurse. I stop when I’m done, not when I’m tired.”
- “Nursing school: where ‘all-nighter’ is a verb.”
- “I’m not lazy. I’m on energy-saving mode.”
Workplace Funny Nurse Quotes
As a nursing student, you’ll spend plenty of time in clinical rotations. These funny quotes will help you find humor in the workplace:
- “I’m not arguing. I’m just explaining why I’m right.”
- “I’m a nurse. What’s your excuse?”
- “I’m not ignoring you. I’m just focusing on my patient.”
- “I’m not lazy. I’m just on my mandatory break.”
- “I’m a nurse. I know how to multitask. I can talk, annoy, and aggravate you all at the same time.”
- “I’m not bossy. I just have a strong leadership style.”
- “I’m a nurse. I have a PhD in patience.”
- “I’m not a morning person. I’m a coffee person.”
- “I’m a nurse. I have a license to heal.”
- “I’m not short. I’m just vertically challenged.”
Funny Nursing Friend Quotes
Nursing school is better with friends by your side. These funny quotes celebrate the bond between nursing students:
- “Friends don’t let friends go through nursing school alone.”
- “I’m not saying we’re codependent, but I once saw two nursing students share a stethoscope.”
- “Nursing school: where your squad goals include passing the NCLEX.”
- “I’m not saying we’re attached at the hip, but I once saw two nursing students share a pair of compression socks.”
- “Nursing school: where your BFF is also your study buddy.”
- “I’m not saying we’re inseparable, but I once saw two nursing students share a blood pressure cuff.”
- “Nursing school: where your social life consists of study sessions and group projects.”
- “I’m not saying we’re joined at the hip, but I once saw two nursing students share a pen light.”
- “Nursing school: where your friendship is measured in cups of coffee and late-night study sessions.”
- “I’m not saying we’re a package deal, but I once saw two nursing students share a name badge.”
Relatable Nursing Student Funny Quotes
As a nursing student, you’ll encounter many situations that are both challenging and humorous. These relatable quotes will make you laugh and remind you that you’re not alone:
- “I’m not saying I’m sleep-deprived, but I once tried to take my patient’s temperature with a stethoscope.”
- “Nursing school: where you learn to appreciate the value of a good pair of compression socks and a strong cup of coffee.”
- “I’m not saying I’m forgetful, but I once tried to start an IV on a mannequin.”
- “Nursing school: where you learn to speak in medical jargon and measure liquids in mL.”
- “I’m not saying I’m clumsy, but I once tripped over my own stethoscope.”
- “Nursing school: where you learn to appreciate the value of a good pair of shoes and a quick bathroom break.”
- “I’m not saying I’m accident-prone, but I once spilled a bedpan on my scrubs.”
- “Nursing school: where you learn to function on minimal sleep and maximum caffeine.”
- “I’m not saying I’m a germaphobe, but I once used an entire bottle of hand sanitizer in one shift.”
- “Nursing school: where you learn to appreciate the value of a good sense of humor and a supportive group of friends.”
Nursing Jokes
Sometimes, a good joke is all you need to brighten your day. These nursing jokes will make you chuckle:
- “Why did the nurse bring a red pen to work? In case she needed to draw blood!”
- “What do you call a nurse who always works with a smile? A patient care technician!”
- “Why did the nurse always carry a pencil? Because it was pointless!”
- “What do you call a nurse who loves to garden? A plant care technician!”
- “Why did the nurse always carry a calculator? Because she needed to count on it!”
- “What do you call a nurse who loves to sing? A patient serenader!”
- “Why did the nurse always wear a watch? Because she needed to keep an eye on the time!”
- “What do you call a nurse who loves to dance? A patient entertainer!”
- “Why did the nurse always carry a compass? Because she needed to find her way around the hospital!”
- “What do you call a nurse who loves to tell jokes? A patient comedian!”
Inspirational Nursing Student Quotes
As a nursing student, you have the power to make a difference in people’s lives. These inspirational quotes will remind you of the importance of your work:
- “Nursing is not just a job; it’s a calling. It’s a commitment to helping others, even when it’s hard.”
- “As a nursing student, you have the opportunity to touch lives and make a difference in the world.”
- “Nursing is a work of heart. It takes compassion, dedication, and a willingness to put others first.”
- “Nursing is not for the faint of heart. It takes strength, courage, and a passion for helping others.”
- “As a nursing student, you are the future of healthcare. Your hard work and dedication will make a difference in countless lives.”
- “Nursing is a privilege. It’s an opportunity to be there for people during their most vulnerable moments.”
- “As a nursing student, you have the power to bring comfort, healing, and hope to those in need.”
- “Nursing is a profession that requires both skill and heart. It’s a calling to serve others with compassion and care.”
- “As a nursing student, you are part of a noble profession. Your work will touch lives and make a lasting impact.”
- “Nursing is a journey of growth, learning, and service. Embrace the challenges and opportunities that come your way.”
Funny Nursing Graduation Quotes
Graduating from nursing school is a major accomplishment. These funny quotes will help you celebrate your achievement with humor:
- “I’m not saying I’m excited to graduate, but I once tried to frame my diploma before I even received it.”
- “Nursing school: where your graduation gown doubles as a superhero cape.”
- “I’m not saying I’m relieved to be done with nursing school, but I once hugged my diploma like it was a long-lost friend.”
- “Nursing school: where your graduation cap doubles as a crown of achievement.”
- “I’m not saying I’m proud of myself, but I once tried to wear my nursing badge to bed.”
- “Nursing school: where your graduation party doubles as a celebration of survival.”
- “I’m not saying I’m ready to take on the world, but I once tried to start an IV on a celebratory champagne bottle.”
- “Nursing school: where your graduation photos double as evidence of your perseverance.”
- “I’m not saying I’m a big deal, but I once tried to sign autographs on my nursing textbooks.”
- “Nursing school: where your graduation speech doubles as a thank-you note to caffeine.”
This article’s funny quotes, jokes, and inspirational messages remind you that laughter and positivity can help you through the toughest times. Remember that your work as a nursing student and future nurse is invaluable. You have the power to make a difference in people’s lives, to bring comfort and healing to those in need, and to be a beacon of hope in a world that often feels uncertain.
READ MORE >>
Preceptorship is a crucial component of nursing education that allows students t ...
Preceptorship is a crucial component of nursing education that allows students to work closely with an experienced nurse in a clinical setting. This hands-on learning experience allows nursing students to apply theoretical knowledge to real-life situations, develop essential skills, and gain confidence in their abilities. Setting SMART goals for your preceptorship can help you maximize this valuable learning opportunity and prepare you for a successful nursing career.
Who is a Nurse Preceptor?
A nurse preceptor is an experienced registered nurse who provides one-on-one guidance, support, and mentorship to a nursing student or new graduate nurse in a clinical setting. Preceptors are typically chosen based on their clinical expertise, leadership skills, and ability to teach and mentor others. They play a vital role in helping students bridge the gap between classroom learning and real-world nursing practice by assisting with learning objectives and offering nursing students assistance.
What does a Nurse Preceptor do?
A nurse preceptor has several key responsibilities, including:
A nurse preceptor has several key responsibilities, including:
- Orientation: Introducing the student to the unit, staff, policies, and procedures.
- Role modeling: Demonstrating best practices in patient care, communication, and professionalism.
- Teaching: Providing hands-on instruction and guidance in clinical skills, critical thinking, and decision-making. For instance, you might ask your preceptor to allow you to practice certain procedures like IVs, injections, or sterile dressing changes.
- Evaluation: Assessing the student’s performance, providing constructive feedback, and completing necessary evaluations.
- Support: Offering emotional support, encouragement, and a safe learning environment for the student.
- Support: Offering emotional support, encouragement, and a safe learning environment for the student. Preceptors serve as the best source of information and guidance during clinical rotation.
Building a Relationship with Your Nursing Preceptor
Establishing a positive, professional relationship with your preceptor is essential for a successful preceptorship experience. Here are some tips for building a strong relationship:
- Be proactive: Introduce yourself, express your enthusiasm to learn as much as possible, and discuss your goals and expectations.
- Communicate openly: Share your strengths, weaknesses, and learning needs with your preceptor. Consider discussing your learning style and how your preceptor can best support you.
- Be respectful: Respect your preceptor’s time, expertise, and feedback.
- Be prepared: Come to each shift with a positive attitude, ready to learn and participate actively. You might even request that your preceptor help you with specific skills or tasks.
- Seek feedback: Ask for feedback from your preceptor regularly on your performance and be open to constructive criticism.
Goals for Nursing Students During Preceptorship
Setting specific, achievable goals for your preceptorship can help you focus your learning, track your progress, and develop the skills and knowledge necessary to become a competent nurse. Here are some key goals to consider:
Enhance communication with other personnel
Effective communication is critical in nursing. During your preceptorship, aim to:
- Practice active listening and clear, concise communication with patients, families, and healthcare team members. SBAR (Situation, Background, Assessment, Recommendation) can be a useful tool.
- Learn and use proper medical terminology and documentation. Your preceptor can help ensure you’re using the correct documentation format to ensure complete notes.
- Develop strategies for communicating with challenging patients or families.
- Participate in interdisciplinary rounds and collaborate with other healthcare professionals.
Strengthen organizational skills
Nurses must be able to manage multiple tasks and priorities efficiently. Set goals to:
- Learn and practice time management techniques, such as prioritization and delegation.
- Develop a system for organizing patient information and tasks.
- Master the use of electronic health records and other documentation tools.
- Adapt to changing patient needs and unexpected situations calmly and efficiently.
Increase psychomotor ability
Preceptorship is an opportunity to refine your clinical skills. Aim to:
- Perform basic nursing skills, such as vital signs, medication administration, and wound care, with increasing confidence and proficiency.
- Under your preceptor’s guidance, learn and practice more advanced skills, such as IV insertion, catheterization, and tracheostomy care.
- Seek opportunities to observe or assist with specialized procedures relevant to your interest.
Increase medical knowledge
Expanding your medical knowledge is essential for providing evidence-based, high-quality patient care. During your preceptorship, strive to:
- Deepen your understanding of common diseases, treatments, and medications relevant to your clinical setting.
- Research and share current best practices and clinical guidelines with your preceptor and team.
- Participate in educational opportunities like in-services, case studies, and journal clubs.
- Ask questions and seek clarification when encountering unfamiliar topics or situations.
Strengthen critical thinking skills
Nursing requires strong critical thinking and problem-solving abilities. Set goals to:
- Practice assessing patients, identifying potential problems, and developing appropriate interventions.
- Analyze complex patient scenarios and discuss your thought process with your preceptor.
- Participate in clinical decision-making and develop evidence-based care plans.
- Reflect on your experiences and learn from both successes and challenges.
Develop leadership skills
Preceptorship is a chance to develop the leadership skills necessary for a successful nursing career. Aim to:
- Observe and learn from your preceptor’s leadership style and techniques.
- As appropriate, practice delegating tasks and supervising nursing assistants or other team members.
- Develop strategies for motivating and supporting colleagues and fostering a positive team dynamic.
- Seek opportunities to take on additional responsibilities or lead small projects with your preceptor’s guidance.
Enhance assertiveness skills
Assertiveness is a crucial skill for nurses, who must advocate for their patients and work effectively in a team. During your preceptorship, strive to:
- Practice speaking up respectfully and confidently when you have concerns, questions, or ideas.
- Learn and apply techniques for managing conflict and communicating assertively with colleagues, patients, and families.
- Develop strategies for advocating for patient needs and ensuring safe, high-quality care.
- Set and maintain professional boundaries while building positive relationships.
Provide quality patient education
Patient education is a key nursing responsibility that can significantly impact patient outcomes. Set goals to:
- Observe and learn from your preceptor’s patient education techniques.
- Practice providing clear, accurate, and culturally sensitive patient education on medication, self-care, and disease management topics.
- Develop and deliver patient education materials under your preceptor’s guidance, such as handouts or demonstrations.
- Evaluate the effectiveness of your patient education and seek feedback from your preceptor and patients.
Participate in organized learning experiences
Preceptorship programs often include structured learning experiences to supplement hands-on clinical learning. Aim to:
- Attend and actively participate in orientation sessions, workshops, and seminars designed for preceptees.
- Complete any required assignments, such as case studies, reflective journals, or presentations, to deepen your learning and demonstrate your progress.
- Collaborate with fellow preceptees to share experiences, knowledge, and support.
- Provide constructive feedback on the preceptorship program to help improve future experiences.
Be a role model of nursing values
As a nursing student, you represent the nursing profession and are responsible for upholding its core values. During your preceptorship, strive to:
- Demonstrate compassion, respect, and empathy in all interactions with patients, families, and colleagues.
- Maintain patient privacy and confidentiality following HIPAA regulations.
- Practice ethical decision-making and adhere to the nursing code of ethics.
- Display a commitment to lifelong learning, professional development, and evidence-based practice.
- Reflect on your own biases and work to provide culturally competent, patient-centered care.
How to Make the Most From Your Nursing Preceptorship
In addition to setting and working towards specific goals, there are several strategies you can use to maximize your learning and growth during your preceptorship:
Be an active learner
- Take initiative in your learning by asking questions, seeking feedback, and participating fully in patient care.
- Reflect on your experiences and keep a journal to track your progress, challenges, and insights.
- Seek additional learning opportunities, such as observing procedures or attending educational sessions.
Build relationships
- Develop a positive, professional relationship with your preceptor built on trust, respect, and open communication.
- Engage with other healthcare team members, including nurses, physicians, and allied health professionals.
- Participate in team meetings, rounds, and social events to foster a sense of belonging and collaboration.
Embrace challenges
- View challenges and mistakes as opportunities for growth and learning.
- With your preceptor’s support, be willing to step outside your comfort zone and take on new responsibilities.
- Maintain a positive attitude and resilience in the face of setbacks or difficult situations.
Seek and provide feedback
- Actively seek feedback from your preceptor and other team members on your performance, strengths, and areas for improvement.
- Be open and receptive to constructive criticism, and use it to guide your learning and development.
- Provide respectful, constructive feedback to your preceptor and the preceptorship program to help improve the experience for future students.
Take care of yourself
- Prioritize self-care and maintain a healthy work-life balance to avoid burnout and manage stress.
- Practice effective time management and organization to balance your clinical responsibilities with your personal and academic commitments.
- Build a support system of family, friends, and fellow nursing students to share experiences and provide encouragement.
Plan for the future
- Reflect on your preceptorship experiences and use them to inform your career goals and interests.
- Seek advice from your preceptor and other mentors on career planning, job search strategies, and professional development opportunities.
- Use your preceptorship to build professional networks and connections supporting your future career growth.
Your nursing preceptorship is a unique and valuable opportunity to learn, grow, and prepare for your future as a registered nurse. By setting clear goals, actively engaging in your learning, and maximizing your experiences, you can emerge from your preceptorship with the skills, knowledge, and confidence necessary to provide high-quality patient care and succeed in your nursing career.
What is the goal of nursing preceptorship?
The goal of nursing preceptorship is to help new nurses or nursing students gain practical, hands-on experience under the guidance of an experienced nurse (preceptor). It helps them build confidence, develop clinical skills, and transition smoothly from theory to real-world nursing practice.
What are the aims of preceptorship?
The aims of preceptorship are to:
- Support new nurses in adjusting to their roles.
- Enhance their clinical skills and knowledge.
- Build confidence and independence in patient care.
- Promote professional growth and development.
- Ensure high standards of nursing practice.
READ MORE >>
