Our Previous Samples
The dress code for nurses is not just about appearance; it significantly impacts ...
The dress code for nurses is not just about appearance; it significantly impacts patient perception and trust. Your attire can influence how patients perceive your professionalism and competence as a nurse. Let’s delve into this aspect of the nursing dress code.
What is the Dress Code for Nurses?
The dress code for nurses varies depending on the healthcare facility, but nurses are generally required to wear scrubs and loose-fitting, comfortable garments designed for medical professionals.
Some facilities may allow nurses to wear professional attire, such as dress pants and a button-down shirt, but this is less common. The dress code also includes guidelines for grooming, such as keeping hair neat and limiting jewelry and fragrances.
Why Do Nurses Wear Scrubs?
Scrubs are the standard uniform for nurses for several reasons. First and foremost, scrubs are designed to be comfortable and allow for easy movement, which is essential when providing patient care.
Scrubs are also easy to clean and replace, which is important in a healthcare setting where cleanliness is paramount. Additionally, scrubs help to identify nurses and other medical professionals, making it easier for patients and colleagues to recognize them.
The History of Nursing Uniforms & Scrubs
The history of nursing uniforms dates back to the early 19th century when nurses wore long dresses with aprons and caps. Over time, the uniform evolved to include shorter dresses and more practical designs.
The first scrubs were introduced in the 1940s. They were designed to be worn in the operating room to maintain a sterile environment. By the 1960s, scrubs had become the standard for nurses and other medical professionals.
Common Nurse Dress Code Requirements
Nurses must adhere to specific dress code requirements to maintain a professional appearance and ensure a safe and hygienic work environment. Let’s discuss the common nurses dress code requirements, including clothing, grooming, and dress code guidelines.
Clothing Requirements for Nurses
Nurses are required to follow specific guidelines regarding their clothing.
- Scrubs: Scrubs are the most common type of clothing worn by nurses. They are typically made of lightweight, breathable material and come in various colors and patterns. Some facilities may require nurses to wear specific colors or styles of scrubs.
- Professional Attire: In some cases, nurses may wear professional attire, such as dress pants and a button-down shirt. However, this is less common than wearing scrubs.
- Undergarments: Nurses are expected to wear appropriate undergarments that are not visible through their clothing.
- Socks or Stockings: Nurses should wear socks or stockings that cover their feet and ankles.
- Undershirts: If wearing scrubs, nurses may wear an undershirt for added comfort and coverage.
- Jackets: Some facilities may allow nurses to wear a jacket or sweater over their scrubs for added warmth.
Grooming Requirements
Nurses must also adhere to certain grooming standards. Let’s look at the guidelines for tattoos, piercings, facial hair, hair, fingernails, and makeup.
- Tattoos: Many healthcare facilities have policies regarding visible tattoos. Some may require nurses to cover their tattoos while on duty.
- Piercings: Nurses may be required to remove or cover certain piercings, such as facial piercings, while on duty.
- Facial Hair: Male nurses are typically required to keep their hair neat and trimmed.
- Hair: Nurses should keep their hair neat, and long hair should be pulled back to avoid interfering with patient care.
- Fingernails: Nurses should keep their fingernails short and clean and avoid wearing artificial nails or nail polish.
- Makeup: If worn, makeup should be minimal and professional.
Dress Code Requirements
Dress code requirements for nurses extend beyond clothing and grooming.
- Head Coverings: Some nurses may wear head coverings for religious or cultural reasons. Healthcare facilities typically have policies to accommodate these needs.
- Jewelry: Nurses should limit their jewelry to a simple watch, wedding band, and small earrings. Dangling jewelry or excessive jewelry may interfere with patient care.
- Fragrances: Nurses should avoid wearing strong fragrances, as some patients may be sensitive to smells.
- ID Badges: Nurses are required to wear an ID badge at all times while on duty.
- Watches: Nurses may wear a simple watch to help keep track of time and monitor patient vital signs.
- Shoes: Nurses should wear comfortable, closed-toe shoes with non-slip soles to ensure safety and comfort while on their feet for long periods.
Protective Equipment in Nurses’ Uniforms
In addition to their regular uniforms, nurses may be required to wear protective equipment when providing care to patients with infectious diseases or in certain medical situations. This equipment may include:
- Gowns: Disposable or reusable gowns worn over scrubs to protect against bodily fluids and other contaminants.
- Face Masks: Masks worn to prevent the spread of infectious diseases and protect the nurse from airborne particles.
- Surgical Caps: Caps are worn to keep the nurse’s hair covered and maintain a sterile environment.
- Disposable Gloves: Gloves are worn to protect the nurse’s hands and prevent the spread of infection.
Nurse Dress Codes After Nursing School
After completing nursing school, new nurses may have questions about what to wear on the job. New nurses need to familiarize themselves with their employer’s dress code policies and ask questions if anything is unclear. Some nursing schools may guide appropriate attire for job interviews and orientation.
Pros and Cons Of Dress Code For Nurses
Implementing a dress code for nurses has both advantages and disadvantages. This section will present a table outlining the pros and cons of having a dress code for nurses.
ProsConsPromotes professionalism and creates a positive image of the healthcare facilityCan be uncomfortable or restrictive, especially during long shiftsHelps to identify nurses and other medical professionalsMay limit personal expression and individualityEnsures a clean and hygienic environment for patient careCan be expensive to purchase and maintain multiple sets of scrubsAllows for easy movement and comfort while providing patient careSome nurses may feel that the dress code is too strict or rigidProtects against bodily fluids and other contaminantsThe Importance of Proper Clothing and Dress Codes for Nurses
Proper clothing and adherence to dress codes are essential for nurses for several reasons.
- They ensure a professional appearance and help to create a positive image of the healthcare facility. Patients and their families expect nurses to look professional and put-together, and a neat and tidy appearance can help to inspire confidence and trust.
- They help to ensure a clean and hygienic environment for patient care. Scrubs and other medical attire are designed to be easily cleaned and replaced, which is important in a healthcare setting where infection control is a top priority.
- They promote safety and comfort for nurses. Scrubs and other medical attire are designed to allow for easy movement and are made from breathable, comfortable materials. This is important for nurses on their feet for long periods and need to move quickly and easily to provide patient care.
Impact of Dress Code on Patient Perception
A nurse’s appearance can significantly impact patient perception and satisfaction. Patients who perceive their nurses as professional and well-groomed are more likely to have confidence in their care and to rate their overall experience more positively.
Nurses who appear unkempt or unprofessional may cause patients to question the quality of their care, leading to lower patient satisfaction scores. This is why it is so important for nurses to adhere to dress code policies and to maintain a tidy appearance at all times.
What Should a Nurse Wear on Orientation?
As a new nurse, making a good first impression on your first day of orientation is important. Most healthcare facilities will guide you on what to wear, but generally, it is best to be professional. If scrubs are required, choose a neutral color and ensure they are clean and wrinkle-free. Wear dress pants or a skirt with a button-down shirt or blouse if professional attire is allowed.
Avoid anything too revealing or casual, such as jeans or T-shirts. In addition to clothing, pay attention to your grooming and accessories. Ensure your hair is neat, and avoid wearing excessive jewelry or strong fragrances. Wear comfortable, closed-toe shoes with non-slip soles, and make sure your ID badge is always visible.
READ MORE >>
Nurse Practitioner Professional Career Planner NRNP 6675Nurse Practitioner Profe ...
Nurse Practitioner Professional Career Planner NRNP 6675
Nurse Practitioner Professional Career Planner NRNP 6675
The Assignment
Develop a cover letter, resume, philosophy statement, and other professional resources that meet the requirements outlined in the Career Planner Guide.
As you approach the end of your Master of Science in Nursing program and prepare for a career as a nurse practitioner, you will want to create a cover letter, resume, and portfolio that best represent your knowledge, skills, and abilities as a professional in the field of nursing.
For this Assignment, you will create a Career Planner, which includes these elements, that you can use as you pursue your next professional role.
To Prepare
Review the Career Planner Guide. This document contains the requirements for the Assignment as well as resources to consult.
Seek out other resources on cover letters, resumes, and other professional resources, as needed. The Walden University Career Planning and Development site has information on many topics of relevance.
Learning Resources
Required Readings (click to expand/reduce)
American Nurses Credentialing Center. (n.d.). Psychiatric-mental health nurse practitioner (across the lifespan) certification (PMHNP-BC).
https://www.nursingworld.org/our-certifications/psychiatric-mental-health-nurse-practitioner/
Scroll to ANCC Study Aids- Free for sample test questions and study guides to help you prepare for your certification exam.
Buppert, C. (2021). Nurse practitioner’s business practice and legal guide (7th ed.). Jones & Bartlett Learning.
Chapter 12, Lawmaking and Health Policy
Chapter 14, Standards of Care for Nurse Practitioner Practice
Chapter 15, Measuring Nurse Practitioner Performance
The National Organization of Nurse Practitioner Faculties. (2017). Nurse practitioner core competencies. https://cdn.ymaws.com/www.nonpf.org/resource/resmgr/competencies/20170516_NPCoreCompsContentF.pdf
The National Organization of Nurse Practitioner Faculties. (n.d.). National organization of nurse practitioner faculties. https://www.nonpf.org/
Stewart, J. G., & DeNisco, S. M. (2019). Role development for the nurse practitioner (2nd ed.). Jones & Bartlett Learning.
Chapter 11, Concepts of the Professional
Chapter 12, Health Policy and the Nurse Practitioner
Chapter 14, Mentoring
Zakhari, R. (2021). The psychiatric-mental health nurse practitioner certification review manual. Springer Publishing Company.
Chapter 1, Preparing to Pass the Psychiatric-Mental Health Nurse Practitioner Certification Exam (for review as needed)
Chapter 16, Practice Test
Document: Career Planner Guide
Required Media (click to expand/reduce)
APRN Central. (2019, October 27). Goal digger: Test taking strategies [Video]. YouTube. https://www.youtube.com/watch?v=STAT1WpQgSM
DrRegisteredNurse. (2020, February 16). Test-taking strategies to pass the NCLEX in 75 questions part 1 [Video]. YouTube. https://www.youtube.com/watch?v=81E3dAxrO2c
NRNP 6675: PMHNP Care Across the Lifespan II
Career Planner Guide
Your Nurse Practitioner Professional Career Planner is due by Day 7 of Week 10. It is highly recommended that you begin planning and working on this Assignment as early in the quarter as is feasible for you. The following checklists outline all of the items you should include in your Career Planner. Additionally, the resources below have been provided to assist you in its development.
Refer to the Walden University Career Center website for resources and information on how to create cover letters, resumes, and professional portfolios. You may also choose to make certain portions of your Career Planner accessible online to members of your professional network or potential employers through platforms such as LinkedIn. Sharing on social media is a useful way to network for many, but it is not a requirement for this assignment.
Checklist for Cover Letter
Cover letters are typically tailored to individual jobs and companies. For this Assignment, you will select a job posting you would like to or could potentially apply for and create a cover letter for it. Your cover letter should be:
- Presented and formatted in professional business manner
- Addressed properly
- Clear and concise (no more than one page) and include:
- Content introduction
- Content body
- Content conclusion
- Written in a professional tone and include:
- Correct spelling, punctuation, and grammar
- Clear and accurate sentence structure
Checklist for Resume
Your resume should be clear, concise, and well organized, and it should also include your:
- Name, location (city/town and state), business phone number, and email address (centered at top of resume)
- Objective: 2–3 sentences describing your goal/objective for employment
- Certifications & licenses
- Education
- Professional experience
- Honors/Awards (as applicable)
Checklist for Portfolio
Your Portfolio should be clear, concise, and well organized, and it should also include your:
- Personal philosophy statement (1-page)
- Personal goals (short term and long term)
- Self-assessment
The following items do not have to be submitted but should be available on request for employers:
- Achievements
- Letters of recommendation (2)
- References (list names, affiliation, and contact information) (3)
- Certifications and licenses
- Prior degrees
- Transcripts (Note: An unofficial transcript will meet this requirement.)
- Certificates of attendance for continuing education
- Publications
- Research
- Oral presentations and/or poster presentations
Learning Resources
Resume and Cover Letter Resources:
Canva. (n.d.). https://www.canva.com/
Canva has many resume templates and formats that may inspire your creativity. (Using Canva is optional.)
Cover Letter Advice (n.d.). Nurse practitioner cover letter sample 1. http://www.coverletter.us/nurse-practitioner-cover-letter/
DeCapua, M. (2019). A nurse practitioner’s guide to the perfect cover letter. Health eCareers. https://www.healthecareers.com/article/healthcare-news/np-cover-letter
Hicks, R. W., & Roberts, M. E. E. (2016). Curriculum vitae: An important tool for the nurse practitioner. Journal of the American Association of Nurse Practitioners, 28(7), 347–352.
Gibson, A. (n.d.). Nurse.org career guide series: Ultimate guide to nursing resumes. Nurse.org. https://nurse.org/resources/nursing-resume/
Walden University Career Services. (n.d.). Resumes & more. https://academicguides.waldenu.edu/careerservicescenter/resumesandmore
Portfolio Resources:
Chamblee, T. B., Dale, J. C., Drews, B., Spahis, J., & Hardin, T. (2015). Implementation of a professional portfolio: A tool to demonstrate professional development for advanced practice. Journal of Pediatric Health Care, 29(1), 113–117.
Clarke, M. (2019). The importance of a professional nursing portfolio. HealthLeaders. https://www.healthleadersmedia.com/nursing/importance-professional-nursing-portfolio
Nurse Practitioner Business Owner. (n.d.). This is why you want to create your professional portfolio today! https://npbusiness.org/professional-portfolio/
Portfolium. (n.d.). https://portfolium.com/
Portfolium is one example of portfolio software that you could use to create a portfolio. You may choose your own tool, and it may be online (Google Sites, Portfolium) or offline (Word, pdf), as long as you can easily submit the portfolio files or link to your Instructor.
COVER LETTER SAMPLE
Dear Sir/Madam,
RE: APPLICATION FOR A FAMILY NURSE PRACTITIONER
This letter shows my interest in the family nurse position advertised on 19th February 2020. I am a graduate of a family nurse from the Washington Adventist University, and I am currently pursuing my master’s degree at Walden University as a family nurse practitioner. I also have over 10-years of experience as a registered nurse.
In my line of operation, I have been consistent and passionate about bringing social changes to organizations and having an opportunity to care for patients with chronic and acute conditions. Additionally, as I send my application for the above-referenced position, I am also looking to expand my career while working at the institution.
Currently, I am a clinical administrator and float pool nurse at Shady Groove Medical Center. While working there for both positions, I have gained skills in overseeing staff, supervising units/departments, and ensuring regulatory compliance, patient safety, time management, and personal safety. The institution has also given me opportunities to interpret and analyze patient history, conduct diagnostic tests, perform physical examinations, and make diagnoses in a busy critical care unit.
Ultimately, I can effectively work as a team player or independently to guarantee better service delivery for the people with or without supervision. I can function under pressure and still maintain a calm nature that will allow solutions for problematic issues that require my attention. Throughout my studies, I have acquired essential skills such as professional practice guidelines, standards of care, and scientific rationale that are critical for developing treatment plans based on evidence-based principles.
When given a chance to work at this institution, I can guarantee a positive and cooperative attitude and implement my skills to advance the organization’s interests. I believe that even as I advance my career while working in this organization, my contribution will help stir the organization to greater heights. It would be my pleasure to be considered part of the team. I am looking forward to hearing from you soon.
Sincerely
Student Name
Also Read: Prescribing for Older Adults and Pregnant Women NRNP6675
READ MORE >>
NURSFPX 4900 ASSESSMENT Problem Identification TemplateNURSFPX 4900 ASSESSMENT P ...
NURSFPX 4900 ASSESSMENT Problem Identification Template
NURSFPX 4900 ASSESSMENT Problem Identification Template
I need the attached file “Problem Identification Template” completed with Opioid Addiction as the topic.
Please refer to the 2nd file attached called “Assessment 1-3 COPY” for reference to complete this template.
The template entitled ” Problem Identification Template” needs to be in association with the attached file. They should flow together as they are part of a large project.
Below is the competency points that need to be adhered to for a satisfactory answer.
- Competency 1: Lead people and processes to improve patient, systems, and population outcomes.
- Define a patient, family, or population health problem that is relevant to personal practice.
- Competency 2: Make clinical and operational decisions based upon the best available evidence.
- Analyze evidence from the literature and professional sources to support decisions related to defining and guiding nursing actions related to a health problem.
- Competency 7: Implement patient-centered care to improve quality of care and the patient experience. NURSFPX 4900 ASSESSMENT Problem Identification Template
- Propose strategies to improve patient or population outcomes related to a health problem.
- Competency 8: Integrate professional standards and values into practice.
- Reflect on state board nursing practice standards relevant to a selected health problem.
- Communicate professionally with clear, logically organized writing, using correct grammar, spelling, and APA style.
NURSFPX 4900 ASSESSMENT Problem Identification Template Problem Identification Template
The following is a guide to organize your assignment. Please be sure to remove the guiding questions and comments for each section. You are expected to write in a professional and academically appropriate manner throughout. Make sure you are using proper APA style and citations throughout.
Define a patient, family, or population health problem, and realistic goals, that are relevant to personal practice.
- Introduce a general summary of the health problem that you will be exploring.
- Provide a brief context for the patient, family, or population struggling with this health problem.
- Propose one or more goals that you deem appropriate and relevant to the health problem.
- Briefly state why this health problem is relevant to your personal practice.
- NURSFPX 4900 ASSESSMENT Problem Identification Template
Analyze evidence from the literature and professional sources to support decisions related to defining and guiding nursing actions related to a health problem.
- Compare and contrast the authors you will be citing, discussing pros and cons of the evidence you are reading about.
- Note whether the authors provide supporting evidence from the literature that is consistent with what you see in your nursing practice.
- Assess the quality of the data presented in the articles you are reading.
- Discuss how you would know if the data were unreliable.
- Include what the literature says about barriers to evidence-based practice.
- Describe research studies that present opposing views regarding this health problem.
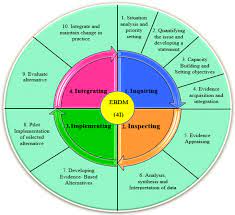
- Describe what the literature says about a nursing theory or conceptual framework that might frame and guide your actions during your clinical practicum.
- NURSFPX 4900 ASSESSMENT Problem Identification Template
Propose potential strategies to improve patient or population outcomes related to a health problem.
- Cite any known authors who have recommended leadership strategies for nurses to use when providing care to this patient population.
- Discuss research on the effectiveness of these strategies in improving patient or population outcomes regarding this health problem.
- Describe what the literature says about patient-centered care, empowering patients to make health care decisions, involving families in patient care, incorporating patient preferences to improve outcomes, prevent illness, and lower readmissions to hospitals.
- Discuss ways your role as a nurse leader will help improve patient outcomes as described in the literature.
- NURSFPX 4900 ASSESSMENT Problem Identification Template
Reflect on state board nursing practice standards relevant to a project related to a health problem.

- Discuss how your state’s nurse practice act will guide your actions in terms of this health problem for this patient or population.
- Identify the most surprising thing that you found while reading your state’s nurse practice act.
- Describe the effects of local, state, and federal laws on your nursing scope of practice and care for this patient or population.
- Explain how nursing ethics will inform your intervention in this clinical practicum.
NURSFPX 4900 ASSESSMENT Problem Identification Template References
Remember to compile your APA-formatted reference list.
NURSFPX 4900 ASSESSMENT Problem Identification Template – Plan Proposal Template Completed with Opioid Topic
The adverse effects of opioids have adverse effects on families, individuals, and American society as a whole. The opioid epidemic is a major problem to the health care system hence the need to address this problem. It leads to poor quality of life and the high cost of medication.
Research indicates that the majority of individuals who develop an addiction to opioids are people who, at some point, received the prescription as pain medication (Addiction Center, 2018). In line with the phrase ‘prevention is better than cure,’ the proposed intervention is to increase access to prevention service to people at risk of the opioid epidemic.
Implementation of the proposed plan can help prevent adverse social, health and economic effects associated with opioid abuse, misuse, and addition. Early intervention to people at risk, education to create awareness to people at risk and the public, digital and social media campaigns, community and school-based programs. Patients prescribed opioids as pain relievers and adolescents will be the main target for intervention services.
Collaboration between various agencies such as national health institute, FDA, and NIDA with private sectors are necessary for developing alternative pain relievers and analgesics and analgesics that cannot be abused easily (US Department of Health and Human Services, n. d). Collaboration with state agencies is essential in improving technologies that can detect trafficking and import of illegal opioids NURSFPX 4900 ASSESSMENT Problem Identification Template.
The interprofessional collaborators will comprise the local caregivers including both clinicians/nurses and behavioural therapists (psychiatrists, social workers, pharmacists, department of justice, training institutions, faith-based organizations, local authority, and community-based organizations
The proposal will be submitted to the health staff and collaborators to give their feedback on making the project better. The refined proposal will be submitted by the nurse manager to the facility board members for approval. If approved, the plan will be implemented in the community and hospital with the help of my mentor and the nurse manager as the project managers as well as the support of collaborators.
Technolicical Analysis
Digital and social media technology can be used in the proposed intervention to improve access to prevention services. Chassiakos et al (2016) found a high rate of internet usage among adolescents and young adults than any other demographic groups. Therefore, digital and social media is relevant in disseminating health information about opioid prevention services to our target population.
Riley et al (2011 ) observed that digital health interventions such as eHealth and mHealth are crucial tools in amplifying the public health messages and promoting behavior change to promote healthy living. A study by Årsand et al (2012) found that health services through social media, automated phone, and SMS services (to people with previous opioid prescriptions) prevented potential opioid addiction and misuse NURSFPX 4900 ASSESSMENT Problem Identification Template.
Overall, these studies indicate that digital and social media technologies are crucial tools in amplifying public health messages and manage health conditions. Hence, literature offers supportive evidence on the use of digital and social media tools in nursing practice. These are evident in the use of eHealth and mHealth in managing diabetes and cardiovascular disorders.
However, given that 23% of Americans do not use a smartphone can hinder the use of digital and social media tools in the prevention of opioid addiction, overdose, and misuse. Instead, combining it with an automatic phone and SMS technology could be most appropriate. Lack of reliability, privacy and confidentiality issues, information overload, and dissemination of false information are other factors that deter the use of digital and social media platforms to disseminate information on opioid prevention services.
However, Murray et al (2011) and Mair et al (2012) argued that digital health interventions are complex and cumbersome to implement due to factors like interoperability, unfit to the current system, high cost, disrupting face-to-face interaction between patients and health professionals NURSFPX 4900 ASSESSMENT Problem Identification Template.
Governmental & Organizational Policies
Health care policies support projects aimed at preventing, treatment, and recovery of those affected by opioids. Both state and Federal governments have enacted policies to curb increased deaths fro opioids overdose. This includes the collection and dissemination of information on opioids abuse and addiction. These policies seek to promote public education and awareness campaigns- this is consistent with the proposed plan.
It also covers community and school-based methods of preventing opioid addiction and misuse (Taft, & Nanna, 2008). Other areas of covered include reducing access and availability of opioids, investing in research to develop less abusive analgesics and alternative pain relievers. Therefore, the design and implementation of the proposed plan are consistent with state and federal policies.
RNs are increasingly influencing health care policies, making to improve patient outcomes and prevention of diseases. With the evolving role of nurses in health care, nurse managers have taken up the role previously reserved for physicians. As a unit manager, nurse managers are tasked with ensuring the safety of patients. The managers should encourage a nurse to engage in research and policy initiatives and changes to improve quality of care.
As a nurse manager, I will seek to propose prevention intervention for opioids through the local government commissions and county health department board. This will be accomplished after the trials at the community and my current facility. The proposed intervention, which based on EBP can then be rolled out to communities and health facilities in the state to help prevent opioid misuse and addiction.
Communicating and Collaborating to Improve Health Outcomes
Interprofessional teams communication and collaboration strategies will be fostered through training of doctors, nurses, and other participants together on opioid prevention services. It can be enriched by retraining these participants on how they can work together as a team to prevent, treat, and help in the recovery of patients from opioid disorders.
The other strategies include the use of interdisciplinary rounds consisting of various professionals in health care. Team huddles method can be used to outline the work that is ahead by clarifying issues to be tackled. Effective communication aided by digital and social media and digital platforms will be used to improve interprofessional communication and collaboration.
Communication strategies between patients and health professionals will involve the digital and social media tools targeted youths- the groups at high risk of opioid addiction and misuse. The second strategy is automatic phone and SMS messaging to the potential opioid addicts and abusers. For one-on-one communication, there is a need to create a rapport with patients and people risk to give them insight regarding the negative effects of opioid addictions.
In my clinical practicum environment, a nurse manager, mentor, nurses, patients, physicians, and administrative staff are critical in implementing the proposed plan. Accordingly, I get unwavering support from my mentor and nurse manager to ensure the project succeeds. I also plan to interact with patients on opioid prescriptions and disorders to gain their opinions on how they react to the proposed plan.
Surprisingly, I realized that initially, facility management was unwilling to support education and behavior change in opioid addicts, but rather prefer the use of medications such as naloxone (Narran) as opposed to prevention interventions.
There are benefits of getting input from participants. First, patient input helps to understand their feelings and possible reaction to the intervention NURSFPX 4900 ASSESSMENT Problem Identification Template. Secondly, input from nurses and doctors will improve the proposed intervention to generate better patient outcomes.
NURSFPX 4900 ASSESSMENT Problem Identification Template References
Årsand, E., Frøisland, D. H., Skrøvseth, S. O., Chomutare, T., Tatara, N., Hartvigsen, G., & Tufano, J. T. (2012). Mobile health applications to assist patients with diabetes: lessons learned and design implications. Journal of diabetes science and technology, 6(5), 1197-1206.
Chassiakos, Y. L. R., Radesky, J., Christakis, D., Moreno, M. A., & Cross, C. (2016). Children and adolescents and digital media. Pediatrics, 138(5), e20162593. https://pubmed.ncbi.nlm.nih.gov/27940795/
Mair FS, May C, O’Donnell C, Finch T, Sullivan F, Murray E. Factors that promote or inhibit the implementation of e-health systems: an explanatory systematic review. Bull World Health Organ. 2012;90(5):357–64
Murray E, Burns J, May C, Finch T, O’Donnell C, Wallace P, et al. Why is it difficult to implement e-health initiatives? A qualitative study. Implement Sci. 2011;6(1):6.
Riley, W. T., Rivera, D. E., Atienza, A. A., Nilsen, W., Allison, S. M., & Mermelstein, R. (2011). Health behavior models in the age of mobile interventions: are our theories up to the task?. Translational behavioral medicine, 1(1), 53-71. NURSFPX 4900 ASSESSMENT Problem Identification Template
Taft, S. H., & Nanna, K. M. (2008). What are the sources of health policy that influence nursing practice?. Policy, Politics, & Nursing Practice, 9(4), 274-287.
US Department of Health and Human Services. (n. d) Straegy to Combat Opioid Abuse, Misuse, and Overdose. A framework Based on the Five Point Strategy. Retrieved from https://www.hhs.gov/opioids/sites/default/files/2018-09/opioid-fivepoint-strategy-20180917-508compliant.pdf
Define a patient, family, or population health problem, and realistic goals, that are relevant to personal practice.
Hypertension is the clinical name for high blood pressure. This condition is a very prevalent patient issue within the healthcare industry NURSFPX 4900 ASSESSMENT Problem Identification Template. Uncontrolled hypertension can lead to severe health complications. It also increases the risk for cardiovascular disease, stroke, heart failure and death. It is vital to keep blood pressure under to control to reduce the risk of these conditions.
The Centers for Disease Control (CDC) defends that approximately one in four adults with hypertension have it under control and that nearly half of the adults that have hypertension either are not prescribed medication, or they do not take their medication (2020). NURSFPX 4900 ASSESSMENT Problem Identification Template
It is estimated that every one out of two adults in the United States has hypertension (CDC, 2020). My mother, Mrs. J.M. is one of those adults struggling with hypertension. She is a 66-year-old Italian American woman. She is a former smoker, with a history of diabetes, colon cancer, obesity and hypothyroidism.
Her father who was deceased at the age of 78 suffered from hypertension, diabetes, heart disease and stroke. Her mother who is still living at the age of 89 currently suffers with hypertension and has a history of stroke NURSFPX 4900 ASSESSMENT Problem Identification Template. Her family history and comorbidities put her at a higher risk for other health related complications if left uncontrolled.
Not all individuals with hypertension require medication. One goal offered for patients with hypertension is lifestyle modification and weight loss. These two when combined have been proven to decrease blood pressure. Lifestyle modifications include; weight loss, exercise, eating a healthy diet, smoking cessation, and stress reduction.
In the case of Mrs. J.M. she has admitted that she needs to lose weight, she does not exercise, and her eating habits are not ideal. Given her family history and comorbidities it is important to implement a lifestyle modification plan for her NURSFPX 4900 ASSESSMENT Problem Identification Template.
This health problem is relevant to my practice because I am an ICU nurse. The majority of my patients come to the ICU with a diagnosis of hypertensive crisis or stroke due to uncontrolled hypertension.
Many of my patients have suffered multiple strokes with significant damage due to this problem. Pharmacist intervention can have a substantial impact on knowledge, blood pressure control and medication adherence for hypertensive patients (Saleem et al., 2015).
While medication might be the only option for some patients to control their blood pressure, as a nurse it is my duty to seek the least invasive option for my patients NURSFPX 4900 ASSESSMENT Problem Identification Template.
Analyze evidence from the literature and professional sources to support decisions related to defining and guiding nursing actions related to a health problem.
Lifestyle modification is an evidence-based strategy designed to eliminate and/or control hypertension. To support this strategy peer-reviewed scholarly journal articles written within the past five years were utilized. This allows for the most up-to-date available evidence-based information.
When using websites to find evidence-based research credible sources are NIH, .gov websites, .org websites, Mayo Clinic and hospital policies. However, blogs, Wikipedia and .com websites are not credible sources of information. Lifestyle modifications include weight loss, exercise, eating a healthy diet, smoking cessation, and stress reduction.
In an article written by Yang et al., a study of 1139 adults with hypertension complying with lifestyle modification was conducted. Patients were assessed on their lifestyle, including smoking, alcohol use, salt intake, and physical activity NURSFPX 4900 ASSESSMENT Problem Identification Template. The purpose of this study was to identify and evaluate life-style modifications associated with blood pressure control in patients diagnosed with hypertension.
The participants checked in at weeks 4, 8, and 12 and discussed drug adherence, weight, physical activity, alcohol and salt consumption, and blood pressure readings. At the conclusion of the study 961 participants (84%) were in the success group. It was discovered that reduced salt intake and increased physical activity were attributed to successful blood pressure control, and increased BMI was associated with uncontrolled blood pressure
The article stated that dietary modifications which are beneficial in reducing hypertension include low sodium intake, alcohol in moderation, weight loss, a diet rich in fruits, vegetables, legumes, low-fat dairy products, and low saturated fat. The researchers also followed up with the participants after 18 months and weight reduction continued to show a trend in reduction of blood pressure (Yang, et al., 2017).
An article written by Magobe et al., stated that the first step in treating hypertension is lifestyle modification and that physical exercise can lower blood pressure and improve quality of life. In the referenced study participants had to engage in physical activity for 10 to 30 minutes a day at least three times a week.
The participants varied from ages 41 to 80 years old and had been diagnosed with hypertension for 1 to 10 years. Lifestyle modifications were proven to lower blood pressure and reduce cardiovascular disease by 21% when patients adhered to a healthy lifestyle (Magobe et al., 2017).
In my current nursing practice evidence from the literature proves to be true. When patients are admitted to the ICU with hypertensive crisis or stroke it is because they have uncontrolled hypertension. When educating them on proper diet, obesity, and exercise it is discovered that they do not practice these lifestyle behaviors. Lack of adequate treatment, reluctance to make lifestyle changes, compliance, and access to healthcare can present barriers to evidence-based practice (Devkota et al., 2016). NURSFPX 4900 ASSESSMENT Problem Identification Template
The Health Belief Model can be used to assist in behavior change for patients. This model is frequently used in the healthcare setting. In this model goal setting, decision-making, and social learning are integrated for making one’s own decisions, along with the patient’s perceived barriers for the change (Drevenhorn, 2018). This model can be effective in treating patient with hypertension because it allows the individual to make choices and decisions that can be a benefit/detriment to their health. NURSFPX 4900 ASSESSMENT Problem Identification Template
Propose potential strategies to improve patient or population outcomes related to a health problem.
Nurses play a critical role in ensuring safe, effective patient outcomes. Nurses serve as educators and care-coordinators for patients with hypertension. Patient-centered care is an effective approach to hypertension management. “A team-based approach is tailored to meet the patients’ needs and has shown to control hypertension NURSFPX 4900 ASSESSMENT Problem Identification Template.
Currently nurses are leading research teams to examine social, cultural, economic, and behavioral determinants of hypertension outcomes” (Dennison-Himmelfarb et al., 2016). As a nursing leader, patient outcomes can be improved by staying abreast with the most recent evidence-based best practices to improve patient safety NURSFPX 4900 ASSESSMENT Problem Identification Template. Nurse leaders also educate peers and other subordinate nurses on the importance of quality care and best practices. Nurse leaders play a vital role in providing high-quality patient care and services (Mansel & Einion, 2019).
Reflect on state board nursing practice standards relevant to a project related to a health problem.
The Nurse Practice Act was enacted to guide nursing practice. Every state Board of Nursing enforces these rules. The Texas Board of Nursing states that their mission “is to protect and promote the welfare of the people of Texas by ensuring that each person holding a license as a nurse in the state is competent to practice safely” (2019). It is important that nurses know and understand the nurse practice act to ensure we are practicing within the determined scope of practice. NURSFPX 4900 ASSESSMENT Problem Identification Template
In a previous course I had to research my state nursing board standards, and the information has not changed so there were no surprising notations. However, when I first moved to Texas and read about safe harbor that was something, we did not have in Florida which was surprising to me because it protects a nurse’s licensure. NURSFPX 4900 ASSESSMENT Problem Identification Template
An informed nurse is a competent nurse, competent nurses remain vigilant to keep their patients from harm. To evaluate how nursing ethics apply to this clinical practicum, I consulted the ethical considerations for nursing. Autonomy based on my experience and knowledge as a nurse I am able to provide my mother and my patients with valid advice.
In regard to beneficence I am compelled to not turn a blind eye to miseducation on my patients and mothers in regard to their health, as a practicing nurse I have an obligation and a duty for health promotion. Justice denotes that all patients are entitled to equal access of care.
NURSFPX 4900 ASSESSMENT Problem Identification Template References
- Centers for Disease Control (CDC). (2020Facts About Hypertension. Retrieved from
- https://www.cdc.gov/bloodpressure/facts.htm
- Dennison Himmelfarb, Cheryl & Commodore-Mensah, Yvonne & Hill, Martha. (2016).
- Expanding the Role of Nurses to Improve Hypertension Care and Control Globally. Annals of Global Health, (82) doi:10.1016/j.aogh.2016.02.003.
- Devkota, S., Dhungana, R. R., Pandey, A. R., Bista, B., Panthi, S., Thakur, K. K., & Gajurel, R.
- (2016). Barriers to Treatment and Control of Hypertension among Hypertensive Participants: A Community-Based Cross-sectional Mixed Method Study in Municipalities of Kathmandu, Nepal. Frontiers in Cardiovascular Medicine, (3)26. https://doi.org/10.3389/fcvm.2016.00026
- Drevenhorn, E. (2018). A Proposed Middle-Range Theory of Nurisng in Hypertension Care. International Journal of Hypertension, (11). doi:http://dx.doi.org.library.capella.edu/10.1155/2018/2858253
- Magobe, N. B., Poggenpoel, M., & Myburgh, C. (2017). Experiences of patients with hypertension at primary health care in facilitating own lifestyle change of regular physical
- exercise. Curationis, 40(1) Retrieved from http://library.capella.edu/login?qurl=https%3A%2F%2Fsearch.proquest.com%2Fdocview%2F1898593873%3Faccountid%3D27965
- Mansel, B., & Einion, A. (2019). “It’s the relationship you develop with them”: emotional intelligence in nurse leadership. A qualitative study. British Journal of Nursing, 28(21), 1400–1408. https://doi-org.library.capella.edu/10.12968/bjon.2019.28.21.1400
- Saleem, F., Hassali, M. A., Shafie, A. A., Haq, N. U., Farooqui, M., Aljadhay, H., & Ahmad, F. (2015). Pharmacist intervention in improving hypertension-related knowledge, treatment medication adherence and health-related quality of life: A non-clinical randomized controlled trial. Health Expectations, 18(5), 1270-1281. NURSFPX 4900 ASSESSMENT Problem Identification Template
- Texas Board of Nursing. (2019). Nurse Practice Act. Retrieved from http://www.bon.texas.gov
- Yang, M. H., Kang, S. Y., Lee, J. A., Kim, Y. S., Sung, E. J., Lee, K. Y., Kim, J. S., Oh, H. J., Kang, H. C., & Lee, S. Y. (2017). The Effect of Lifestyle Changes on Blood Pressure Control Among Hypertensive Patients. Korean Journal of Family Medicine, 38(4), 173–180. https://doi.org/10.4082/kjfm.2017.38.4.173.
READ MORE >>
NURSFPX4020 Capella Assessment 3 Improvement Plan In-Service Presentation.For th ...
NURSFPX4020 Capella Assessment 3 Improvement Plan In-Service Presentation.
For this assessment, you will develop an 8-14 slide PowerPoint presentation with thorough speaker’s notes designed for a hypothetical in-service session related to the improvement plan you developed in Assessment 2. As a practicing professional, you are likely to present educational in-services or training to staff pertaining to quality improvement (QI) measures of safety improvement interventions.
Such in-services and training sessions should be presented in a creative and innovative manner to hold the audience’s attention and promote knowledge acquisition and skill application that changes practice for the better. The teaching sessions may include a presentation, audience participation via simulation or other interactive strategy, audiovisual media, and participant learning evaluation.
The use of in-services and/or training sessions has positive implications for nursing practice by increasing staff confidence when providing care to specific patient populations. It also allows for a safe and nonthreatening environment where staff nurses can practice their skills prior to a real patient event. Participation in learning sessions fosters a team approach, collaboration, patient safety, and greater patient satisfaction rates in the health care environment (Patel & Wright, 2018).
As you prepare to complete the assessment, consider the impact of in-service training on patient outcomes as well as practice outcomes for staff nurses. Be sure to support your thoughts on the effectiveness of educating and training staff to increase the quality of care provided to patients by examining the literature and established best practices.
You are encouraged to explore the AONE Nurse Executive Competencies Review activity before you develop the Improvement Plan In-Service Presentation. This activity will help you review your understanding of the AONE Nurse Executive Competencies—especially those related to competencies relevant to developing an effective training session and presentation. This is for your own practice and self-assessment, and demonstrates your engagement in the course.
Demonstration of Proficiency
By successfully completing this assessment, you will demonstrate your proficiency in the following course competencies and assessment criteria:
- Competency 1: Analyze the elements of a successful quality improvement initiative.
- Explain the need for and process to improve safety outcomes related to a specific organizational issue.
- Create resources or activities to encourage skill development and process understanding related to a safety improvement initiative.
- Competency 4: Explain the nurse’s role in coordinating care to enhance quality and reduce costs.
- List the purpose and goals of an in-service session for nurses.
- Explain to the audience their role and importance of making the improvement plan successful.
- Competency 5: Apply professional, scholarly, evidence-based strategies to communicate in a manner that supports safe and effective patient care.
- Communicate with nurses in a respectful and informative way that clearly presents expectations and solicits feedback on communication strategies for future improvement.
Reference for NURSFPX4020 Capella Assessment 3: Improvement Plan In-Service Presentation.
- Patel, S., & Wright, M. (2018). Development of interprofessional simulation in nursing education to improve teamwork and collaboration in maternal child nursing. Journal of Obstetric, Gynecologic & Neonatal Nursing, 47(3), s16–s17.
PROFESSIONAL CONTEXT
As a baccalaureate-prepared nurse, you will often find yourself in a position to lead and educate other nurses. This colleague-to-colleague education can take many forms, from mentoring to informal explanations on best practices to formal in-service training.
In-services are an effective way to train a large group. Preparing to run an in-service may be daunting, as the facilitator must develop his or her message around the topic while designing activities to help the target audience learn and practice.
By improving understanding and competence around designing and delivering in-service training, a BSN practitioner can demonstrate leadership and prove him- or herself a valuable resource to others.
Also Read:
NURSFPX4020 Capella University Safety Improvement Plan Analysis Paper
NURSFPX4020 Capella Assessment 3 SCENARIO
For this assessment it is suggested you take one of two approaches:
- Build on the work that you have done in your first two assessments and create an agenda and PowerPoint of an educational in-service session that would help a specific staff audience learn, provide feedback, and understand their roles and practice new skills related to your safety improvement plan, or
- Locate a safety improvement plan through an external resource and create an agenda and PowerPoint of an educational in-service session that would help a specific staff audience learn, provide feedback, and understand their roles and practice new skills related to the issues and improvement goals presented in your chosen context.
NURSFPX4020 Capella Assessment 3: Improvement Plan In-Service Presentation Instructions
The final deliverable for this assessment will be a PowerPoint presentation with detailed presenter’s notes representing the material you would deliver at an in-service session to raise awareness of your chosen safety improvement initiative and to explain the need for it. Additionally, you must educate the audience as to their role and importance to the success of the initiative.
This includes providing examples and practice opportunities to test out new ideas or practices related to the safety improvement initiative. Be sure that your presentation addresses the following, which corresponds to the grading criteria in the scoring guide. Please study the scoring guide carefully so you understand what is needed for a distinguished score.
- List the purpose and goals of an in-service session for nurses.
- Explain the need for and process to improve safety outcomes related to a specific organizational issue.
- Explain to the audience their role and importance of making the improvement plan successful.
- Create resources or activities to encourage skill development and process understanding related to a safety improvement initiative.
- Communicate with nurses in a respectful and informative way that clearly presents expectations and solicits feedback on communication strategies for future improvement.
There are various ways to structure an in-service session; below is just one example:
Part 1: Agenda and Outcomes.
- Explain to your audience what they are going to learn or do, and what they are expected to take away.
Part 2: Safety Improvement Plan.
- Give an overview of the current problem, the proposed plan, and what the improvement plan is trying to address.
- Explain why it is important for the organization to address the current situation.
Part 3: Audience’s Role and Importance.
- Discuss how the staff audience will be expected to help implement and drive the improvement plan.
- Explain why they are critical to the success of the improvement plan.
- Describe how their work could benefit from embracing their role in the plan.
Part 4: New Process and Skills Practice.
- Explain new processes or skills.
- Develop an activity that allows the staff audience to practice and ask questions about these.
- In the notes section of your PowerPoint, brainstorm potential responses to likely questions or concerns.
Part 5: Soliciting Feedback.
- Describe how you would solicit feedback from the audience on the improvement plan and the in-service.
- Explain how you might integrate this feedback for future improvements.
Remember to account for activity and discussion time. For tips on developing PowerPoint presentations, refer to:
- Capella University Library: PowerPoint Presentations.
- Guidelines for Effective PowerPoint Presentations [PPTX].
ADDITIONAL REQUIREMENTS
- Presentation length: There is no required length; use just enough slides to address all the necessary elements. Remember to use short, concise bullet points on the slides and expand on your points in the presenter’s notes. If you use 2 or 3 slides to address each of the parts in the above example, your presentation would be 10–15 slides.
- Speaker notes: Speaker notes should reflect what you would actually say if you were delivering the presentation to an audience. Another presenter would be able to use the presentation by following the speaker notes.
- APA format: Use APA formatting for in-text citations. Include an APA-formatted reference slide at the end of your presentation.
- Number of references: Cite a minimum of 3 sources of scholarly or professional evidence to support your assertions. Resources should be no more than 5 years old.
Note: Your instructor may also use the Writing Feedback Tool to provide feedback on your writing. In the tool, click the linked resources for helpful writing information. Portfolio Prompt: Remember to save the final assessment to your ePortfolio so that you may refer to it as you complete the final Capstone course.
NURSFPX4020 Capella Assessment 3: Improvement Plan In-Service Presentation Sample Approach
This is an excerpt of the presentation, with only slide content provided. The speaker notes have been excluded.
Institutional Affiliation
- Medication error is an preventable adverse event that occurs during
Introduction
prescribing, transcribing or dispensing.
- It has escalated at the medical facility due to various factors such as workloads, inadequate training and distractions (Farzi et (2017)
- Medication errors result in patient harm, increased hospital stay, escalated medical costs or even
- Addressing this issue will help avoid unintended consequences in the long
Agenda
Agenda and Outcomes- We have conducted extensive research on Root Cause Analysis and Safety Improvement plan over the past
- Based on the obtained results, more emphasis will be channeled to proper staff training on safe medication
- Some of our key topics of interest include:
- Safety improvement
- Audience role and importance
- New skills and
- Sessions will last for 3-4 days
Agenda and Outcomes
- Outcomes
• By the end of the training, the staff will:
- Understand the appropriate strategies to avoid the common medication
- Provide effective evidence based
- Appreciate the role of teamwork and effective
- Learn new skills and
- Understand the importance of medication safety in a healthcare
Safety Improvement
Plan
- The medical facility has recorded immense medication errors over the past 8
- Addressing this issue is vital since it will:
- Reduce morbidity and mortality
- Minimize healthcare related
- Improve work
- Preserve organizational
- Promote a safe working
- Avoid lawsuits (Kasemsap, 2017)..
Safety Improvement
Plan
Below is the proposed safety plan
- Embrace health information technology to avoid human error (Hughes & Ortiz, 2015).
• Reinforce effective communication to foster collaboration.
- Increase nurse staffs to minimize
• Provide staff training to instill new competencies.
- Minimize interruption to promote
Audience’s Role and Importance
- Staff audience will help implement and drive the plan through:
- Making comments or further
- Role
- Sharing personal experience on medication
- Taking
- Helping win top management support through campaign where
- Embracing the plan
Audience’s Role and Importance
- The audience are importance because they:
- Are directly affected by the improvement
- Are integral part of the
- Their response and perception towards the plan significantly determines its success.
- By embracing their roles in the plan, the audience’s work could benefit by:
- Recording minimal medication
- Gaining credibility and trust from their
- Increasing the overall
New Process and Skills Practice
• “Five Rights” of medication administration can encourage skill development and process understanding.
- Right patient
- Right drug
- Right dose
- Right route
- Right time
- These guides are accepted and recognized for safe medication (Martyn et al., 2019).
New Process and Skills Practice
- Further processes and skill practice include:
- Role play by providers to ensure effective practice of medication
- Provide rigorous activities related to medication labels, and medication orders to stimulate critical
- Provide questions worksheets to be completed at specified
Soliciting Feedback
• Feedback can be solicited by:
- Asking for
- Conducting feedback surveys at the end of
- Performing exploratory audience
- Asking
• Integrating the feedback for future reference:
- Respond to feedbacks
- Making the necessary
- Compile the
- The presented agendas and outcomes are relatable and necessary in prevention of medication errors.
Conclusion on NURSFPX4020 Capella Assessment 3 Improvement Plan In-Service Presentation.
- The proposed improvement plan is tailored to work in the best interest of patient
- The involved audience have pertinent roles and significance that makes them more impactful in the
- Strategic processes and skills practice are necessary for effective medication
- Soliciting audience feedback is an integral process and aids in making the appropriate future improvements. NURSFPX4020 Capella Assessment #3: Improvement Plan In-Service Presentation.
References on NURSFPX4020 Capella Assessment 3 Improvement Plan In-Service Presentation.
- CDC, (2017) Medication Safety https://www.cdc.gov/medicationsafety/basics.html
- Farzi, S., Irajpour, A., Saghaei, M., & Ravaghi, H. (2017). Causes of medication errors in intensive care units from the perspective of healthcare Journal of research in pharmacy practice, 6(3), 158.
- Hughes, R. G., & Ortiz, E. (2015). Medication errors: why they happen, and how they can be prevented. Journal of infusion nursing, 28, 14-24.
- Kasemsap, (2017). The perspectives of medical errors in the health care industry. In Impact of medical errors and malpractice on health economics, quality, and patient safety (pp. 113-143). IGI Global.
- Martyn, -A., Paliadelis, P., & Perry, C. (2019). The safe administration of medication: Nursing behaviours beyond the five-rights.
- Nurse Education in Practice, 37, 109–114. https://doi.org/10.1016/j.nepr.2019.05.006
NURSFPX4020 Capella Assessment 3: Improvement Plan In-Service Presentation SCORING GUIDE
Use the scoring guide to understand how your assessment will be evaluated.
CRITERIA
- NON-PERFORMANCE
- BASIC
- PROFICIENT
- DISTINGUISHED
List clearly the purpose and goals of an in-service session for nurses.
- Does not list the purpose and goals of an in-service session for nurses.
- Lists with insufficient clarity the purpose and goals of an in-service session for nurses.
- Lists clearly the purpose and goals of an in-service session for nurses.
- Lists clearly the purpose and goals of an in-service session for nurses, with purpose and goals that are relevant and achievable within the in-service session.
Explain the need and process to improve safety outcomes related to a specific organizational issue.
- Does not describe the need and process to improve safety outcomes related to a specific organizational issue.
- Describes a safety improvement outcome, but the described need for the improvement or process to achieve improvement is unclear or irrelevant.
- Explains the need and process to improve safety outcomes related to a specific organizational issue.
- Explains the need and process to improve safety outcomes related to a specific organizational issue, with reference to specific data, evidence, or standards to support the explanation.
Explain audience’s role in and importance of making the improvement plan successful.
- Does not describe the audience’s role in and the importance of making the improvement plan successful.
- Describes the audience’s role in the improvement plan but does not clearly address how the audience is important to the success of the improvement plan.
- Explains the audience’s role and the importance of making the improvement plan successful.
- Explains the audience’s role and importance of making the improvement plan successful, using persuasive and transparent communication to improve buy-in.
Create resources or activities to encourage skill development and process understanding related to a safety improvement initiative.
- Does not list resources or activities.
- Lists resources or activities, but their relevance to skill development or process understanding related to a safety improvement initiative is unclear.
- Creates resources or activities to encourage skill development and process understanding related to a safety improvement initiative.
- Creates resources or activities to encourage skill development and process understanding related to a safety improvement initiative, explaining their value.
Communicate with nurses in a respectful and informative way that clearly presents expectations and solicits feedback on communication strategies for future improvement.
- Does not communicate with nurses in a respectful and informative way that clearly presents expectations and solicits feedback on communication strategies for future improvement.
- Communicates with nurses without clarifying expectations or soliciting feedback or does not communicate respectfully.
- Communicates with nurses in a respectful and informative way that clearly presents expectations and solicits feedback on communication strategies for future improvement.
- Communicates with nurses in a respectful and informative way that clearly presents expectations and solicits feedback on communication strategies for future improvement.
- Presentation slides and speaker notes are free from errors that impact clarity or persuasiveness.
NURSFPX4020 Capella Assessment 3 Resources:
Leadership Competencies
• American Organization of Nurse Executives. (2015). Nurse executive competencies [PDF]. Retrieved from https://www.aonl.org/nurse-executive-competencies
• The AONE nurse executive competencies may be a helpful resource as you design your presentation, especially with regard to communication and collaboration.
Evidence and Value-Based Decision Making
Zadeh, R., Sadatsafavi, H., & Xue, R. (2015). Evidence-based and value-based decision making about healthcare design: An economic evaluation of the safety and quality outcomes. HERD: Health Environments Research & Design Journal, 8(4), 58–76.
• This article presents a model for taking different decision-making approaches to improve outcomes.
Facilitating Learning
Fewster-Thuente, L. (2014). A contemporary method to teach collaboration to students. Journal of Nursing Education, 53(11), 641–645.
This article may give you some ideas for a skills practice activity to include in your Improvement Plan In-Service Presentation.
• Green, J. K., & Huntington, A. D. (2017). Online professional development for digitally differentiated nurses: An action research perspective. Nurse Education in Practice, 22, 55–62.
Green and Huntington highlight five elements that are key to effective online professional development in this article describing an action-research project involving RNs in clinical settings.
• Moradi, K., Najarkolai, A. R., & Keshmiri, F. (2016). Interprofessional teamwork education: Moving toward the patient-centered approach. The Journal of Continuing Education in Nursing, 47(10), 449–460.
The study discussed in this article involved the development of a framework of interprofessional framework competencies on which curricula and assessment tools could be based. Such an approach may be useful for you to consider as you develop your presentation.
• Rakhudu, M. A., Davhana-Maselesele, M., & Useh, U. (2016). Concept analysis of collaboration in implementing problem-based learning in nursing education. Curationis, 39(1), 1–13.
In their effort to better understand and define collaboration in terms of problem-based learning, the authors observed the increasing importance of interprofessional collaboration to nursing education and other aspects of the health care profession.
• Capella Writing Center
• Introduction to the Writing Center.
• Access the various resources in the Capella Writing Center to help you better understand and improve your writing.
Assessment 3: Improvement Plan In-Service Presentation APA Style and Format
• Capella University follows the style and formatting guidelines in the Publication Manual of the American Psychological Association, known informally as the APA manual. Refer to the Writing Center’s APA Module for tips on proper use of APA style and format.
Capella University Library
• BSN Program Library Research Guide.
• The library research guide will be useful in guiding you through the Capella University Library, offering tips for searching the literature and other references for your assessments.
PowerPoint
Refer to these helpful Campus resources for PowerPoint tips:
• Capella University Library: PowerPoint Presentations.
• Guidelines for Effective PowerPoint Presentations [PPTX].
READ MORE >>
26–33. https://doi.org/10.1016/j.profnurs.2022.05.012Tariq R. A. ...
READ MORE >>
NURSFPX4020 Capella University Safety Improvement Plan Analysis PaperMedication ...
NURSFPX4020 Capella University Safety Improvement Plan Analysis Paper
Medication Errors Root Cause Analysis and Safety Improvement Plan Example Approach
Root cause analysis (RCA) is a tool used to investigate and understand the underlying causes of patient safety incidents, such as medication errors (Ahmed et al., 2019). It helps in problem identification so that health practitioners can introduce changes that improve care quality and patient experience. Medication errors are a typical incident that requires an RCA that will ultimately produce various recommendations to reduce medication errors and improve patient safety.
The application of RCA to medication errors within a clinical care setting is critical considering the alarming numbers of increased length of stay, hospital injuries and death that adverse events have caused in American hospitals (Gates et al., 2019). For instance, according to Mazer and Nabhan (2019), at least 200,000 deaths are attributable to medication errors yearly, indicating that various root cause factors play a role in those events and are worth exploring. This report covers an RCA of ten hospitals in the US, analyzing and describing the fundamental causes and major contributors to medication errors, as well as an evidence-based plan and resources for improving patient safety.
Root Causes Of Medication Errors And Evidence-Based Solutions
When nurses, pharmacists, or physicians offer any type of healthcare service to patients, they can unknowingly inflict injury on the patient or cause adverse events such as medication errors or misdiagnosis. As per Gates et al. (2019), 10-20% of medication orders contain medication errors depending on the adverse event, for instance, delayed medicine administration.
However, Gates et al. (2019) also found out that serious medication errors make up 5% of medication administrations in the US. In the case of Delaware Community Clinic, the management reports collected over the past 30 days indicated that for every 100 medication administration cases, seven errors are experienced. This number is above the acceptable rate of medication errors.
The data was collected through direct and non-participant medication preparation and delivery observations. The non-participatory observation of medication errors yielded important information about medication errors. For example, it was observed that distractions and secondary events were among the direct causes of medication errors in the Delaware Community Clinic.
While most medication errors are preventable, they cause an array of adverse events, such as triggering new health conditions, patient injury, or, in the worst cases, death (Ibrahim et al., 2020). Medication errors also lengthen hospital stay, increases the cost of healthcare, and inflicts psychological or physical pain on the patient and their families. Medication errors in healthcare organizations reduce patient satisfaction and ultimately contribute to trust issues among nurses, physicians, and entire health organizations.
The RCA was conducted by a team of six practitioners, including a clinician, a supervisor, two quality improvement personnel and two nurses. The medication errors were recorded through nurse observations, emphasizing medication ordering and administration services. The error cases were categorized under prescription omission, wrong timing, improper usage, dose preparation and dosage, medication administration errors including extra dosage, and giving the wrong patient.
The observed incidences revealed that time, unauthorized administration, and dosage errors were the most prevalent, accounting for 17, 10 and 18 percent of the medication errors, respectively. The observations also indicated that the errors occur during periods of high activity, for instance, during shift changes and emergency calls. The RCA also showed that staff-related causes of medication errors were attributable to inadequate pharmacological knowledge.
For instance, it was observed that nurses who lacked the ideal knowledge of the ideal medication administration route were likely to cause incidences of intravenous injections. The errors were also observed to be highly associated with poor knowledge of drug pharmacological properties as well as excessive dosage. These errors were observed to be primarily caused by the complex nature of intravenous medication, which requires vast experience to deliver the drug as optimally as possible.
Notably, the nurses who made these mistakes showed a lack of in-service training among newer staff, which constrained them of the necessary knowledge to prepare and deliver the drugs. As Mazer and Nablan (2019) recommended, in-service training on pharmacology and administration of complex medicine could be an excellent approach to reducing such medication errors.
The second root cause of medication errors in the Delaware Community Clinic was a shortage of nurses, which increased the workload of nurses needed at one point in time. Interviewed nurses revealed that medication errors were highly attributable to understaffing because nurses were pressured to cover the workload. Therefore, some evidence-based solution to understaffing is employing more nurses, ensuring a smoother change of shifts, and supporting the nursing staff as much as possible (Mazer & Nabhan, 2019). For instance, during the root cause analysis, it was observed that some laboratory staff could call the physicians to collect the lab results physically.
However, the results could easily be transmitted to the physician using an electronic medical records system (EMRs). Rezaei (2019) recommends that EMRs can reduce medication errors by facilitating fast, efficient, and reliable transmission of patient information between nurses, pharmacists, laboratory technicians and the patient. Using technology to transmit necessary information, such as lab reports, could help minimize the pressure that comes with physically handling the data.
Improvement Plan
The improvement plan following this RCA will take two approaches: improving staff’s skills and knowledge and making the necessary environmental changes to minimize medication errors. The first item of the plan is to improve the hospital’s medication monitoring system to improve staff coordination and enhance prescription accuracy through various cross-checking points and communication among staff. The second improvement plan will be to train the staff to prevent medication errors, especially when administering complex medications such as intravenous injections. The training should improve the nurses’ pharmacological knowledge, especially on new drugs, contraindications, dosages, and proper administration.
Conclusion
Medication errors are associated with lengthened hospital stays, injury, increased care costs and even death. An RCA of the factors contributing to medication errors revealed important information on some of the leading causes and their potential solutions. The report indicated that nurses’ lack of skills and knowledge, followed by poor communication and distractions, are the most common cause of medication errors. Some of the evidence-based strategies for addressing the problem include the improvement of staff skills and knowledge and making the necessary environmental changes to minimize medication errors. These two solutions will provide a ground approach to minimizing medication errors in Delaware Community Hospital.
NURSFPX4020 Capella University Safety Improvement Plan Analysis Paper References
Ahmed, Z., Saada, M., Jones, A.M., & Al-Hamid, A.M. (2019). Medical errors: Healthcare professionals’ perspective at a tertiary hospital in Kuwait. PLoS ONE, 14(5), 1-14. https://doi.org/10.1371/journal.pone.0217023
Gates, P.J., Baysari, M.T., Mumford, V., Raban, M.Z. & Westbrook, J. I. (2019). Standardizing the Classification of Harm Associated with Medication Errors: The Harm Associated with Medication Error Classification (HAMEC). Drug Safety, 42, 931–939. https://doi.org/10.1007/s40264-019-00823-4
Ibrahim, O.M., Ibrahim, R.M., Meslamani, A.Z.A., & Mazrouei, N.A. (2020). Dispensing errors in community pharmacies in the United Arab Emirates: investigating incidence, types, severity, and causes. Pharmacy Practice (Granada), 18(4), 2111. https://doi.org/10.18549/PharmPract.2020.4.2111
Mazer, B.L., & Nabhan, C. (2019). Strengthening the Medical Error “Meme Pool.” Journal of General Internal Medicine, 34, 2264-2267. https://doi.org/10.1007/s11606-019-05156-7
NURSFPX4020 Capella University Root-Cause Analysis and Safety Improvement Plan Example 2
A root-cause analysis is a method of problem-solving that entails determining the primary reason for a situation or issue to stop it from happening again in the future. Investigating the root causes of safety problems and potential remedies is often part of a safety improvement plan.
Organizations wishing to increase safety and prevent accidents or incidents must apply root-cause analysis and safety improvement planning. Organizations may make their workplaces safer and more productive for both their employees and clients by recognizing and addressing the fundamental causes of issues. This paper aims to conduct a root cause analysis of an incident that risked patient safety in my health organization and develop a safety improvement plan from the analysis.
Analysis of the Root Cause
Mr. X, a 52-year-old black male, had been hospitalized for three days for treatment but was diagnosed with stage II hypertension during his inpatient stay. As part of his treatment plan, he was prescribed Lisinopril tablets, a medication used to lower blood pressure, to be taken once daily at a dosage of 10mg upon his discharge from the hospital. The medication was dispensed by a licensed pharmacist, who checked that it was the correct medication and had not expired. However, the pharmacist made a mistake and provided the patient with 20mg tablets of Lisinopril instead of the prescribed 10mg tablets.
The patient, who was also a healthcare professional, took the medication as directed and subsequently experienced severely low blood pressure and dizziness, requiring emergency care the next morning. This error occurred despite the pharmacist’s efforts to ensure the accuracy and safety of the medication. The patient received treatment at the emergency department and recovered from the adverse reaction to the medication. This incident highlights the importance of careful medication management in preventing adverse events and the need for proper training and oversight of healthcare professionals.
The nurses discovered this problem at the emergency department who, during medication reconciliation and health history building, questioned the patient’s past medical and medication history. The nurse wanted to know the reason for this unplanned readmission within 48 hours after discharge. The patient, Mr. X, was impacted by the issue or event in the scenario mentioned above. Mr. X’s extremely low blood pressure and disorientation were caused by the pharmacist’s mistake in the medication he dispensed, necessitating emergency care. As a result, Mr. X had a great deal of stress and inconvenience, and it is possible that this had a detrimental effect on his physical and mental well-being.
The error might have potentially resulted in long-term effects if it had not been caught right afterward. Patients who experience medication errors may experience adverse side effects, damage, or even death (Assiri et al., 2018). Healthcare providers must adhere to established protocols and procedures to ensure patient safety and minimize avoidable mistakes. Healthcare providers must adhere to established protocols and procedures to guarantee patient safety and minimize avoidable mistakes. Patients should be knowledgeable about their prescriptions and speak out if they have any concerns or inquiries.
Root Cause Analysis
As part of his hypertension treatment plan, Mr. X was given a prescription for Lisinopril pills at a dosage of 10mg once daily and was meant to be discharged from the hospital. A qualified pharmacist was required to dispense the drug and ensure that it was the right one and that it had not expired. However, the pharmacist misread the prescription and gave Mr. X 20mg of Lisinopril tablets rather than the 10mg tablets that were intended.
Despite the pharmacist’s best efforts to ensure the medication’s accuracy and safety, this error nonetheless happened. The usual chain of medication use in the facility is that upon the prescription of medication by the physician or an advanced practice registered nurse, the nurse should check the prescription and obtain the correct medication from the pharmacists.
In case of uncertainty, the nurse, as the professional administering the medication, should check with the prescriber to ascertain that the prescription is safe and appropriate for the patient and that all the five R’s of medication use are considered in the prescription. The pharmacists should ensure that the patient gets the right medication with the correct dose per the prescription. In cases of uncertainty, the pharmacist should check with the prescriber and professional administering the medication to prevent errors. Another role of the nurse in this system is ensuring that the patient understands their prescription and is aware of adverse effects, when to seek emergency help, and when to expect clinical improvement.
The environmental factors that played a part in this case can only be inferred from the documented evidence-based literature. In this scenario, the physical environment could have played a part in this issue because of the external distractions in the case of heavy workload in the inpatient pharmacy. Distractions from colleagues or other patients could have deterred the pharmacist from double-checking the dosage strength of Lisinopril dispensed.
The presence of a heavy workload from the high number of patient cases being handled could have played a role in this error. The inpatient pharmacy dispenses medication daily to more than five units in the hospital. Patients being discharged may be highly likely to be overlooked because of the presumed stable condition and thus might not require much attention as opposed to patients requiring emergency care and close monitoring.
The absence of automatic dispensing cabinets for patients being discharged could have influenced this medication error. Barcode medication administration (BCMA) systems could have also prevented this error by assisting the pharmacist in double-checking the prescription. BCMA and automatic dispensing cabinets can promote medication safety by ensuring that the prescription by the physician or the advanced practice registered nurse could be translated accurately to the dispensing department (Williams et al., 2021). Other technologies can also support or complement these technologies in ensuring medication safety.
The medication provided to the patient may have been incorrect due to several communication-related problems. A breakdown may have significantly influenced the circumstances leading up to this problem in communication between the prescribing doctor and the pharmacist over the appropriate dosage and frequency of the medicine.
This incident might have been caused by a communication breakdown between the pharmacist and the patient regarding the drug and how to use it properly. The strength of the medication may have been overlooked due to inadequate or unclear documentation or labeling of the drug, which could have caused confusion or misunderstanding.
Nevertheless, written or verbal communication, synchronous or asynchronous, played a critical part in this event. The presence of protocols for communication and guidelines for medication treatment was lacking in this patient’s case. These protocols can ensure accountability and empower teamwork when followed in a coordinated fashion (Russ-Jara et al., 2021). The need for collaboration, leadership, and management is thus evident from the literature.
Application of Evidence-Based Strategies
To address the issue of medication errors, healthcare organizations can implement various best practice strategies. One strategy is to use electronic prescribing systems, which provide accurate and up-to-date medication information and can reduce the risk of errors by eliminating the need for handwritten prescriptions and facilitating communication between prescribing physicians and pharmacists (Mohanna et al., 2022).
Another strategy is to conduct medication reconciliation, which involves reviewing and comparing a patient’s current medications with those prescribed at previous healthcare encounters to ensure that the patient is receiving the correct medications and dosages. Providing ongoing education and training for staff on medication administration protocols, proper labeling and documentation, and error prevention strategies can also help prevent errors (Vaismoradi et al., 2020).
Creating a culture of safety within the organization, where staff feel comfortable reporting errors and identifying potential risks, and implementing a medication error reporting system to identify patterns and trends can also contribute to preventing errors and ensuring patient safety (Mutair et al., 2021).
Our healthcare organization must regularly assess its medication management processes and identify potential areas for improvement to prevent errors (Afaya et al., 2021). According to Chui et al. (2019), addressing medication safety should be multidisciplinary and multifaceted because factors of medication errors cut across more than one discipline and profession. Therefore, these evidence-based strategies would require implementation in all stakeholder departments in our health organization.
Improvement Plan with Evidence-Based and Best-Practice Strategies
A proposed plan for this health organization will include implementing certain additional technologies, regularly training staff on medication safety, establishing an error-reporting system, and developing policies for medication safety. These strategies can help reduce the risk of errors by providing accurate and up-to-date medication information, facilitating better communication between prescribing physicians and pharmacists, reviewing and comparing a patient’s current medications with those prescribed at previous healthcare encounters, ensuring that staff has the necessary knowledge and skills to safely manage medications, establishing clear protocols for medication management, and identifying patterns and trends in medication errors to allow for targeted interventions (Mohanna et al., 2022).
Specific additional technologies required will be Computerized Physician Order entry (CPOE), BCMA, and automated dispensing cabinets. Impending these technologies would require roughly half a year owing to the lengthy process of procurement, budgetary approval, training staff on their usage, and engaging all stakeholders to evaluate outcomes. However, other strategies, such as continuous staff education, establishing error reporting systems, and policy development, could be completed in a month after stakeholder consultations.
Existing Organizational Resources
Implementing the above plan would require human, technological, and financial resources. The organization already has healthcare professionals who can implement the plan. However, additional staff in the pharmacy and technology department would make this plan more feasible because it would reduce the workload on the existing human resources.
Identify existing organizational personnel and/or resources that would help improve the implementation or outcomes of the plan. The additional resources necessary would require an electronic health record (EHR) or a computerized method of managing patient information. The institution already has an EHR that can complement the BCMA, CPOE, and automated dispensing cabinets. Most importantly, financial resources would be critical in enhancing this improvement plan. Purchasing the additional technologies, implementing them, and compensating the involved personnel could require additional funds from the institution’s supplementary budget or outside sources.
Conclusion
Root-cause analysis is an essential method for identifying the primary causes of safety issues to prevent them from occurring again in the future. In this case, a root-cause analysis was conducted on an incident in a healthcare organization where a patient was given an incorrect medication dosage, leading to adverse effects requiring emergency care. The root cause of this incident was determined to be a mistake made by the pharmacist in reading the prescription and dispensing the wrong dosage of medication.
A safety improvement plan was developed to address this issue and prevent similar incidents from occurring in the future. This plan includes strategies such as implementing an electronic prescribing system, conducting medication reconciliation, providing ongoing education and training for staff, developing clear policies and procedures for medication management, and implementing a medication error reporting system. By implementing these strategies, healthcare organizations can improve patient safety and minimize the risk of preventable medication errors.
NURSFPX4020 Capella University Safety Improvement Plan Analysis Paper References
Afaya, A., Konlan, K. D., & Kim Do, H. (2021). Improving patient safety through identifying barriers to reporting medication administration errors among nurses: an integrative review. BMC Health Services Research, 21(1), 1156. https://doi.org/10.1186/s12913-021-07187-5
Assiri, G. A., Shebl, N. A., Mahmoud, M. A., Aloudah, N., Grant, E., Aljadhey, H., & Sheikh, A. (2018). What is the epidemiology of medication errors, error-related adverse events, and risk factors for errors in adults managed in community care contexts? A systematic review of the international literature. BMJ Open, 8(5), e019101. https://doi.org/10.1136/bmjopen-2017-019101
Chui, M. A., Pohjanoksa-Mäntylä, M., & Snyder, M. E. (2019). Improving medication safety in varied health systems. Research in Social & Administrative Pharmacy: RSAP, 15(7), 811–812. https://doi.org/10.1016/j.sapharm.2019.04.012
Mohanna, Z., Kusljic, S., & Jarden, R. (2022). Investigation of interventions to reduce nurses’ medication errors in adult intensive care units: A systematic review. Australian Critical Care: Official Journal of the Confederation of Australian Critical Care Nurses, 35(4), 466–479. https://doi.org/10.1016/j.aucc.2021.05.012
Mutair, A. A., Alhumaid, S., Shamsan, A., Zaidi, A. R. Z., Mohaini, M. A., Al Mutairi, A., Rabaan, A. A., Awad, M., & Al-Omari, A. (2021). The effective strategies to avoid medication errors and improving reporting systems. Medicines (Basel, Switzerland), 8(9), 46. https://doi.org/10.3390/medicines8090046
Russ-Jara, A. L., Luckhurst, C. L., Dismore, R. A., Arthur, K. J., Ifeachor, A. P., Militello, L. G., Glassman, P. A., Zillich, A. J., & Weiner, M. (2021). Care coordination strategies and barriers during medication safety incidents: A qualitative, cognitive task analysis. Journal of General Internal Medicine, 36(8), 2212–2220. https://doi.org/10.1007/s11606-020-06386-w
Vaismoradi, M., Tella, S., A Logan, P., Khakurel, J., & Vizcaya-Moreno, F. (2020). Nurses’ adherence to patient safety principles: A systematic review. International Journal of Environmental Research and Public Health, 17(6), 2028. https://doi.org/10.3390/ijerph17062028
Williams, R., Aldakhil, R., Blandford, A., & Jani, Y. (2021). Interdisciplinary systematic review: Does alignment between system and design shape adoption and use of barcode medication administration technology? BMJ Open, 11(7), e044419. https://doi.org/10.1136/bmjopen-2020-044419
NURSFPX4020 Capella University Safety Improvement Plan Analysis Paper
For this assessment, you will develop a Word document or an online resource repository of at least 12 annotated professional or scholarly resources that you consider critical for the audience of your safety improvement plan, pertaining to medication administration, to understand or implement to ensure the success of the plan.
NURSFPX4020 Capella University Safety Improvement Plan Analysis Paper Resources:
Collaboration and Teamwork
Chard, R., & Makary, M. A. (2015). Transfer-of-care communication: Nursing best practices. AORN Journal, 102(4), 329–342.
- Consider applying some of the communications best practices highlighted in this article to how you communicate your tool kit.
Dietz, A. S., Pronovost, P. J., Mendez-Tellez, P., Wyskiel, R., Marsteller, J. A., Thompson, D. A., & Rosen, M. A. (2014). A systematic review of teamwork in the intensive care unit: What do we know about teamwork, team tasks, and improvement strategies? Journal of Critical Care, 29(6), 908–914.
- The authors discuss best practices related to teamwork and team improvement, some of which may help you think about how best to present the information in your tool kit.
Kalisch, B. J., Aebersold, M., McLaughlin, M., Tschannen, D., & Lane, S. (2015). An intervention to improve nursing teamwork using virtual simulation. Western Journal of Nursing Research, 37(2), 164–179.
- This article presents a feasibility study for use of a simulation to improve teamwork among nursing staff.
Malamed, C. (n.d.). Using wikis for learning and collaboration. ;Retrieved from http://theelearningcoach.com/elearning2-0/using-wi…
- This article may be helpful as you think about how to put together your tool kit for your assessment.
MindTools. (n.d.). How to create a wiki: Setting up a collaborative online workspace. ;Retrieved from https://www.mindtools.com/pages/article/how-to-cre…
- MindTools provides a practical overview of wikis, including their history and purpose, as well as how to build them.
BLOGS
Wolf, D. M., & Morouse, K. M. (2015). Using blogs to support informatics nurses’ curriculum needs. ;Online Journal of Nursing Informatics, ;19(2), 1–9.
- This article looks at the use of blogs and other online platforms to improve learning and communication, as well as patient care.
GOOGLE SITES
Refer to the following links to help you build your tool kit:
- G Suite Learning Center. (n.d.). ;Get started with Sites. ;Retrieved from https://gsuite.google.com/learning-center/products…
- Google. (n.d.). ;Google Sites. ;Retrieved from https://sites.google.com
- Google. (n.d.). ;Sites help. ;Retrieved from https://support.google.com/sites/?hl=en#topic=
- Resources for safety and improvement measures in geropsychiatric care. ;(n.d.). Retrieved from https://sites.google.com/view/safetyimprovementmea…
Also Read:
NURSFPX4020 Capella Assessment 3: Improvement Plan In-Service Presentation
NURS-FPX4020 Assessment 2 Root-Cause Analysis and Safety Improvement Plan.
BUILDING PROFESSIONAL EFFICACY AND VISIBILITY
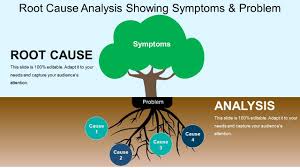
Kaminski, J. (2016). Why all nurses can/should be authors. Canadian Journal of Nursing Informatics, 11(4), 1–7.
- This editorial urges nurses to be active contributors to ongoing research, journals, blogs, and other outlets to increase visibility of their valuable perspectives on health care.
EVALUATING RESOURCES
The Library of Congress. (n.d.). Evaluating Internet resources: An annotated guide to selected resources. Retrieved from https://www.loc.gov/rr/business/beonline/selectbib…
- This Web page collects resources related to evaluating the reliability and relevance of information from electronic sources. The format of this page may also be a helpful model for the resource list you are assembling.
BUILDING PROFESSIONAL EFFICACY AND VISIBILITY
Kaminski, J. (2016). Why all nurses can/should be authors. Canadian Journal of Nursing Informatics, 11(4), 1–7.
- This editorial urges nurses to be active contributors to ongoing research, journals, blogs, and other outlets to increase visibility of their valuable perspectives on health care.
Root-Cause Analysis and Safety Improvement Plan Example
Root cause analysis (RCA) systematically and methodologically investigates an occurrence to identify the reason for a system failure that might not be apparent initially after the incident. System and personal failures can lead to patient safety risks, including medication errors (Center for Drug Evaluation & Research, 2019).
A root cause analysis was conducted to investigate an incident in the surgical postoperative unit that involved a morphine overdose. The purpose of this paper is to describe this incident, conduct a root cause analysis, and develop a safety improvement plan to prevent these occurrences in the future in the organization.
Root-Cause Analysis of Falls of Medication Errors
Charlie is a 20-year-old white female who had an emergency appendectomy three days ago due to acute appendicitis. Today, he still complains of severe pain at the incision site and the abdomen. During the review in the afternoon, his surgeon prescribed oral morphine 10mg Stat for his pain and documented that prescription in writing in the patient’s physical records. The same evening, four other patients were admitted from the operating room and post-anesthesia care unit (PACU).
RN, the day shift nurse in charge of the room, delegated the administration of morphine to a student nurse because she was attending to the new admissions. Charlie had been on IV painkillers in the first two days but showed suboptimal pain control. The student nurse picked IV morphine rarely used in the unit, and administered 10ml instead of the 10mgs prescribed by the surgeon.
The surgeon, who happened to be the head of the department of surgery, and the nurse manager in charge of the department agreed that a root cause analysis of the issue be done because there had been prior near misses in the last in the same department.
The RN discovered the issue on her hourly reviews when she noted that Charlie was becoming drowsy and confused and had vomited twice about half an hour after drug administration. The event necessitated the use of naloxone use to reverse the side effects of morphine overdose. A multidisciplinary care team was formed that monitored Charlie’s postoperative healing and recovery.
Analysis of Root Causes
The most common practice factors involved in medication errors include training, engagement, motivation, and work organization system. Interruptions commonly lead to medication errors by breaching the work organization system, thus increasing the risk of making medication errors of omission due to a break in concentrations (Schroers et al., 2022).
Possible outcomes are wrong medication, wrong dose, or wrong route in medication administration. Transitions in care provide a high risk of making medication errors. During this time, there are high chances of a break in the continuity of care, which can involve the patient medication lists.
Human factors contributing to the medication error included understaffing
READ MORE >>
Nursing 6830 Comprehensive Physical Examination TemplateSTUDENTS MAY USE THIS AS ...
Nursing 6830 Comprehensive Physical Examination Template
STUDENTS MAY USE THIS AS A TEMPLATE FOR THEIR WRITE-UP
Otterbein University Graduate Studies in Nursing
Nursing 6830 –Spring 2021
(Appendix E-3 Below E with RUBRIC APPENDIX)
Comprehensive Physical Examination
- General appearance
Include general state of health, build, and sexual development. Note posture, motor activity, and gait; dress, grooming, and personal hygiene; and any odors of body or breath. Note manner, affect, and reactions to people and environment, speech. Note state of awareness or level of consciousness.
- Measurement
Ht, Wt, BP, P, R, BMI
- Skin
– Inspect skin, hair, nails
- Head & face
– Inspect hair, scalp, skull and face
- Eye
– Check visual acuity and screen visual fields
– Note position and alignment of eyes
– Observe eyelids and inspect the sclera and conjunctiva of each eye
– Inspect cornea, iris and lens
– Extraocular muscles movement
– Pupil, size, response to light/accommodation
– Opthalmoscopic exam: red reflex, disc, vessels, retinal background
- Ear
– Inspect auricles, canals and drum (otoscope for canals and drum)
– Check acuity. If acuity diminished, check Weber and Rinne.
- Nose
– Inspect external nose – symmetry
– with nasal speculum, inspect mucosa, septum, turbinates
– palpate for tenderness of frontal and maxillary sinuses
- Mouth & throat
– Inspect lips, oral mucosa, gums, teeth, tongue, palate, tonsils and pharynx
– Note mobility of uvula as person says aaaaah
- Neck
– Inspect and palpate the cervical lymph nodes: note masses or pulsations
– Feel for deviation of trachea
– Inspect and palpate thyroid
- Back
-Inspect and palpate the spine and muscles of the back.
-Observe shoulder height for symmetry
- Posterior Thorax and Lungs
– Inspect posterior chest: skin, thorax, symmetry, movement
– Palpate: symmetrical expansion, tactile fremitus
– Percuss: lung fields, diaphragmatic excursion
– Auscultate: breath sounds (normal vs. adventitious); transmitted voice sounds if indicated
- Breasts, Axillae, and Epitrochlear Nodes
-In a woman, inspect breast with arms relaxed, then elevated, and then with hands on hips
-Inspect axillae and feel for axillary nodes. Feel for epitrochlear nodes.
-Palpate breasts (may be deferred or may do over t-shirt or gown)
- Upper Extremities
-Examine hands, arms, shoulders, neck and temporomandibular joints
-Inspect and palpate joints and check their range of motion
-Examine upper extremity muscle bulk, tone, strength, and reflexes
-Check radial and brachial pulses
- Anterior Thorax
– Inspect: skin, thorax, symmetry, movement
– Palpate: expansion, tactile fremitus
– Percuss: lung fields
– Auscultate breath sounds, transmitted voice sounds
- Cardiovascular System
– Observe for jugular venous pulsations and measure the JVP
– Inspect and palpate carotid pulsations. Listen for carotid bruits
– Inspect and palpate precordium for pulsations, heaves
– Note the location, diameter, amplitude and duration of apical pulse
– Listen at each auscultatory area with the diaphragm of the stethoscope
– Listen at the apex and the lower sternal border with the bell
– Turn person to left side while auscultating apex with bell
– Have patient sit, lean forward, and exhale while you listen at the base
- Abdomen
– Inspect: contour, symmetry, skin characteristics, umbilicus & pulsations
– Auscultate bowel sounds, aortic bruits, renal artery bruits
– Percuss abdomen. Palpate abdomen lightly, then deeply.
– Assess the liver and spleen by percussion and then palpation
– Try to feel the kidneys, and palpate aorta and its pulsations
– Percuss posteriorly over the costovertebral angles if indicated
- Lower extremities (While supine)
– Palpate femoral, popliteal, dorsalis pedis, posterior tibial pulses
– Palpate the inguinal lymph nodes.
– Inspect for lower extremity edema, discoloration, or ulcers. Palpate for pitting edema.
– Inspect joints, palpate joints, check range of motion
– Assess lower extremity muscle bulk, tone and strength, assess sensation and reflexes
– Inspect & separate toes
(Standing)
-Inspect for varicose veins
-Examine the alignment of the spine and its range of motion, the alignment of legs and feet
– Genitalia and hernia in men – defer this exam
-Observe patient’s gait and ability to walk heel-to-toe, toe walk, heel walk, hop, shallow knee bends. Romberg test and check for pronator drift
- Nervous System
– Test mental status – orientation, mood, thought process, thought content, abnormal perceptions, insight and judgment
– Test cranial nerves – (In addition to what was done in HEENT exam) check smell, strength of temporal and masseter muscles, facial movement, gag reflex and strength of trapezia and sternomastoid muscles.
– Test motor system – Cerebellar function – Rapid alternating movements, point to point movements
– Test sensory ability – pain, light touch, vibration
– Reflexes – Check deep tendon reflexes: biceps, triceps, brachioradialis, patellar, ankle, Babinski
Problem List (indicate any problems found in history or on exam)
Risk Profile (indicate risk factors that may lead to future problems)
Appendix E-3: Final Physical Exam Write Up – Grading Rubric 20 points
Partial PointsPartial PointsFull PointsClearDescriptions consistently not clear and appropriate terminology not used(1-2)
Descriptions not always clear or appropriate terminology not used
(2-3)
Descriptions are clear and appropriate terminology is used(4)
Uses concise descriptionsEither missing several descriptive elements or is overly wordy(1-2)
Either missing descriptive elements or is overly wordy
(3)
Descriptions are not overly wordy, and do not omit essential parts(4)
AccurateWrite up differs from exam performed in more than one way(1-2)
Write up differs from exam performed in one way
(3)
Write up accurately reflects the physical exam performed(4)
AppropriateDoes not include more than one component that should be performed based on the history or a comprehensive exam(1-2)
Does not include a component that should be performed based on the history or a comprehensive exam
(3)
The exam is appropriate for a comprehensive physical exam and the patient’s history(4)
Problem ListProblem list updated but more than one problem from physical exam findings is missing(1-2)
Problem list updated but at least one problem from physical exam findings is missing
(3)
Problem List updated to reflect physical exam findings(4)
READ MORE >>
Nursing Annotated Bibliography on Health Informatics PaperNursing Annotated Bibl ...
Nursing Annotated Bibliography on Health Informatics Paper
Nursing Annotated Bibliography on Health Informatics: Point-of-Care Testing
The systems of testing in healthcare can either be centralized (central laboratory) or available at the point-of-care. Point-of-care testing refers to the rapid tests that are available within the vicinity of the patient’s bed (Gous et al., 2018). Due to the demerits associated with centralized laboratories such as delayed results, delayed initiation of treatment and the distorted specimen, point-of-care testing is a strategy to minimize the gaps. Following the potential impacts the point-of-care testing has on the quality of patient care, for example reducing the diagnostic time and ensuring a rapid initiation of treatment, I choose to explore the topic.
Reliable and recommended medical databases such as the Google Scholar, PubMed and the ProQuest are used. As part of the research process, I employed the Boolean strategy, using the operators AND, OR and NOT. Hereafter are examples of the search terms I used; point-of-care testing technology, imaging technology, blood gas analysis technology and infectious disease testing and technology. The following annotated bibliography explores the role of technology in enhancing quality of care through the point-of-care testing.
Annotated Bibliography
This article explores the use of point-of-care technology in testing for Mycobacterium tuberculosis and detecting the strains resistant to Rifampin. The article discusses a new technology that improves and replaces the existing Xpert MTB/RIF. Since its endorsement in 2010 by the World Health Organization, the Xpert MTB/RIF has been used by over 130 countries as a point-of-care testing for Tuberculosis [TB] (Chakravorty et al., 2017). However, due to its demerits such as decreased sensitivity for smear negative samples, and the decreased detection for Rifampin resistant strains, a new version, an Xpert MTB/RIF Ultra was developed.
The findings of the research reveal that the Ultra has better detection for TB as compared to the Xpert. To underpin the statement, the Ultra has a 100% detection for samples as low as 25 CFU/ml. Contrarily, the Xpert detection rate lowered to 85%, 50% and 10% for 100, 50 and 25 CFU/ml (Chakravorty et al., 2017). Additionally, the overall sensitivity for Ultra is higher (87.5%) than the Xpert with a sensitivity of 81%. The Ultra’s sensitivity for smear negative samples is also high (78.9%) as compared to the Xpert (66%). The advantage of Ultra when used as a point-of-care testing includes quick results and better detection for TB (Chakravorty et al., 2017). Therefore, treatment can be initiated rapidly, and the chances for transmission are reduced; this improves care quality.
Further, the Ultra is capable of detecting mutations that are associated with Rifampin resistance, and therefore, informs the choice for therapy. The ability to detect Rifampin resistant MTB saves the patient from a prolonged exposure to unhelpful medications and the potential adverse effects of the medications; therefore, improving the safety of patient cares. An interdisciplinary team consisting of doctors and the laboratory technicians must therefore work as a team to improve the diagnosis of MTB. Even though the tests are available, organizational factors such as training on the use of the new technologies are crucial. In conclusion, the study recommends an increased embracement of the new point of care technologies to improve the diagnosis and treatment of MTB and the Rif resistant strains.
The article provides a review about the use of point-of-care ultrasound (POCUS) for patients with pulmonary pathologies in the emergency and the critical care units. Initially, before the widespread use of POCUS, chest X-Rays and chest Computed Tomography scans were popular. However due to the technical difficulties related to chest X-Rays which ultimately led to decreased accuracy of the results, and the exposure to radiation which put patients and care providers at risk of developing neoplastic mutations, a new method was required. Besides being expensive, chest CT scans also expose patients to high amounts of radiation. To solve the problems, a POCUS has been shown to be superior to lung CT scans and chest X-rays in detecting some of the lung pathologies. A POCUS is less expensive, portable, and non-invasive, provides quick results and do not expose patients to ionizing radiation (Shrestha, Weeratunga & Baker, 2018.). A POCUS is therefore safe due to the lack of radiation, and improves patient care following quick detection of lung pathologies. According to the review, a POCUS has an accuracy of 93% and 100% as compared to CXR and chest CT scans respectively, in diagnosing and ruling out interstitial syndrome (Shrestha et al., 2018).
In detection of lung consolidations, the POCUS has been shown to have a sensitivity of 90% and a specificity of 98% (Shrestha et al., 2018). Further, in low risk patients with pulmonary embolism, an ultrasound can be used as an alternative test in case the recommended CT pulmonary angiography is contraindicated. Moreover, a POCUS can be used to guide procedures for example thoracentesis. According to the review, an ultrasound guided thoracentesis has reduced risks for complications (pneumothorax) by 0-9.1% (Shrestha et al., 2018). This improves patient care and safety by preventing iatrogenic pneumothorax. Moreover, according to the review, care providers take at least 3 minutes to perform a POCUS test; this time is sufficient to make a diagnosis and to initiate a rapid treatment which grants quality care. Despite the efficacy of a POCUS, the organization must conduct a formal training that aims at improving the knowledge and skills of the care providers that perform the POCUS tests. In conclusion, the review recommends POCUS as an effective tool to diagnose pulmonary pathologies and to monitor and guide the treatments.
The article addresses a new rapid point-of-care technology that can be used even in low resource environments to test for COVID-19. The test is known as SHERLOCK (Specific High Sensitivity Enzymatic Reporter UnLOCKing). Before SHERLOCK, the US Food and Drug Administration approved the Cephid Gene Expert and the Abbot ID NOW as the two point-of-care tests. However, due to technical difficulties, expensive equipment and instruments, and the limited widespread use, there was a need to develop an affordable and an easy-to-use test. In this article, a simple test, the STOP (SHERLOCK testing in one pot) is discussed.
The test provides results in less than one hour and can be used to initiate a rapid therapy to minimize the spread of the infection. The limit of detection of the test is 100 copies of the viral genome in either a nasopharyngeal swab or in saliva. Further, the sample processing process of the test is minimal, and do not require complex equipment of instrumentation; therefore, it can be used at home or at low-resource settings even by lay users (Joung et al., 2020). Most patients report that they are uncomfortable during a nasopharyngeal swab; this test, however, can utilize saliva which is easily collected and has similar viral loads as the nasopharyngeal swabs.
Technology and chemistry are integrated to amplify the viral RNA and also to detect the resulting amplicon. Due to the rapid results (< 1-hour) and the comfort to patients (saliva used instead of a nasopharyngeal swab), patient care and satisfaction is improved. An organizational hindrance, including lack of finances to secure the required reagents can thoroughly delay the testing.
This article discusses a rapid and a less expensive point of care technology to measure blood ammonia levels in patients where the test is indicated. Elevated ammonia levels, hyper ammonia, can be detrimental. It causes encephalopathy which present as confusion, memory loss, mood changes and somnolence (Veltman et al., 2020). Hyper ammonia can also cause permanent neurologic sequelae such as brain damage. To avoid the adversities, there is a need for a rapid point of care test. The standard test requires a volume of 1-3ml of blood, and takes nearly 2-hours to produce the results; this delays the diagnosis of hyper ammonia, a detrimental condition (Veltman et al., 2020). Further, the phlebotomy is traumatic, and can cause significant hemorrhage which lead to anemia particularly in children. Moreover, the samples have to be transported to a central laboratory, a duration which takes long and during which samples can be distorted.
This study discusses an alternative point of care test that utilizes small volumes of blood and is portable. This method utilizes a sensor technology, which detects ammonia in gaseous state. This method generates results in less than 2-minutes therefore facilitate rapid interventions. Further, the test is inexpensive, and can be used even in low resource settings. The method has a first-generation device which can utilize up to 100microlitres of blood, and a second generation which uses 10-20 microliters of blood; this limits the risk for excessive blood loss via phlebotomy.
The test has been proven to be rapid and accurate, conferring speed (<2-minutes). It resembles a glucometer, easy to perform and can facilitate repeatability. Rapid diagnosis and initiation of therapy, in addition to the limited trauma and blood loss reduces mortality from hyper ammonia and improves patient care, safety and satisfaction.
Conclusion
Concerning the substitution of Xpert MTB/RIF for Ultra, better detection of MTB and Rifampin resistant strains have been reported. This has resultant effects on the diagnosis, treatment and transmission of MTB. About the use of lung ultrasound in critical care unit, the modality is inexpensive, portable, and non-invasive and have better efficacy in detecting various lung pathologies. As compared to the CXR and CT scan which expose patients to radiation, it is a safe point of care imaging modality.
The STOPCovid test confers speed (less than 1-hour); therefore, facilitating a rapid diagnosis and treatment which ultimately reduces the rate of transmission. Further, due to the detrimental nature of hyper ammonia, the portable ammonia detector (PAD) is useful in preventing the permanent neurologic sequelae of the condition. The above publications underpin the importance of technology in improving patient care and safety by improving the diagnosis and treatment of various conditions.
Despite the significance of the technologies, organizational factors play a role in their use. For example, organizations without the required technical staff experience difficulties in implementing the point-of-care technologies. Further, organizations must conduct adequate training to the staff to handle the technologies. Moreover, financial strains, as cited in the acquisition of the reagents and instruments for the SHERLOCK test derails the implementation. Even though MTB is a global health concern, the success of the point of care test is justified by the decrease in the rates of transmission. Further, reduced mortality from lung pathologies in the emergency and critical care units justifies the success of POCUS in rapid diagnosis and treatment of the pathologies. Additionally, unlike initially when the Covid-19 results would delay, the STOP-Covid test produces results in less than an hour therefore justifying its success.
References
- Chakravorty, S., Simmons, A. M., Rowneki, M., Parmar, H., Cao, Y., Ryan, J., Banada, P. P., Deshpande, S., Shenai, S., Gall, A., Glass, J., Krieswirth, B., Schumacher, S. G., Nabeta, P., Tukvadze, N., Rodrigues, C., Skrahina, A., Tagliani, E., Cirillo, D. M., … Alland, D. (2017). The new Xpert MTB/RIF Ultra: Improving detection of Mycobacterium tuberculosis and resistance to rifampin in an assay suitable for point-of-care testing. MBio, 8(4). https://doi.org/10.1128/mBio.00812-17
- Gous, N., Boeras, D. I., Cheng, B., Takle, J., Cunningham, B., & Peeling, R. W. (2018). The impact of digital technologies on point-of-care diagnostics in resource-limited settings. Expert Review of Molecular Diagnostics, 18(4), 385–397. https://doi.org/10.1080/14737159.2018.1460205
- Joung, J., Ladha, A., Saito, M., Segel, M., Bruneau, R., Huang, M.-L. W., Kim, N.-G., Yu, X., Li, J., Walker, B. D., Greninger, A. L., Jerome, K. R., Gootenberg, J. S., Abudayyeh, O. O., & Zhang, F. (2020). Point-of-care testing for COVID-19 using SHERLOCK diagnostics. MedRxiv?: The Preprint Server for Health Sciences. https://doi.org/10.1101/2020.05.04.20091231
- Shrestha, G. S., Weeratunga, D., & Baker, K. (2018). Point-of-Care Lung Ultrasound in Critically ill Patients. Reviews on Recent Clinical Trials, 13(1), 15–26. https://doi.org/10.2174/1574887112666170911125750
- Veltman, T. R., Tsai, C. J., Gomez-Ospina, N., Kanan, M. W., & Chu, G. (2020). Point-of-care analysis of blood ammonia with a gas-phase sensor. ACS Sensors, 5(8), 2415–2421. https://doi.org/10.1021/acssensors.0c00480
READ MORE >>
Landing a nursing job straight out of college can be challenging. A good nursing ...
Landing a nursing job straight out of college can be challenging. A good nursing capstone project on your resume shows initiative and can give you an edge over other applicants. But coming up with unique and intriguing nursing capstone project ideas is easier said than done.
In this complete guide, we’ll cover everything you need to know about developing standout capstone nursing projects, from understanding what they are to generating creative topic ideas across nursing specializations. Let’s get started!
What is the Nursing Capstone Project?
A nursing capstone project is a final-year assignment that allows students to demonstrate competency in clinical practice. It requires conducting independent research on a healthcare-related issue to propose an evidence-based solution.
Capstone project writing takes various forms, including research proposals, quality improvement initiatives, community health promotion programs, education plans, or systematic literature reviews. The central aim is to address a problem that is meaningful to current nursing practice.
Capstones assess the capacity to synthesize classroom and clinical learning into recommendations that enhance patient outcomes. They also evaluate skills in critical inquiry, using quality evidence, and effectively presenting key learnings.
Why Capstone Projects Are Important for Nursing Students
Undertaking an independent capstone lays solid foundations for professional and academic growth in four key ways:
Develops Crucial Research Abilities
From performing literature reviews to data analysis, capstones build vital skills for continuous learning throughout a nursing career. Evaluating research and distinguishing high-quality evidence is central to nursing practice.
Cultivates Problem-Solving Skills
Determining creative solutions to complex patient issues is central to quality care. Capstones teach logical and analytical thinking to make evidence-based clinical judgments.
Strengthens Written and Oral Communication
Conveying research professionally is imperative for patient safety. Capstones provide opportunities to produce scholarly papers and deliver engaging presentations to hone these skills.
Provides a Competitive Edge
Outstanding projects attract positive faculty recommendations for graduate school and convey career dedication to employers.
Difference between a Nursing Capstone Project and a Nursing Thesis
Before selecting a topic, recognizing distinctions between nursing capstones versus theses lays strong foundations. Theses demand in-depth investigations into a focused research problem. Capstones incorporate broader literature reviews on a practice area to recommend an initiative.
While research-oriented master’s theses aim to generate new nursing knowledge, capstones demonstrate the ability to apply existing evidence to real clinical settings.
Useful Tips When Choosing Great Nursing Capstone Ideas
An eye-catching topic aligned with personal and professional aspirations kickstarts strong capstone projects. Consider these pointers:
- Select issues connected to your desired career specialization. Picking neonatal ICU concepts builds NICU prospects.
- Identify problems needing solutions through nursing news sites and journals. Underexplored issues position you as an innovator.
- Draw inspiration from clinical observations revealing patient care obstacles. Address challenges you’ve personally witnessed.
- Review prior outstanding projects for engageable topics and structure expectations. Build on alumni capstone ideas.
- Use course lectures and textbooks pointing to therapy areas needing advancements. Instructors highlight promising themes.
- Ensure substantial research exists to support recommendations. Seek issues with sufficient evidence available.
- Pick narrow, focused topics, allowing in-depth investigation within limitations. Broad concepts become unmanageable.
- Verify capacity to access settings and data sources essential for proposed projects. Consider feasibility constraints.
- Determine projects addressing problems meaningful to patient outcomes over personal interests alone. Select issues with genuine practice impacts.
- Receive professor input on initial topic concepts through early discussions. Faculty can refine ideas needing honing.
The Potential Sources to Get Creative BSN Capstone Project Ideas
Nursing News Articles: Journals like JAN or AJN provide awareness of challenges needing solutions.
Peer-Reviewed Nursing Journals: PubMed delivers abstracts on cutting-edge and specialty interventions prime for exploration.
Clinical Rounds: Clinical observations reveal obstacles detrimentally impacting patients suitable for projects.
Nursing Capstone Papers from Past Classes: Outstanding alumni capstones indicate engageable medical issues and structure expectations.
Class Notes and Material: Course material signposts therapy areas needing enhancements for safer quality care.
The Best Capstone Project Ideas for Nursing
Now, let’s explore winning topics across major nursing concentrations:
General Nursing Capstone Project Ideas
- Evaluating Nurse Staffing Levels on Patient Mortality
- Reducing Pressure Injuries Through Patient Turning Protocols
- Discharge Educational Resources for Improved Care Transitions
- Palliative Models for Enhanced End-of-Life Care
- Cultural Competence Modules for Diverse Populations
- Analyzing Patient Satisfaction Across Hospital Units
- Evidence-Based Fall Prevention Interventions for Older Adults
- Pain Management Solutions for the Opioid Crisis
- Triage Protocol Revisions Through Application of Telehealth Tech
- Health Literacy Strategies for Care Plan Adherence
- Remote Patient Monitoring for Chronic Disease Management
- Reducing Alarm Fatigue Through Customizable Monitoring Systems
- Rehospitalization Risk Factors for Adult Medicine Patients
- Antibiotic Stewardship for Combating Resistant Infections
- Transitional Care Packages to Reduce Readmissions
- RN Delegation Decisions Using Evidence-Based Practice Models
- Stress-Reduction Programs for Improved Nurse Wellbeing
- Evaluation Tools Assessing Heart Failure Self-care Abilities
- Analyzing EHR Systems to Improve Clinical Workflow Efficiency
- Volunteer Programs Expanding Community Health Service Access
Nursing Capstone Project Ideas for Mental Health
- Art Therapy Impact on Veterans with PTSD
- Pet Therapy for Geriatric Depression Management
- CBT-Based Substance Abuse Prevention Programs for Teens
- Suicide Risk Screening Tools for College Campuses
- Nurse Practitioner-led group Therapy for Bipolar Patients
- Reducing Seclusion/Restraint Use Through De-Escalation Plans
- Anxiety/Depression Care Models for Low-Income Communities
- Music Listening Effects on Schizophrenia Symptoms
- Peer Support Programs for Borderline Personality Recovery
- Nature Exposure Influence on Pediatric ADHD Outcomes
- Telepsychiatry to Expand Rural Access to Care
- Evaluating Dementia Caregiver Burden
- Smartphone CBT Apps for Reducing OCD Severity
- Analyzing Factors in Psych Nurse Burnout
- Implementing WRAP Plans for Client Crisis Prevention
- Animal-Assisted Activities on Outpatient Satisfaction
- Horticultural Therapy for Improved Mood Regulation
- Dance/Movement Therapy for Childhood Trauma
- MDMA-Assisted Treatment for Severe PTSD
- Psychedelics Role In Anxiety and Depression
Medical Surgery Capstone Project Ideas
- Analyzing Post-op Delirium Risk Factors
- Surgical Safety Checklists for Error Reduction
- Enhanced Recovery Pathways for Colorectal Surgeries
- ICU Diaries Impact on Family Member Anxiety
- Surgical Site Infection Prevention Strategies
- Patient Acuity Systems for Effective Workforce Utilization
- Ultrasound-Guided IV Insertion Success Rates
- Evidence-Based Obesity Models Impacting Surgical Outcomes
- Preoperative Carbohydrate Loading for Positive Results
- Robotic Surgery Techniques Transforming Care
- Healing Touch Effects on Post-Mastectomy Patients
- Alarm Management Solutions on Telemetry Units
- Identifying Risk Factors for Unplanned Extubations
- Multimodal Analgesia Models for Orthopedic Pain
- Analyzing Impacts of 12-Hour Shifts on Errors
- Palliative Surgery Options for End-Stage Cancer Patients
- Family Presence During Resuscitation Policies
- Triage Protocol Revisions Through 5-Level ESA System
- Temporary Abdominal Closure Techniques for Trauma
- Internal Bleeding Risk With Anticoagulant Therapies
Health Promotion Nursing Capstone Ideas
- Worksite Wellness Plans for Health Behavior Change
- Community Gardens Addressing Nutrition Inequities
- Culturally Tailored Diabetes Prevention Programs
- Faith-Based Initiatives for Hypertension Awareness
- HPV Vaccination Drives Through School Systems
- Tobacco Cessation Social Media Campaigns
- Safe Sex Educational Resources for Teen Pregnancy Prevention
- Analyzing the Effectiveness of Heart Disease Screening Tools
- Home Visiting Models to Reduce Infant Mortality Rates
- Volunteer Doula Support Roles in Childbirth
- Micronutrient Deficiencies in Impoverished Communities
- Comprehensive Sex Ed Curriculums for LGBTQ+ Youth
- Farmers Market PDAs Strengthening WIC Impacts
- Community Paramedicine Home Visits for Elder Falls Risk
- Culturally Responsive Preventative Care in Hispanic Populations
- Faith Community Partnerships for Health Equity
- Food Rx Programs to Address Obesity
- Park Prescriptions for Chronic Disease Self-Management
- Peer Modeling and Social Support for Breastfeeding Rates
- Analyzing the Effectiveness of Worksite Wellness Incentives
Nursing Leadership Capstone Project Ideas
- Shared Governance Frameworks for Retention
- Nursing Advocacy Through Professional Organizations
- Succession Planning Models for Nurse Managers
- Analyzing Impacts of Staffing Ratios on Outcomes
- Diversity Training Programs for Cultural Competence
- Mentorship Role Efficacy in Onboarding Processes
- Staff Engagement Strategies for Magnet Designation
- Microsystems Training Improving Frontline Leadership
- Ethical Decision-Making Models for Rising Concerns
- Product Evaluation Frameworks for Technology Adoption
- Cost-Benefit Analysis of Turnover Prevention Incentives
- RN Continuing Education Tracking Systems
- Strategic Analysis of Work Environment Factors
- PR Campaigns Showcasing Nursing’s Societal Value
- Policy Evaluation Frameworks for Advocacy Planning
- Caring Science Integration in Shared Governance
- Budget Optimization Models for Tight Fiscal Situations
- Productivity Dashboard Revisions Aligned With Culture
- Analyzing Virtual Training Platform User Experiences
- Transition to Practice Curriculums for Graduates
Capstone Project Topics on Nursing Burnout
- Nurse Preceptor Support Roles in Resilience Building
- Self-Care Action Plans for Enhanced Coping Abilities
- Pet Therapy Influence on Compassion Fatigue
- MBSR Techniques to Combat Workplace Stress
- Massage Therapy for ICU Nurse Anxiety/Fatigue
- Conflict Management Training for Internal Incivility
- Analyzing Impacts of Nurse-Patient Ratios
- Peer Support Programs for Secondary Trauma
- Smartphone Apps Measuring Resilience and Burnout
- Coping Strategy Resources for Nursing Students
- Mandated Limits on Consecutive Shift Hours
- Shared Leadership Models and Wellbeing Outcomes
- Volunteer Programs Impacting Occupational Joy
- Confidence Training Interventions for New Nurses
- Analyzing Moral Distress Situations in Critical Care
- Nature Exposure for Restorative Respite Breaks
- Anonymous Reporting Systems for Ethical Issues
- Nursing Code of Ethics Integration into Practice
- Debriefing Practices Addressing Compassion Fatigue
- Quantitative Analyses of Turnover Cost Savings
Patient Falls Nursing Capstone Project Ideas
- Post-Fall Debriefing Resources to Cut Recurrences
- Analyzing High-Risk Medications in Gerontology
- Temporary Bed Alarms Policies Upon Admission
- Video Monitoring Ethics in Long-Term Care
- Enhanced Visual Representations of Fall Risk Factors
- Family-Engaged Fall Prevention Model Testing
- Volunteer Assistance Programs on Unsteady Patients
- Quantitative Cost Analyses for Fall-Related Injuries
- Bedside Shift Report Influence on Reporting Rates
- Multifactorial Fall Risk Assessment Scale Analysis
- Analyzing Nursing Documentation on Precautions
- Hourly Rounding Schedules for Maximum Effectiveness
- Enhanced Discharge Education on Home Modifications
- Fall Agreement Contracts with Cognitively Impaired
- Communication Boards for Individualized Care Plans
- Terminal Cleaning Checklists Preventing Reoccurrences
- Quantitative Review of Fall Rates Across Specialties
- Staff In-Service Fall Prevention Training Persistence Testing
- High-Fidelity Fall Simulation Impacts on Confidence
- Analyzing Missed Nursing Care Related to Falls
Women’s Health Capstone Project Ideas
- Doula Support Access Through Community Partnerships
- Analyzing Postpartum Readmission Diagnoses
- Quantifying Undocumented Prenatal Care Barriers
- Nurse Leadership in Reproductive Justice Initiatives
- Volunteer Crisis Pregnancy Center Role Efficacy
- Pap Smear Reminder Systems via Patient Portals
- Faith Community Models for Postpartum Depression Support
- Pump Access Expansion Policies for Breastfeeding Mothers
- Midwifery Integration Frameworks in Hospitals
- Volunteer Doula Impact on Birth Satisfaction
- Centering Pregnancy Influence on Infant Mortality Disparities
- Music Therapy Addressing Fetal Heart Rate Variability
- Telemental Health for High-Risk Antepartum Patients
- Quantifying Nursing Knowledge on Lactation Complications
- Analyzing Cultural Sensitivity in Women’s Health Education
- Papaya Seed Impact on Essentializing Postpartum Bleeding
- Increased Raw Vegetable Prevalence in WIC Offerings
- Volunteer Roles Expanding HPV Vaccination Access
- Nurse Leadership in Promoting Evidence-Based Birth Plans
- Volunteer Postpartum Support through Textline Services
Nursing Informatics Capstone Project Ideas
- Dashboards for Streamlined Handoff Communication
- Securing Mobile Device Data Through Encryption
- Workflow Redesign for Enhanced EHR Experience
- Simulation Training for Smooth EMR Transitions
- Analyzing Virtual Rounding Impacts on Collaboration
- Blockchain Protocols Safeguarding Health Data Exchange
- Patient Portal Effectiveness for Care Engagement
- Cloud Computing Models Maximizing Data Storage
- Workflow Obstacle Identification Through Shadow Charting
- Natural Language Processing in Clinical Documentation
- Alarm Recognition and Response Tracking Systems
- Quantifying Impacts of Downtime Workarounds
- IoT Integration Frameworks Across Continuums
- BYOD Security Policy Recommendations
- RN EHR Proficiency Testing Models
- Augmented Reality Uses in Nurse Training Curriculums
- Implementing RFID for Asset Visibility and Control
- Dashboards Centralizing Critical Information
- Sensor Tech Integration Protocols Across Settings
- Analyzing Telehealth Nursing Competency Gaps
Pediatric Nursing Capstone Project Topics
- Asthma Action Plans Tailored to Health Literacy
- Quantifying Impacts of Nurse Understaffing on Errors
- Clowning Therapy Influence on Hospital Anxiety
- Pet-assisted Therapy on Pain Management
- VolunteerReader Programs Boosting Empathy/Optimism
- Pediatric Discharge Bundle Testing for Central Lines
- Child Life Specialist Impact on ED Patient Flow Efficiency
- Hemodialysis Nursing Documentation Analysis
- Spanish Language Resources for Optimal Family Education
- Parent Training on Safe Sleep Positioning for Infants
- Analyzing Cultural Factors in Sickle Cell Pain Assessments
- Music Therapy to Reduce Pre-MRI Anxiety
- Enhanced Cooling Therapy Post Cardiac Arrest
- Patient Navigation Models Bridging Access Barriers
- Emergency Triage Protocol Revisions for Pediatrics
- District School Nurse Impacts on Chronic Absenteeism
- Communication Boards for Nonverbal Children
- Volunteer-based Literacy Programs Combating Toxic Stress
- Oral Rehydration Protocol Testing for Decreased Admissions
- Anti-Bullying Policies Protecting LGBTQ Youth
Managed Nursing Care Topic Ideas
- Preventable ED Visits Among Medicaid Populations
- Impacts of Social Determinant Screenings
- Analyzing Prior Authorization Denial Rates by Plan Type
- Emergency Hotspotting Targeting Super-Utilizers
- Community Health Worker Home Visiting for Utilization Cuts
- Member Retention Strategies Based on Satisfaction Surveys
- Revenue Reinvestment Models Expanding Value-Based Care
- Analyzing Linkages Between Claims Data and Outcomes
- Culturally Tailored Wellness Resources for At-Risk Members
- Secure Messaging for Personalized Preventative Reminders
- Incentivization Models for Lifestyle Change Adherence
- Depression Screening Rates Across Various Settings
- Nurse Triage Lines Reducing PCP Appointment Demand
- Patient Portal Adoption Strategies
- Post-Discharge Medication Reconciliation for Readmission Reduction
- Analyzing Social Support Access and Chronic Disease Burden
- Community Care Team Impact on Key Utilization Indicators
- Patient-Centered Medical Home Transformation Guidance
- Evidence-Based Standards for Care Manager Caseloads
- Medication Therapy Management Value Demonstration
Emergency Nursing Capstone Project Ideas
- Family Presence Policies for Cardiac Arrests
- Dementia Sensory Solutions on Behavioral Disturbance
- Analyzing Time to Pain Med Administration By Arrival Mode
- Mandated Nurse Ratios Based on Seasonal Volume Fluctuations
- Code Sepsis Compliance Strategies
- Geriatric Hip Fracture Clinical Pathways
- Volunteer Doula Support for Miscarrying Mothers
- Telemental Health for Enhanced Psych Consults
- Cultural Competency Training on Implicit Bias Awareness
- RN Delegation Decisions in Resource-Limited Settings
- Reducing 911 Overuse Through Community Health Access Points
- Alternate Destination Protocols Based on Necessity Factors
- Reducing Adverse Drug Events
- Analyzing Capacity Prediction Model Accuracy
- Volunteer Doula Support Access Expansion
- Community Paramedicine Impact on Super Utilizers
- Smart Triage Algorithms for Patient Acuity
- Quantifying Impacts of Boarding on Clinical Outcomes
- Caregiver Support Resources for Frequent Callers
- Pediatric Disaster Preparedness Competency Evaluation
Nursing Leadership Project Ideas
- Shared Governance Frameworks for Retention
- Nursing Advocacy Through Professional Organizations
- Succession Planning Models for Nurse Managers
- Analyzing Impacts of Staffing Ratios on Outcomes
- Diversity Training Programs for Cultural Competence
- Mentorship Role Efficacy in Onboarding Processes
- Staff Engagement Strategies for Magnet Designation
- Microsystems Training Improving Frontline Leadership
- Ethical Decision-Making Models for Rising Concerns
- Product Evaluation Frameworks for Technology Adoption
- Cost-Benefit Analysis of Turnover Prevention Incentives
- RN Continuing Education Tracking Systems
- Strategic Analysis of Work Environment Factors
- PR Campaigns Showcasing Nursing’s Societal Value
- Policy Evaluation Frameworks for Advocacy Planning
- Caring Science Integration in Shared Governance
- Budget Optimization Models for Tight Fiscal Situations
- Productivity Dashboard Revisions Aligned With Culture
- Analyzing Virtual Training Platform User Experiences
- Transition to Practice Curriculums for Graduates
Oncology Nursing Capstone Project Ideas
- Analyzing Impacts of Nurse Understaffing on Errors
- Cultural Competency Training on Care Inequities
- Massage Therapy Influence on Chemo Symptoms
- Pet Therapy for Improved Emotional Wellbeing
- Volunteer Reader Programs Addressing Isolation
- Evidence-Based Scalp Cooling for Alopecia Prevention
- Advanced Care Planning Resources Across Settings
- Music Therapy Addressing Post-Mastectomy Pain
- Support Groups for Enhanced Psychosocial Care
- Analyzing Delays in Lung Cancer Screening
- Palliative Sedation Therapy Ethics Analysis
- Smartphone Apps for Symptom Reporting/Tracking
- Volunteer Doula Role in End-of-Life Comfort
- Pediatric Early Phase Clinical Trial Nursing Competencies
- Camp Volunteer Impact on Pediatric Resilience
- Patient Navigation Strategies By Demographic Factors
- MBSR Techniques to Address Secondary Trauma
- Nature Imagery for Procedural Pain Management
- Analyzing Genetic Testing Access Barriers
- Transitional Care Intervention Testing
Final Words
Outstanding nursing capstone projects pave pathways for professional success through honing crucial skills. Selecting novel concepts demonstrates dedication by investigating challenges meaningful to enhancing practice. A wealth of inspirational ideas are available through academic journals, clinical observations, alumni papers, and lectures.
Consider connections to intended career arcs when deciding on topics for maximum relevance. Seek issues offering opportunities to take on thought leader positioning by probing creative concepts.
Through synthesizing evidence and logical translation of research into realistic recommendations, capstones provide opportunities to grow critical reasoning abilities imperative for impactful patient advocacy.
The nursing capstone is a final assignment assessing your capacity to merge clinician competencies with a nursing education scholarship. Seize this chance to shine by picking a unique, intriguing concept aligned with your aspirations.
READ MORE >>