Our Previous Samples
As a nursing student, the journey toward becoming a compassionate and skilled he ...
As a nursing student, the journey toward becoming a compassionate and skilled healthcare professional is filled with challenges, triumphs, and moments of self-reflection. Along this path, many students find solace and strength in prayer, seeking guidance, wisdom, and grace from a higher power.
Let’s explore various prayers that nursing students may turn to during their educational journey, each focusing on a specific aspect of their personal and professional growth.
A Prayer for Nursing Students
A nursing student’s prayer is a personal conversation with God, expressing their hopes, fears, and aspirations as they embark on their educational journey. One such prayer may be:
“Dear Lord, as I begin my nursing education, I pray for the strength to persevere through the challenges ahead. Grant me the wisdom to learn and grow, the compassion to care for others, and the courage to face my fears. Help me to remember that my purpose is to serve You by serving others and guide me in becoming the best nurse I can be. Amen.”
This prayer acknowledges the difficulties of nursing school while reaffirming the student’s commitment to their calling.
Prayer for Nurses
Prayers for nurses are not limited to those in the nursing profession; they are often offered by patients, families, and communities who recognize nurses’ vital role in healthcare. A prayer for nurses may be:
“Heavenly Father, we thank You for the selfless dedication and tireless efforts of our nurses. Please watch over them as they care for the sick and suffering, and grant them the strength, wisdom, and compassion they need to carry out their sacred work. Protect them from harm, both physical and emotional, and bless them abundantly for their service. Amen.”
This prayer acknowledges nurses’ sacrifices and asks for divine protection and blessing.
A Nursing Student’s Prayer Before the Examination
Examinations are critical to nursing education, testing students’ knowledge and skills in a high-pressure environment. Before an exam, a nursing student may pray:
“Dear God, as I prepare to take this examination, I ask for Your guidance and peace. Calm my anxious thoughts and help me to focus on the task at hand. Give me the clarity of mind to recall what I have learned and the wisdom to apply it correctly. I trust in Your plan for my life and know that, with Your help, I can overcome any challenge. Amen.”
This prayer seeks divine assistance in achieving academic success while acknowledging the student’s trust in God’s plan for their life.
A Nursing Student’s Prayer for Strength
Nursing school can be physically, mentally, and emotionally demanding, and students may need extra strength to persevere. A prayer for strength may be:
“Almighty Father, I come to You today feeling weary and overwhelmed. The demands of nursing school have taken their toll, and I am in need of Your strength to carry on. Fill me with Your energy and vitality, and help me to find the courage and determination to keep going, even when the path seems long and difficult. Remind me that I am never alone and that, with You by my side, I can accomplish anything. Amen.”
This prayer expresses the student’s struggles while seeking divine strength and support.
A Nursing Student’s Prayer for Compassion
Compassion is a core value of nursing, and students must learn to cultivate empathy and understanding for their patients. A prayer for compassion may be:
“Loving God, as I learn to care for others, I pray that You would fill my heart with compassion. Help me to see each patient as a unique individual, created in Your image and worthy of love and respect. Give me the patience to listen, the gentleness to comfort, and the wisdom to understand the needs of those in my care. May my hands be an extension of Your healing touch, and may my presence bring peace and solace to those who are suffering. Amen.”
This prayer seeks divine assistance in developing the emotional intelligence and empathy needed to provide compassionate care.
Nurses Prayer for Divine Protection
Nursing can be demanding and sometimes dangerous; students may seek divine protection as they learn to care for others. A prayer for protection may be:
“Heavenly Father, as I train to serve others in the nursing profession, I ask for Your divine protection. Watch over me as I care for the sick and vulnerable, and keep me safe from harm, both physical and emotional. Give me the courage to face the challenges and risks of this work, and help me to trust in Your love and care. Surround me with Your angels, and guide me in the path of righteousness. Amen.”
This prayer acknowledges the inherent risks of nursing while seeking God’s protection and guidance.
A Nursing Student’s Prayer for Wisdom
Nursing requires academic knowledge, practical skills, and sound judgment, and students must continually seek wisdom in their studies and practice. A prayer for wisdom may be:
“Almighty God, as I learn the art and science of nursing, I pray for the gift of wisdom. Help me to discern the best course of action in each situation, and give me the knowledge and understanding to make sound decisions. Guide my thoughts and actions, and help me to apply the principles of compassionate care in all that I do. May Your wisdom be my constant companion, both in the classroom and at the bedside. Amen.”
This prayer recognizes the importance of wisdom in nursing and seeks divine guidance in developing this essential quality.
A Nursing Student’s Prayer for Guidance
The path to becoming a nurse can be filled with uncertainty and difficult decisions, and students may seek God’s guidance as they navigate their educational journey. A prayer for guidance may be:
“Dear Lord, as I journey through nursing school, I ask for Your guidance and direction. Help me to discern Your will for my life and to follow the path You have chosen for me. Give me clarity of purpose and the courage to pursue my calling, even when the way seems unclear. Lead me in the way of truth and righteousness, and help me to trust in Your plan for my future. Amen.”
This prayer seeks divine guidance and clarity in uncertainty, acknowledging the student’s trust in God’s plan for their life.
A Nursing Student’s Prayer for Patience
Patience is vital for nurses, who must often deal with challenging patients, families, and situations. A prayer for patience may be:
“Heavenly Father, as I learn to care for others, I pray for the gift of patience. Help me to remain calm and composed, even in the face of frustration or adversity. Give me the grace to listen attentively, to speak gently, and to act with kindness and understanding. May my presence be a source of comfort and reassurance to those in my care, and may I always reflect Your love and compassion. Amen.”
This prayer seeks divine assistance in cultivating the patience and self-control needed to provide effective and compassionate care.
A Nursing Student’s Prayer in Difficult Times
Nursing students may face many challenges and hardships during their educational journey, from academic struggles to personal crises. In these difficult times, they may pray for comfort and strength. A prayer in difficult times may be:
“Dear God, I come to You today feeling overwhelmed and discouraged. The challenges of nursing school have tested my faith and my resolve, and I am in need of Your comfort and strength. Help me to remember that You are with me always, and that no trial is too great to overcome with Your help. Give me the courage to persevere, the wisdom to seek help when needed, and the peace that passes all understanding. I trust in Your love and care, now and always. Amen.”
This prayer expresses the student’s struggles while seeking divine comfort, strength, and peace amid adversity.
A Nursing Student’s Prayer for Endurance
Nursing school can be a long journey, requiring great endurance and perseverance. A prayer for endurance may be:
“Almighty Father, as I continue on this path to becoming a nurse, I pray for the gift of endurance. Give me the strength to keep going, even when I feel like giving up. Help me to stay focused on my goals and to trust in Your plan for my life. Renew my energy and my passion for this work, and help me to find joy and purpose in each day. May I run with perseverance the race that is set before me, keeping my eyes fixed on You. Amen.”
This prayer seeks divine strength and renewal in the face of the long and challenging nursing education journey.
Nurses Prayer for Peace
Nursing can be stressful and emotionally taxing, and students may seek God’s peace as they learn to care for others. A prayer for peace may be:
“Heavenly Father, as I learn to serve others in the nursing profession, I pray for Your peace to fill my heart and mind. Help me to let go of my worries and fears, and to trust in Your love and care. Give me the serenity to accept the things I cannot change, the courage to change the things I can, and the wisdom to know the difference. May Your peace be my constant companion, guiding me through the challenges and joys of this work. Amen.”
This prayer seeks divine peace and serenity in the face of the stresses and uncertainties of nursing.
A Nursing Student’s Prayer for Patients
As nursing students learn to care for patients, they may pray for their physical, emotional, and spiritual well-being. A prayer for patients may be:
“Dear Lord, I lift up to You the patients in my care. I pray for Your healing touch to be upon them, and for Your love to surround them. Give them strength to face their challenges, courage to fight their battles, and peace in the midst of their struggles. Help me to be a compassionate and skillful caregiver, and to reflect Your love and light to all those I serve. May each patient know that they are loved and valued, and may they find hope and comfort in Your presence. Amen.”
This prayer intercedes on behalf of patients, seeking divine healing, love, and comfort for those in need.
A Nursing Student’s Prayer for Colleagues
Nursing students often rely on the support and collaboration of their colleagues to succeed in their studies and practice. A prayer for colleagues may be:
“Almighty God, I thank You for the gift of my fellow nursing students and colleagues. I pray that You would bless them with strength, wisdom, and compassion as they learn and grow in this profession. Help us to support and encourage one another, to share our knowledge and skills, and to work together in harmony and unity. May we be a reflection of Your love and grace to each other and to all those we serve. Amen.”
This prayer seeks divine blessing and support for the student’s colleagues, recognizing the importance of collaboration and mutual support in nursing education.
READ MORE >>
Nutritional Self Analysis Sample PaperBMI & Hamwi:BMI = or BMI = * 703 = ...
Nutritional Self Analysis Sample Paper
BMI & Hamwi:
BMI = or BMI = * 703 = * 703 = *703
BMI = 0.02601 * 703 = 18.288 (Weir & Jan, 2019)
Hamwi = 106 lb for first 5ft + 6lb for each additional inch (male) or 100 lb for first 5ft + 5lb for each additional inch (female) (Brochetti et al., 2020)
Hamwi = 100lb + 5*2= 100lb + 10lb = 110lb
According to the Center for Diseases Control and Prevention, my BMI weight status is underweight, since any weight below 18.5 is classified as underweight. 18.5 to 24.9 is considered as healthy weight (Weir & Jan, 2019). By the Hamwi formula, since I live a sedentary lifestyle and do not exercise at all, my daily caloric intake should be (ideal weight * 11) = 110lb * 11 = 1210 calories per day (Brochetti et al., 2020).
Food Diary
Intake Spreadsheet for 5th September, 2021
FOODSCaloriesCarbsFatProteinCholestSodiumSugarsFiberBreakfastStarbucks- Oatmeal with Brown Sugar, 1.5 cup28557g4.5g7.5g0mg0mg19.5g6gStarbucks Coffee- Grande Cinnamon Dolce Latte-Skinny, 32fl oz26038g0g24g10mg320mg34g0gLunchMcdonald’s-fries, large, 1 order44463g22g6g0mg350mg0g6gMcdonald’s- Mcdouble Cheeseburger, 10.6 oz (2 sandwiches 302g)78066g38g46g130mg1700mg14g4gCoke-Zero 16oz, 16oz00g0g0g0mg57mg0g0gDinnerCoke Zero- Beverage, 24 ounces00g0g0g0mg80mg0g0gCajun shrimp-Shrimp, 1 container (10 shrimp)92022g76g46g319mg0mg0g0gGeneric-Bell Pepper-Orange, 1 cup7020g0g4g0mg8mg12mg4gTotal2759266 g140.5 g133.5 g459 mg2515mg79.5mg20gFoodSaturated (g)Polyunsaturated (g)Monounsaturated (g) Trans (g)Potassium (mg)Vitamin A %Vitamin C(mg)Calcium (mg)Iron (mg)BreakfastStarbucks- Oatmeal with Brown Sugar, 1.5 cup0.20006100833Starbucks Coffee- Grande Cinnamon Dolce Latte-Skinny, 32fl oz0.30005806208LunchMcdonald’s-fries, large, 1 order1.980.221.98000201.08Mcdonald’s- Mcdouble Cheeseburger, 10.6 oz (2 sandwiches 302g)4.4000.6200001602.34Coke-Zero 16oz, 16oz000000000DinnerCoke Zero- Beverage, 24 ounces000000000Cajun shrimp-Shrimp, 1 container (10 shrimp)10002590007003.6Generic-Bell Pepper-Orange, 1 cup0.070.1860.0080251187226.180.51Total7.950.8362.0082.583160187232.191648.53
Intake Spreadsheet for 6th September, 2021
FOODSCaloriesCarbsFatProteinCholestSodiumSugarsFiberBreakfastPancake, Plain, Prepared (3 items- 5 in. in diameter)187.7433.5911.517.5944.86333.663.650.76Syrup, Maple (1 tablespoon)52.3213.20.010.0102.4213.380Bread, Pumpkin Loaf (2 slices)233.0820.263.431.9512.66113.129.370.64LunchAPPLEBEE’S Mozzarella Sticks (2 pieces)202.247.365.844.7810.58266.120.80.69APPLEBEE’S French Fries (0.5 serving)275.518.786.241.590.49293.5601.84Lettuce, Iceberg, Chopped (2 cups chopped)15.41.650.100.405.61.070. 67Cheese, Cheddar, Shredded (0.125 cup)68.880.359.387.0230.01174.420.140CULINARY SECRETS dressing, vinaigrette, Italian Herb (3 ounces)283.51.8918.900754.9700Cucumber, Peeled 3 tablespoon30.350.020.200.350.240.14Potatoes, Mashed, Garlic (2 ounces)40.564.470.0500.073.30.420.56DinnerKELLOGG’S RAISIN BRAN Cereal 2 cups570681.67.603142810.6WHITE WAVE SILK PURE ALMOND Almondmilk, Vanilla 1.5 cup135172.720152172BUGLES Nacho Cheese Flavor 1.5 cup180.4513.556.790.770233.060.770SnacksRUFFLES Potato Chips, Cheddar & Sour (4 ounces)64044357068804Reeces Big with reece pieces (40.2 g)0241250020.71.7Total 268.45113.5746.5498.673334.5895.5422.93FoodSaturated (g)Polyunsaturated (g)Monounsaturated (g) Trans (g)Potassium (mg)Vitamin A IU) (µg)Vitamin C mgCalcium mgIron mgBreakfastPancake, Plain, Prepared (3 items- 5 in. in diameter)2.513.401.900100.34148.940.26166.881.39Syrup, Maple (1 tablespoon)000041.720020.120.04Bread, Pumpkin Loaf (2 slices)0.871.170.98064.6626.730.9715.440.69LunchAPPLEBEE’S Mozzarella Sticks (2 pieces)2.161.491.370.1434.78138.2609.010.49APPLEBEE’S French Fries (0.5 serving)1.082.781.590.06257.5400.359.030.47Lettuce, Iceberg, Chopped (2 cups chopped)0.010.040077.57276.31.569.70.25Cheese, Cheddar, Shredded (0.125 cup)5.940.292.67027.66283.050203.660.17CULINARY SECRETS dressing, vinaigrette, Italian Herb (3 ounces)2.8300000000Cucumber, Peeled 3 tablespoon000024.6211.760.542.350.06Potatoes, Mashed, Garlic (2 ounces)0.020.020098.688.733.658.060.17DinnerKELLOGG’S RAISIN BRAN Cereal 2 cups00005837530286.73WHITE WAVE SILK PURE ALMOND Almondmilk, Vanilla 1.5 cup00.71.706250204520.74BUGLES Nacho Cheese Flavor 1.5 cup5.2800022.580000SnacksRUFFLES Potato Chips, Cheddar & Sour (4 ounces)4.713.613.60962014.601.07Reeces Big with reece pieces (40.2 g)5000000320.7Total30.423.4923.810.22357.152148.7721.93956.2512.97
Intake Spreadsheet for 7th September, 2021
FOODSCaloriesCarbsFatProteinCholestSodiumSugarsFiberBreakfastBread, Banana Nut 2 slices281.7555.952.937.690.47294.3920.372.98LunchBeef, Rib Eye Steak, Boneless, Lip-On, Separable Lean Only, Trimmed to 1/8” Fat, All Grades, Grilled 128 g266.43013.5535.6101.1475.5300CAMPBELL’S Beans, Baked, Brown Sugar & Bacon Flavor 1.5 cup3225841269452818SnacksOROWEAT Bread, Sweet Hawaiian 2 slices1121734017860.7Ham, Sliced, Prepackaged or Deli 0.5 slices,4 ¼ in. squares240.140.783.448.63252.650.240Cheese, Gouda 0.5 ounces102.920.657.767.0532.35232.170.650Mayonnaise, Regular 1 teaspoon15.660.021.730.030.9914.80.030Salad Dressing, Ranch 2.5 ounces239.23.2425.280.7314.76510.882.680WHITE WAVE SILK PURE ALMOND Almondmilk, Original 0.5 cups, 250 ml3231.240.60723.70.7RUFFLES Potato Chips, Cheddar & Sour Cream 28g159.0413.8510.851.970227.1400.97Broccoli 2 cups, chopped32.976.060.352.59030.051.532.35Total1587.97157.9171.4775.7164.342832.6163.225.7FoodSaturated (g)Polyunsaturated (g)Monounsaturated (g) Trans (g)Potassium (mg)Vitamin A IU) (µg)Vitamin C (mg)Calcium (mg)Iron (mg)BreakfastBread, Banana Nut0.350.941.350351.96424.372.8779.372.55LunchBeef, Rib Eye Steak, Boneless, Lip-On, Separable Lean Only, Trimmed to 1/8” Fat, All Grades, Grilled5.360.86.250.68378.877.6608.983.26CAMPBELL’S Beans, Baked, Brown Sugar & Bacon Flavor3000000822.86SnacksOROWEAT Bread, Sweet Hawaiian0200000421.06Ham, Sliced, Prepackaged or Deli0.230.130.260133.96001.070.11Cheese, Gouda4.970.172.3034.5159.630198.470.09Mayonnaise, Regular0.291.050.3700.441.700.160Salad Dressing, Ranch3.9714.585.40.3436.2736.87015.860.19WHITE WAVE SILK PURE ALMOND Almondmilk, Original00.230.7707725201520.34RUFFLES Potato Chips, Cheddar & Sour Cream1.464.464.460316.0704.7200.34Broccoli0.060.020.020287.54566.9181.1842.750.68Total19.6924.3821.181.021616.611449.1488.77622.6611.48
Analysis
Nutrients Recommended Dietary Allowances5/09/20216/09/20217/09/2021Carbohydrates (g)202.0 – 292.0266268.45157.91Fat (g)40.0 – 70.0140.5113.5771.47Protein (g)43.54 g133.546.5475.7Fiber (g)25 g2022.9325.7Sugar (g)N/A79.595.5463.2Saturated (g)< 18 g7.9530.419.69PolyunsaturatedN/A0.83623.4924.38MonounsaturatedN/A2.00823.8121.18TransN/A2.580.21.02CholesterolN/A45998.67164.34Sodium mg150025153334.582832.61Potassium mg470031602357.151616.61Vitamin A µg7001872148.771449.14Vitamin C mg75232.121.9388.77Calcium mg1000916956.25622.66Iron mg1848.531211.48
Most of my calories come from carbohydrates, as evidenced in the spreadsheets analysis above. For all three days, my intake of carbohydrates was higher than for either proteins or fats.
Nutritional Analysis of Food Diary
The recommended daily allowance of carbohydrates is 202.0 – 292.0 g (Van Elswyk, Weatherford & McNeill, 2018). For 5th and 6th September, my intake was within the RDA while on 7th the intake was below the RDA. I could include generic sweet corn in my diet since it is a rich source of carbohydrate. Carbohydrates are the main source of energy for cell metabolism and cellular respiration (Childs, Calder & Miles, 2019; Großkopf & Simm, 2020). Glucose is the primary source of energy for neurons in the brain, skeletal muscles and myocardial cells.
The RDA of fat is 40.0 – 70.0g. For all three days, my fat intake exceeded the RDA, particularly due to fast foods such as fries, cheeseburger and shrimps (Van Elswyk, Weatherford & McNeill, 2018). Also culinary dressing salad was another rich source of fat. These foods are replaceable by low-fat options such as boiled potatoes, boiled shrimp and fresh fruits/vegetables. Fats provide energy for metabolism in times of starvation.
The RDA for proteins is 43.54 g (Van Elswyk, Weatherford & McNeill, 2018). On all three days, my intake exceeded the RDA. The high protein was from cheeseburger, beef, ham and latte coffee. These foods are replaceable with plant-protein such as peanuts, green grams and beans. Proteins play major roles in the formation of cellular structures and components such as the microtubules and microfilaments that maintain the cell’s architecture (Childs, Calder & Miles, 2019). They are referred to as the body-building foods.
The RDA for fiber is 25 g (Van Elswyk, Weatherford & McNeill, 2018). For all three days, my intake was within the recommended limits. Fiber is significant in digestion in that it adds bulk to the food within the gut lumen, promoting peristalsis, enhancing passage of food material along the digestive tract (Childs, Calder & Miles, 2019). This prevents constipation.
There is currently no recommended daily allowance of sugar.
The RDA for saturated fat is <18g (Van Elswyk, Weatherford & McNeill, 2018). My intake exceeded the RDA on 6th and 7th of September. The main source of saturated fat was ham, cheese, MacDonald cheeseburger and Bugle’s Nacho. These are all processed foods that could be replaced by freshly-prepared home-made meals such as wet-fried beef and beans. Plant fat such as olive oil has trace amounts of saturated fat. Saturated fats are used to monitor the risk for cardiovascular disease (Childs, Calder & Miles, 2019). Too much saturated fat results in high serum levels of low-density lipoprotein (LDL), which increase the likelihood of arteriosclerosis, atherosclerosis and deep venous thrombosis (Bonnacio et al., 2020).
There is presently no RDA for polyunsaturated fat. Polyunsaturated fats are important for nerve function, muscle strength, brain health and blood clotting.
At present there is no RDA for monounsaturated fat. Monounsaturated fats are significant in assisting an individual to lose weight and protect against heart disease (Childs, Calder & Miles, 2019). Monounsaturated fats lower the LDL that is linked to cardiovascular disease
No RDA exists for cholesterol at present. Cholesterol is a precursor molecule in the synthesis of steroid hormones such as testosterone, estrogen, aldosterone and epiandosterone (Childs, Calder & Miles, 2019). Cholesterol is also crucial in the synthesis of Vitamin D in presence of sunlight.
The RDA for sodium is 1500mg (Van Elswyk, Weatherford & McNeill, 2018). All three days intake exceeded the RDA. The primary sources of high sodium were Ruffle’s potato chips, mayonnaise, salad dressing, nacho, culinary secret dressing and McDonald’s cheeseburger. Appropriate substitutions include generic baked beans, boiled generic potatoes and olive oil dressing. Sodium assists to maintain the water-electrolyte balance in the body and generation plus transmission of signals in nerves and muscles (Childs, Calder & Miles, 2019).
The RDA for potassium is 4700mg (Van Elswyk, Weatherford & McNeill, 2018). All daily intakes were within the recommended limit. Potassium assists to offset the harmful effects of sodium on blood pressure (Childs, Calder & Miles, 2019). Potassium is also significant in generation and propagation of impulses in nerves and muscles, as well as maintaining the heartbeat.
The RDA for vitamin A is 700 µg (Van Elswyk, Weatherford & McNeill, 2018). The intake was below the recommended on 5th and above the RDA on 6th and 7th. Alternative food options to improve Vitamin A include yellow, leafy and red vegetables/fruits such as carrots, sweet potatoes, red pepper, spinach, mangoes, papaya and apricots. Vitamin A maintains normal vision, a healthy immune system and reproductive function (Childs, Calder & Miles, 2019). It also enhances the functioning of the heart, kidneys and lungs.
The RDA for vitamin C is 75 mg (Van Elswyk, Weatherford & McNeill, 2018). The intake exceeded the recommended on 5th and 7th and was below on 6th. Sources of vitamin C are citrus fruits, peppers, strawberries, blackcurrants, broccoli, potatoes and Brussels sprouts. Vitamin C is useful in maintaining healthy skin, bones/cartilage, and blood vessels (Childs, Calder & Miles, 2019). It protects cells and keeps them healthy by promoting the functioning of white blood cells.
The RDA for calcium is 1000 mg (Van Elswyk, Weatherford & McNeill, 2018). All intakes were within the recommended limit. Calcium assists to maintain strong bones and teeth (Childs, Calder & Miles, 2019). It is also useful in muscle contraction and transmission of nerve signals across synapses.
The RDA for iron is 18 mg (Van Elswyk, Weatherford & McNeill, 2018). The intake exceeded the limit on 5th September. This was due to Starbucks coffee latte, Starbucks oatmeal with brown sugar and broccoli. Alternative sources are spinach, tofu and lentils. Iron is utilized to form hemoglobin and myoglobin that transport oxygen in blood and muscle, respectively (Childs, Calder & Miles, 2019).
Diet Plan
My dietary needs comprise of meals that will assist me to add weight. These should be primarily proteins, fats and some carbohydrates. For breakfast I will include bread with banana nut, protein powder, spinach and white wave silk pure almond. My lunch will consist of large plain hamburger, ketchup and buddy’s bar-b-q sauce while dinner will include Bison, Ribeye and Baked Beans. Bread with banana nut, protein powder, hamburger, Bison and baked beans are important sources of protein that are body-building foods, assisting in gaining body mass. Spinach will provide vitamin A which is essential for normal vision, and fiber that prevents constipation.
Goals
By October 31st, I will walk around my estate for 30 minutes three times a week. By October 31st, I will gain 4lbs body weight at a rate of 1lb per week. By September 30th I will increase my daily water intake to 3 liters per day.
Implementation Strategies and Obstacles
I will set a reminder on my personal computer and mobile device at 1800 hrs to begin the walking on Tuesdays, Thursdays and Saturdays. I will take the meals rich in protein as per my diet plan for breakfast, lunch and supper daily. I will purchase a water bottle that will carry drinking water when am at work or walking.
In taking the walk, the major obstacle could be phone calls from work, friends or family, requiring my immediate attention. The obstacle to taking protein-rich meals in gaining weight is lack of appetite due to monotonous diet options. Drinking water could be limited by forgetfulness, particularly when am not thirsty.
Conclusion
In a nutshell, the majority of our diet plans fall short of the recommended daily allowance, by either too much or too little of a nutrient. This information is significant in clinical practice as it will enable me to calculate the appropriate dietary requirements of particular patients according to their dietary needs.
References
- Brochetti, A. M., Brose, S. W., Kuemmel, A. M., Dang, D. J., & Bourbeau, D. J. (2020). Interdisciplinary bodyweight management program for persons with SCI. The journal of spinal cord medicine, 43(1), 24-30. https://www.tandfonline.com/doi/abs/10.1080/10790268.2018.1547860
- Bonnacio, M., Di Castelnuovo, A. F., Costanzo, S., De Curtis, A., Persichillo, M., Cerletti, C., Donati, M. B., de Gaetano,G. & Iacoviello, L. (2020). Abstract 49: Consumption of Ultra-processed Foods and Beverages is Associated With Increased Risk of Cardiovascular Mortality in the Moli-sani Study Cohort. Circulation, 141(1). https://doi.org/10.1161/circ.141.suppl_1.49
- Childs, C. E., Calder, P. C., & Miles, E. A. (2019). Diet and immune function. https://www.mdpi.com/2072-6643/11/8/1933
- Großkopf, A. & Simm, A. (2020). Carbohydrates in nutrition: friend or foe?. Z Gerontol Geriat 53, 290–294. https://doi.org/10.1007/s00391-020-01726-1
- Van Elswyk, M. E., Weatherford, C. A., & McNeill, S. H. (2018). A systematic review of renal health in healthy individuals associated with protein intake above the US recommended daily allowance in randomized controlled trials and observational studies. Advances in Nutrition, 9(4), 404-418.
- Weir, C. B., & Jan, A. (2019). BMI classification percentile and cut off points. https://europepmc.org/article/nbk/nbk541070
READ MORE >>
Writing a cohesive one-page essay can be a challenge. With little room for extra ...
Writing a cohesive one-page essay can be a challenge. With little room for extraneous details, every word must add value to your discussion. Careful planning, efficient writing, and ruthless editing are essential. This academic writing guide covers simple steps to help you write a focused one-pager worth an A.
How Many Words Is a 1-Page Essay?
Before outlining the main points, it helps to know precisely how much copy you need to produce. Word counts differ slightly based on format specifications:
Single-spaced
With standard margins (1 inch top/bottom, 1.25 inches left/right), a single-spaced document in 12-point Times New Roman font yields approximately 550 words per page. Since you need one page total, aim for 550 words.
Double-spaced
The same document, double-spaced, produces about 275 words per page. So, for your one-page, double-spaced essay, strive for 275 well-chosen words.
Steps for Writing a One-Page Paper (The Writing Process)
Writing an essay involves specific key steps. Here are helpful tips to help you craft a well-structured one-page paper that will engage the reader:
Step 1 – Avoid Distractions
Before attempting one-page brilliance, eliminate diversions. Turn off social media, silence your phone, and close redundant browser tabs. You need complete focus.
Also, ensure you have sufficient time. Rushing the writing process results in sloppy arguments and grammatical errors. Give yourself an hour or two of uninterrupted time to outline thoughts, summarize them, and compose draft paragraphs smoothly.
Step 2 – Set the Right Atmosphere
Find a quiet, comfortable workspace. I prefer a tidy desk in my bedroom, furthest from the buzz of household activity. Ensure adequate lighting, ventilate the room, gather paper and pens, and keep your favorite coffee mug handy.
Making minor environmental adjustments keeps you alert and oriented on the essay, not tuning out your surroundings. Also, consider sound: some writers require absolute silence to channel ideas, while others prefer instrumental or natural background noise. Figure out what environment fuels your best work.
Step 3 – Make Sure You Understand the Topic
Before asserting arguments about a topic, verify full comprehension. Carefully read the essay prompt or assignment guidelines several times, noting keywords and assessing exactly what the instructor expects you to discuss.
Jot down initial reactions to the topic. Then, conduct any limited research permitted, seeking obscure facets you may not have initially considered. Outline potential supporting points. Vet sources for credibility. Precision now prevents vague rambling later.
Step 4 – Develop a Thesis Statement
With a firm grasp on expectations around the topic, synthesize your position in a single thesis statement. Articulating the paper’s primary argument upfront provides direction.
A thesis statement:
- Clearly conveys the essay’s main point
- Provides a specific, debatable stance regarding the topic
- Uses assertive language
- Fits into one sentence neatly
Here’s a sample thesis statement:
“The nursing shortage can be addressed through an approach of increased funding, improved workplace culture, and recruitment efforts aimed at bringing more men and minorities into the profession.“
Some key things this sample thesis statement does:
- Identifies the specific issue being addressed: the nursing shortage
- Proposes a solution to the problem that includes multiple components (increased funding, improved workplace culture, diversified recruitment)
- Implies that this solution will help address the nursing shortage without overstating or making unsupported claims
- Focuses on a specific and current issue relevant to the nursing field
Step 5 – Create an Outline
Now, roughly map how you’ll support your sharp thesis. An organized essay structure ensures the final draft flows logically.
An effective one-page essay outline:
- Introduces the topic and thesis in 2-3 sentences
- Develops 3-4 key points to substantiate the thesis
- Concludes by circling back to the thesis with a closing thought
Given length constraints, categorize points by priority, pursuing only the most compelling.
Step 6 – Write Your Paragraphs
With your thesis set and supporting points outlined, it’s time to start writing.
Compose the introductory paragraph, hooking interest while forecasting arguments. Next, use each outline heading to launch supporting paragraphs expanding the point. Show, don’t merely tell, through data examples or anecdotes.
Paragraph order matters—sequence points from most to least persuasive. Wrap up with a summary, revisiting your original thesis to book a discussion.
Throughout the draft, check the word count periodically to ensure concise delivery. Every sentence must build the case efficiently.
Step 7 – Edit and Proofread
Polish the draft with ruthless editing. As famed writer Stephen King advised: “Kill your darlings, kill your darlings, even when it breaks your egocentric little scribbler’s heart, kill your darlings.”
Scrutinize each section, cutting filler phrases that blunt meaning. Eliminate wasted words diluting your message. Kill those darlings! Pare sections down to hard-hitting essence through revision.
Next, proofread for glaring errors in grammar, syntax, or citation format. Read every sentence aloud, even better if possible. Verbalizing text helps catch awkward phrasing.
Finally, give the draft one last skim, confirming your thesis still rings clearly with properly cited evidence tightly aligned. Make any final tweaks necessary.
Then, celebrate one powerful page articulating an informed, convincing stance worth an impressive grade.
Checklist
To recap advice for acing a one-page essay:
- Verify the precise word count needed for the format
- Focus on a dedicated environment
- Grasp topic expectations fully
- Craft a strong thesis statement
- Outline supporting discussion points
- Compose sharp supporting paragraphs citing evidence
- Refine draft relentlessly
Follow these steps for writing excellence even with severe space limitations. A flexible approach sets you up to shine.
Wrapping Up: How to Write a 1 Page Essay or Paper
This guide outlines a strategy to help you research, plan, organize, write, and refine a superior short-form essay worth top academic accolades. Test these methods when assigned your next paper. Implementing an efficient workflow keeps the process smooth while producing skillful writing, proving your scholastic prowess within restrictive parameters.
Aim not just to vaguely address complex themes in isolation but to showcase the connection of concepts across case examples. Creativity and precision reconcile competing demands. Trust the process; it works! I believe your brilliant ideas deserve to be heard, so send convincing messages to educate about issues resonating with your unique worldview.
Meanwhile
Crafting a compelling one-page essay can be both an art and a science, blending creativity with structured technique. It’s an academic exercise frequently assigned to check one’s ability to formulate their thoughts concisely and persuasively. A well-written one-page essay, typically spanning 200 to 250 words and organized into 2 to 3 paragraphs, serves as a testament to your ability to communicate effectively, engaging the reader from the introductory paragraph to the conclusion.
However, even experienced writers can stumble over the complexities of not only writing but also editing and proofreading a perfect essay. From ensuring your introduction and conclusion are impactful to structuring supporting paragraphs that convey your arguments clearly, each step requires careful planning and attention to detail. Moreover, grammatical errors, spelling mistakes, and overlooking formatting guidelines are pitfalls that can detract from the credibility of your academic paper, regardless of its insightful content.
This is where our essay writing service steps in. Tailored for nursing students across the United States, our service is designed to elevate your academic writing, ensuring it resonates across various spheres of life, including public health, nursing, and psychology. Our team of experts, familiar with every nuance from the title page to the final sentence of the conclusion, is here to offer helpful tips, essay examples, and personalized assistance.
Whether you’re struggling with organizing your thoughts, crafting an effective essay outline, or navigating the nuances of academic writing, our service provides comprehensive support. From proofreading to editing, we ensure your essay is free of spelling and grammar errors, adhering to the highest standards of grammatical accuracy.
Engage our writing service to transform your personal essay writing experience. We not only offer essay samples but also empower you with the tools and knowledge to improve your writing process. Let us help you in writing the introduction, developing body paragraphs that engage the reader, and concluding with a powerful statement that underscores your argument.
Remember, a teacher or professor is not just assessing your ability to write but also your capacity to think critically and present your ideas compellingly. Don’t let the challenges of academic paper writing hold you back. With our expertise, you can craft essays that stand out, reflecting your unique perspective and academic rigor.
Let’s make your next one-page essay not just an assignment but a milestone in your academic journey.
FAQs
How Many Words Is 1 Page Single-Spaced?
A single-spaced page typically contains around 550 words. This allows for denser text with no extra spacing between lines.
How Many Words Is a 1-Page Essay or Paper?
A 1 page essay contains approximately 550 words when single-spaced or 275 words when double-spaced.
How Many Words Is 1 Page Double-Spaced?
A standard 1-page essay or paper double-spaced will contain approximately 275 words. Double-spacing inserts an extra blank line between each line of text.
How Many Words Is 1 Page Handwritten?
When handwritten, a single page can hold 100-200 words, depending on the handwriting size. Smaller writing will allow more words to fit.
How Many Paragraphs Is 1 Page?
On average, a single page will have 3-5 paragraphs of text. Paragraph length and spacing determine the exact number.
How Many Sentences Is 1 Page?
Expect to find about 30 sentences on a full page. The number of sentences contained depends on the average sentence length.
Which Font Produces More Pages?
Times New Roman, Cambria, and Calibri use proportional spacing so more words fit per line. On the other hand, Arial, Verdana, and Tahoma use monospacing, so fewer words fit.
How Long Does It Take to Write a 1-Page Essay?
For a 1 page double-spaced essay with around 275 words, an experienced writer should spend 30-60 minutes writing, depending on topic familiarity. For a writer who can type 40 words per minute, writing the essay will take about 12.5 minutes on average.
READ MORE >>
Opinion essays allow writers to express unique viewpoints while convincing reade ...
Opinion essays allow writers to express unique viewpoints while convincing readers to agree with their perspectives. Choosing a compelling and current topic is key to engaging your audience and structuring a discussion-worthy debate.
This article will outline amazing and thought-provoking opinion essay ideas across various categories.
How to Select the Best Opinion Essay Topic
Selecting the best opinion paper topic involves a thoughtful process to ensure the chosen subject aligns with your interests, engages your audience, and allows for a well-supported argument. Here are some steps to guide you in choosing the most suitable topic for your opinion essay:
- Identify Your Interests: Begin by considering topics that genuinely interest you. Passion for the subject will not only make the writing process more enjoyable but also result in a more compelling and authentic essay.
- Consider Your Audience: Think about the perspective of your intended audience. Choose a topic that resonates with them and addresses issues or concerns they may find relevant or thought-provoking.
- Research Potential Topics: Conduct preliminary research on the topics you’re considering. Ensure there is enough information available to support your argument and provide a well-rounded view of the subject.
- Check Relevance: Assess the relevance of the topic to the current societal context or the context within which your essay will be read. A timely and pertinent subject can capture more attention.
- Define Your Stance: Clearly understand your own stance on the topic. Your essay should present a strong, well-supported opinion. Avoid topics where your viewpoint may be unclear or where you feel indifferent.
- Consider Controversy: Controversial topics often generate more interest and discussion. However, be mindful of your audience and the context in which you are presenting your essay.
- Brainstorm Supporting Points: Ensure there are multiple supporting points for your chosen topic. A robust opinion essay requires a well-rounded argument with evidence and examples.
- Avoid Overused Topics: While popular topics may be tempting, try to avoid those that have been extensively covered unless you have a unique angle or fresh perspective to bring to the discussion.
A List of 200+ Opinion Essay Topics
Opinion essays provide an excellent platform for individuals to express their thoughts, beliefs, and perspectives on a wide range of subjects. This list of 200+ opinion essay topics covers diverse areas, inviting writers to explore and share their viewpoints on issues that matter.
Best Opinion Essay Topics for 2024
- The Benefits and Drawbacks of Integrating Telemedicine in Nursing Care
- Ethical Considerations in End-of-Life Care: Exploring Alternatives to the Death Penalty
- Standardized Tests for Nursing Licensure: Assessing Their Efficacy and Impact
- The Role of Technology in Nursing Education: Advantages and Challenges
- Public Transportation Accessibility for Nurses: Improving Healthcare Access
- Gender Discrimination in Nursing: Addressing Challenges and Promoting Equity
- The Impact of Air Pollution on Nurse Health: Mitigation Strategies
- Should Nursing Students Be Allowed to Administer Medications? Examining the Debate
- Incorporating Foreign Language Education in Nursing Curricula: Benefits and Implementation Challenges
- The Influence of Extracurricular Activities on Nursing Student Well-being
- Nurses’ Role in Addressing Domestic Violence: Challenges and Support
- The Importance of Romantic Relationships in Nursing: Balancing Personal and Professional Life
- Energy Drinks Consumption Among Nurses: Health Risks and Awareness
- African American Representation in Nursing: Promoting Diversity and Inclusion
- The Role of Nurses in World War II: Lessons Learned and Impact on Modern Nursing Practice
Good Opinion Writing Topics
- The Pros and Cons of Nursing Students Grading Their Teachers
- Financial Literacy Education for Nurses: Bridging the Gap
- Cognitive Behavioral Therapy in Nursing Practice: Effectiveness and Applications
- Parenting Styles and Their Impact on Nurses’ Work-Life Balance
- Influence of Pop Culture on Nursing Trends and Patient Care
- Exploring the Role of Nurses in Space Exploration Missions
- Public Health Initiatives and Their Impact on Nursing Practice
- Light Pollution and its Effects on Nurses’ Sleep Patterns
- Human Trafficking: Nurses as Advocates for Victims
- Should Children Be Allowed to Visit Patients in Hospitals? Perspectives and Policies
- Eating Disorders Among Nurses: Prevention and Support
- Crafting a Narrative Essay on a Nurse’s Journey in Healthcare
- Descriptive Essay: A Day in the Life of a Nurse Practitioner
- Exploring Science Fiction’s Influence on Nursing Education and Innovation
- The Nursing Profession: Challenges and Opportunities
Easy Opinion Essay Topics
- Should Nurses Have Access to Healthcare Insurance? Exploring Coverage Options
- Domestic Violence Awareness: Why Every Nurse Should Advocate
- The Role of Women in Nursing: Past, Present, and Future
- Should Plastic Be Banned in Healthcare Settings? Examining Alternatives
- Nuclear Energy in Healthcare Facilities: Risks and Benefits
- Assessing the Healthcare System: What Works and What Needs Improvement
- The Importance of Mental Health Support for Nurses: Breaking the Stigma
- Promoting Freedom of Speech Among Nurses: Balancing Professionalism and Advocacy
- Sharing Thoughts and Opinions: Fostering Open Communication in Nursing Teams
- Overcoming Writer’s Block: Strategies for Nurse Writers
- The Impact of Traditional Schooling on Nursing Education: Innovations Needed
- Should the Government Regulate Nurse-Patient Ratios? Exploring Policy Debates
- Personal Experiences in Nursing: How They Shape Professional Identity
- The French Revolution and Its Influence on Modern Nursing Ideals
- Nurses as Advocates for Environmental Health: Addressing Climate Change
Opinion Essay Topics for High School Students
- The Benefits and Drawbacks of Standardized Tests: Students’ Perspectives
- Should College Students Have Access to Mental Health Services? Discussing Support Options
- Exploring the Role of Technology in High School Education: Enhancing Learning or Distracting?
- Public Transportation Access for High School Students: Improving Accessibility
- Gender Discrimination in High School Sports: Promoting Equity
- The Impact of the Industrial Revolution on Modern Education Systems
- Cold War Ideologies and Their Influence on High School History Curriculum
- Air Pollution Around High Schools: Awareness and Action
- Should High School Students Be Allowed to Choose Their Foreign Language Courses?
- The Importance of Extracurricular Activities for High School Students: Balancing Academics and Personal Growth
- Addressing Health Insurance Gaps for High School Students: Ensuring Coverage for All
- Promoting Awareness of Domestic Violence Among High School Students: Education and Prevention
- Navigating Romantic Relationships in High School: Understanding Consent and Boundaries
- The Effects of Energy Drinks on High School Students’ Health: Educating for Safe Consumption
- African American Representation in High School Curriculum: Recognizing Contributions and Challenges
Opinion Topics in History
- The Evolution of Nursing: From Florence Nightingale to Modern Times
- Nursing’s Contribution to Public Health Throughout History
- The Impact of Wars on the Nursing Profession
- Historical Perspectives on Nursing Education: Challenges and Progress
- Epidemics and Pandemics: Nurses on the Frontlines Throughout History
- The Role of Nurses in the History of Medical Discoveries
- Nursing Practices in Ancient Civilizations: A Comparative Analysis
- Historical Perspectives on Midwifery and Women’s Health
- The Influence of Religious and Cultural Beliefs on Historical Nursing Practices
- Pioneering Nurses in History: Unsung Heroes
- The Evolution of Nursing Uniforms and Attire
- Nurses in the Civil Rights Movement: Advocacy and Activism
- Historical Advances in Surgical Nursing Techniques
- The Impact of Historical Healthcare Policies on Nursing Practice
- Nurses’ Roles in Historical Public Health Campaigns
Personal Opinion Essay Topics
- My Journey into Nursing: Personal Reflections
- Balancing Empathy and Professionalism: Personal Challenges in Nursing
- The Role of Personal Values in Ethical Decision-Making for Nurses
- My Perspective on the Future of Nursing Education
- The Impact of Personal Experiences on Patient Care
- Personal Strategies for Maintaining Well-being in Nursing
- Navigating Cultural Competence in My Nursing Practice
- Overcoming Challenges: My Experience with Nurse Burnout
- Personal Reflections on the Importance of Teamwork in Nursing
- My View on the Use of Technology in Nursing
- The Significance of Lifelong Learning in My Nursing Career
- The Role of Nurses as Advocates: My Personal Commitment
- My Thoughts on Integrating Complementary Therapies in Nursing
- Personal Perspectives on the Nurse-Patient Relationship
- Nursing Leadership: My Vision for Positive Change
Environment Opinion Topics
- The Environmental Impact of Healthcare Practices: A Nursing Perspective
- Nurses as Advocates for Sustainable Healthcare
- The Role of Nurses in Addressing Climate Change Health Impacts
- Sustainable Nursing: Reducing Waste in Healthcare Settings
- The Impact of Environmental Factors on Public Health Nursing
- Nurses’ Involvement in Environmental Health Education
- Green Hospitals: Nurses Leading the Way to Sustainability
- Addressing Environmental Injustices in Nursing Practice
- The Role of Nurses in Disaster Preparedness for Environmental Events
- Nurses’ Contributions to Eco-Friendly Healthcare Initiatives
- Integrating Environmental Health into Nursing Curriculum
- The Connection Between Biodiversity and Human Health: Nurses’ Responsibilities
- Nurses’ Advocacy for Clean Water and Air Quality
- Environmental Sustainability in Nursing: Challenges and Opportunities
- Nurses’ Engagement in Community Environmental Health Projects
Opinion Topics On Education
- The Evolution of Nursing Education: Challenges and Innovations
- The Impact of Technology on Nursing Education
- The Role of Simulation in Nursing Education
- The Importance of Interprofessional Education for Nursing Students
- Online Learning in Nursing Education: Pros and Cons
- Addressing Diversity and Inclusion in Nursing Education
- Strategies for Enhancing Clinical Education for Nursing Students
- The Significance of Lifelong Learning for Nursing Professionals
- The Role of Mentorship Programs in Nursing Education
- Integrating Cultural Competence in Nursing Curriculum
- The Impact of Accreditation on Nursing Education Programs
- Nurse Educators as Change Agents in Healthcare Education
- Balancing Theory and Practice in Nursing Education
- Addressing Mental Health Awareness in Nursing Curriculum
- The Influence of Standardized Testing in Nursing Education
Health Opinion Topics
- Universal Healthcare: A Nursing Perspective
- The Impact of Socioeconomic Factors on Health Disparities
- The Role of Nurses in Preventive Healthcare
- Mental Health Stigma: Nurses as Advocates for Change
- Addressing the Opioid Epidemic: Nurses’ Contributions
- Integrating Holistic Approaches in Mental Health Nursing
- The Influence of Culture on Healthcare Beliefs and Practices
- Telehealth and its Impact on Access to Healthcare
- The Importance of Health Literacy in Patient Care
- Nurses’ Involvement in Community Health Promotion
- Palliative Care: A Holistic Approach to End-of-Life Nursing
- The Intersection of Public Health and Nursing Practice
- The Role of Nurses in Health Policy Advocacy
- Emerging Trends in Global Health: Nurses’ Perspectives
- The Challenges of Providing Healthcare in Rural Communities
Psychology Opinion Topics
- The Influence of Psychology in Nursing Practice
- Addressing Mental Health in Critical Care Nursing
- The Impact of Trauma-Informed Care in Nursing
- Psychosocial Factors in Chronic Illness: A Nursing Perspective
- Nurse-Patient Communication: Applying Psychological Principles
- The Role of Nurses in Mental Health Crisis Intervention
- Integrating Positive Psychology in Nursing Care
- Nurses as Advocates for Mental Health Parity
- The Relationship Between Stress and Nursing Burnout
- The Importance of Emotional Intelligence in Nursing Psychology
- Behavioral Interventions in Pediatric Nursing
- Psychiatric Nursing: Destigmatizing Mental Health Disorders
- Coping Strategies for Nurses Dealing with Patient Loss
- The Impact of Psychological Support in Surgical Nursing
- The Connection Between Sleep and Mental Health: Nursing Considerations
Ethics Opinion Topics
- Ethical Dilemmas in End-of-Life Nursing Care
- The Role of Nurses in Patient Autonomy and Informed Consent
- Balancing Truthfulness and Compassion in Nursing Ethics
- Ethical Considerations in Pediatric Nursing
- Nurses’ Responsibilities in Advocating for Patient Rights
- Cultural Competence and Ethical Decision-Making in Nursing
- The Impact of Healthcare Policies on Nursing Ethics
- The Ethical Implications of Nurse-Patient Boundaries
- Addressing Ethical Challenges in Nursing Research
- The Role of Nurses in Organ Allocation and Transplantation
- Ethical Considerations in the Use of Technology in Nursing
- The Influence of Religious Beliefs on Nursing Ethics
- End-of-Life Decision-Making: Navigating Ethical Quandaries
- The Intersection of Social Justice and Nursing Ethics
- The Ethical Responsibilities of Nurses in Public Health Emergencies
Opinion Essay Topics On Culture
- Cultural Competence in Nursing: Bridging Gaps in Patient Care
- The Influence of Cultural Diversity on Nursing Practices
- The Role of Nurses in Promoting Culturally Competent Care
- Addressing Health Disparities Through Cultural Competence
- Cultural Sensitivity in Pediatric Nursing: A Necessity
- Cultural Competence Training for Nursing Students
- The Impact of Language Barriers on Patient-Nurse Communication
- Integrating Traditional Healing Practices in Nursing Care
- Nurses as Advocates for Culturally Tailored Healthcare Policies
- The Influence of Cultural Beliefs on End-of-Life Care Decision-Making
- The Role of Nurses in Respecting and Preserving Cultural Traditions
- Cultural Competence in Mental Health Nursing
- Challenges in Providing Culturally Competent Palliative Care
- Addressing Racism and Discrimination in Nursing Practice
- The Importance of Cultural Competence in Global Nursing
Technology Opinion Essay Ideas
- The Impact of Wearable Technology on Nursing Care
- Electronic Health Records: Streamlining or Complicating Nursing Practice?
- Telemedicine and its Implications for Nursing
- Nurses as Innovators: The Role of Technology in Healthcare
- Cybersecurity Concerns in Nursing Informatics
- The Integration of Artificial Intelligence in Nursing: Opportunities and Challenges
- The Use of Mobile Apps in Patient Education and Engagement
- The Influence of Technology on Patient-Nurse Communication
- The Ethical Considerations of Health Monitoring Devices in Nursing
- The Role of Virtual Reality in Nursing Education and Training
- Addressing the Digital Divide in Healthcare: Nursing Solutions
- Technology’s Impact on Nursing Workflow Efficiency
- The Use of Robotics in Nursing: Enhancing or Replacing Human Care?
- The Importance of Nurses in Healthcare Technology Adoption
- The Role of Social Media in Nursing: Opportunities and Pitfalls
Social Opinion Topics
- The Role of Nurses in Addressing Social Determinants of Health
- Nurses as Advocates for Gender Equality in Healthcare
- LGBTQ+ Inclusivity in Nursing: Promoting Safe Spaces
- The Impact of Social Isolation on Mental Health: Nursing Interventions
- Nurses’ Contributions to Social Justice Movements
- Addressing Discrimination in Nursing: A Call for Cultural Competence
- The Influence of Social Media on Public Perception of Nursing
- The Role of Nurses in Combatting Human Trafficking
- Nurses as Allies in the Fight Against Substance Abuse Stigma
- The Impact of Poverty on Access to Quality Healthcare: Nursing Perspectives
- Promoting Racial Equity in Nursing Education and Practice
- The Role of Nurses in Advocating for Disability Rights in Healthcare
- The Connection Between Social Support and Health Outcomes: A Nursing Perspective
- Nurses as Leaders in Community Health Initiatives
- The Ethical Responsibilities of Nurses in Social Media Engagement
Public Opinion Essay Topics
- “Public Perceptions of the Role of Government in Healthcare: Pros and Cons”
- “The Impact of Social Media on Shaping Public Opinion”
- “Public Attitudes Towards Vaccination: Addressing Misinformation”
- “The Influence of Media Bias on Public Opinion and Trust”
- “Public Opinion on Climate Change Policies: Challenges and Solutions”
- “The Role of Public Opinion in Shaping Education Policies”
- “Public Perspectives on Police Reform and Community Safety”
- “Government Response to Public Health Emergencies: Assessing Public Trust”
- “Public Opinion on Immigration Policies: Balancing Security and Compassion”
- “The Influence of Public Opinion on Criminal Justice Reforms”
- “Public Perceptions of Income Inequality: Addressing Socioeconomic Disparities”
- “The Impact of Public Opinion on Foreign Policy Decision-Making”
- “Public Attitudes Towards Artificial Intelligence and Automation in the Workplace”
- “Public Opinion on Gun Control: Finding Common Ground”
- “The Role of Public Opinion in Shaping Urban Planning and Development”
Nursing Opinion Essay Topics
- The Role of Nurse Practitioners in Primary Care
- Ethical Dilemmas in Nursing Practice
- Impact of Technology on Nursing Care
- Nursing Shortages: Causes and Solutions
- The Importance of Cultural Competence in Nursing
- Mental Health Awareness in Nursing
- Integrating Holistic Care into Nursing Practice
- Challenges Faced by Male Nurses in the Profession
- The Role of Nurses in Disaster Response
- Nursing Education: Bridging the Gap between Theory and Practice
- Addressing Burnout and Compassion Fatigue in Nursing
- Advocating for Patient Rights: Nurses as Patient Advocates
- End-of-Life Care: Ethical Considerations for Nurses
- Innovations in Nursing: Telemedicine and Remote Patient Monitoring
- The Impact of Evidence-Based Practice on Nursing Outcomes
Literature Opinion Essay Topics
- Exploring the Theme of Identity in Modern Literature
- The Representation of Gender Roles in Classic Literature
- The Role of Nature in Romantic Poetry
- Cultural Perspectives in Post-Colonial Literature
- Dystopian Fiction: Reflections on Societal Issues
- Analyzing the Symbolism of Light and Dark in Literature
- Character Development in Bildungsroman Novels
- Satire and Social Critique in Contemporary Literature
- The Influence of Mythology on Modern Storytelling
- Feminist Perspectives in Literature: Empowerment and Critique
- Exploring Magical Realism in Latin American Literature
- The Impact of War on Literature: From World War I to Present Conflicts
- Environmental Themes in Ecocritical Literature
- LGBTQ+ Representation in Literature: Progress and Challenges
- Nostalgia and Memory in Literary Works
Psychology Opinion Essay Topics
- The Nature vs. Nurture Debate: Contemporary Perspectives
- Exploring the Psychology of Addiction and Recovery
- The Influence of Social Media on Mental Health
- Understanding the Psychology of Prejudice and Discrimination
- Cognitive Behavioral Therapy: Effectiveness and Applications
- Psychodynamic Approaches to Understanding Personality
- Mental Health Stigma: Challenges and Strategies for Change
- The Psychology of Resilience: Coping with Adversity
- The Impact of Childhood Trauma on Adult Mental Health
- Exploring the Psychology of Creativity and Innovation
- Attachment Theory: Implications for Relationships and Development
- Cross-Cultural Psychology: Understanding Human Diversity
- The Psychology of Happiness: Myths and Realities
- Neuroplasticity: The Brain’s Ability to Change and Adapt
- Exploring the Psychology of Motivation and Goal Setting
Some Great Examples of Opinion Essay Questions
- “Is the Role of the Nurse Expanding or Narrowing in Modern Healthcare?”
- “Should Nurses Have a More Prominent Role in Health Policy Decision-Making?”
- “How Can Nurses Contribute to the Prevention of Chronic Diseases in Communities?”
- “Do Advances in Technology Enhance or Compromise the Patient-Nurse Relationship?”
- “What Ethical Considerations Arise in Nurse-Patient Relationships and How Should They Be Addressed?”
- “Should Cultural Competence Training be Mandatory for all Nursing Professionals?”
- “In What Ways Can Nursing Education Adapt to the Changing Landscape of Healthcare?”
- “Should Nurses Take a More Active Role in Advocating for Environmental Sustainability in Healthcare?”
- “How Can Nurses Address Mental Health Stigma in the Workplace?”
- “Is Telehealth the Future of Nursing Care, or Does it Pose Risks to Patient Well-being?”
- “Should Nurses Be Involved in End-of-Life Decision-Making, and to What Extent?”
- “What Role Can Nurses Play in Promoting Social Justice and Equity in Healthcare?”
- “How Can Nursing Education Programs Foster Diversity and Inclusion?”
- “Is Gender Equality Achievable in the Nursing Profession, and What Barriers Exist?”
- “What Steps Can Nurses Take to Combat Discrimination and Bias in Healthcare?”
Final Thoughts on Opinion Writing Prompts
Opinion writing prompts are valuable tools that encourage individuals to articulate their thoughts on a diverse array of topics. By engaging with these prompts, whether as students refining their persuasive skills or writers seeking inspiration, individuals contribute to a broader dialogue that shapes understanding on societal, technological, and ethical fronts.
READ MORE >>
Organizational Analysis My Experience Sample PaperThroughout this course, I have ...
Organizational Analysis My Experience Sample Paper
Throughout this course, I have had the opportunity to engage in an in-depth organizational analysis by shadowing a nurse leader in the organization I work and observing her leadership strategies and behaviors. As a result of this experience, I have reflected on my leadership and management styles and skills and gained invaluable insights into the complex roles of nurse leaders in healthcare organizations. I have also understood the critical role that effective leadership and management play in providing high-quality patient care. This paper aims to provide an overview of my experience in this course and highlight my observation, reflection, and professional development.
Observation
I observed a few conflicts during shadowing my nurse leader. One instance involved a disagreement between two of the nurses on the team about the best approach to a care plan for a patient. My nurse leader was effective in handling the conflict by facilitating a collaborative method of conflict resolution between the two nurses, allowing each nurse to explain the reasoning behind their approach and encouraging them to come to a consensus (Moeta & du Rand, 2019). She also encouraged mutual respect between the two nurses, allowing them to resolve the issue. Her transformational leadership style was evident in her ability to motivate the two nurses to work together to resolve.
Another conflict I observed was a disagreement between a nurse and a physician on the best course of treatment for a patient. My nurse leader was able to effectively handle this conflict by utilizing her communication skills to ensure that both parties were heard and that each understood the other’s perspective (Gossman et al., 2019). She was also able to provide evidence-based research to support the patient’s care plan and explain why it was the best option for the patient. Her transformational leadership style enabled her to foster an environment of trust and mutual respect between the two parties, enabling them to reach a resolution that was in the patient’s best interest.
Patients sometimes refuse to follow their prescribed care plan leading to conflicts between the patient and the care provider. My nurse leader would typically handle this conflict by first understanding the patient’s reason for refusal and then educating the patient on the importance of the care plan and the care provider on the importance of collaborative care planning (Kwame & Petrucka, 2021). She would also utilize her evidence-based research to support her explanations and encourage open dialogue between the patient and healthcare professionals. Her transformational leadership style would be evident in her ability to motivate the patient to understand the importance of the care plan and follow it to achieve the best outcomes.
Reflections
My initial impression of the Nurse Manager was that she was well-equipped and knowledgeable to lead the nursing staff in providing high-quality patient care. Through this shadowing experience, I have come to understand the importance of the nurse manager’s role in an organization and the unique skills and abilities required to excel in this role through her continuous professional development. I have also gained a greater appreciation for the Nurse Manager’s commitment to providing quality patient care and staying up-to-date with the latest developments in the nursing field.
My leadership style is collaborative, as I prefer to take a more personal approach to address each patient’s individual needs. According to Ang’ana and Kilika (2022), leaders employing a collaborative leadership style work closely with their team members to achieve shared organizational goals. The leader encourages open communication and actively seeks input and feedback from team members. This style emphasizes teamwork and collaboration, as opposed to a top-down approach where the leader makes decisions independently (Ang’ana & Kilika, 2022).
I believe that this leadership style would complement the organization as it allows for a more personalized approach to patient care. I also believe that my leadership style would work in tandem with my nurse manager’s leadership skills and style, as they both focus on providing quality patient care and staying up-to-date on the latest advancements in the field.
My nurse manager’s leadership skills and style effectively complement the effectiveness of the organization. According to Mlambo et al. (2021), ongoing professional development is essential to nurses’ lifelong learning and is an important aspect of keeping their knowledge and skill up-to-date. Her commitment to ongoing professional development and effective communication skills ensure that the nursing staff is informed of changes and updates to policies and procedures. Additionally, her transformational leadership style fosters trust, mutual respect, and improved patient outcomes.
Professional Development
Given the opportunity, I would like to have this position as a Nurse Manager. I believe that my experience in nursing, combined with my dedication to providing quality patient care and staying up-to-date with the latest developments in the field, would enable me to excel in this role. I also believe that I possess the necessary skills for success, such as financial management, negotiation, recruitment and development of staff, conflict resolution, staying updated on technological advancements, and effective leadership.
I believe that advancing my studies by pursuing a Master of Science in Nursing (MSN) degree and certification as a Nurse Leader (CNL) would be beneficial to develop my skills further and acquire new ones. According to Bender et al. (2019), advancement in the educational level of a clinical nurse leader is essential in identifying and evaluating suitable models of care delivery, thereby enhancing the safety and quality of patient care.
Additionally, attending conferences, workshops, and seminars and reading professional journals would help me stay informed on best practices in nursing leadership and management (Price & Reichert, 2019). I would also take advantage of online courses and webinars to expand my knowledge and skills in the field.
Conclusion
Through my experience in this course, I have gained a greater understanding of the importance of effective leadership and management in providing high-quality patient care. I have also come to understand the unique roles and skills required to excel in the role of a Nurse Manager. I believe that my experience in nursing, combined with my dedication to providing quality patient care and staying up-to-date with the latest developments in the field, would enable me to be successful in this role.
I plan to pursue a Master of Science in Nursing (MSN) degree and certification as a Nurse Leader (CNL) to further my education and knowledge in the field. I also plan to take advantage of online courses and webinars, conferences, workshops, and seminars to stay informed on best practices in nursing leadership and management.
References
- Ang’ana, G. A., & Kilika, J. M. (2022). Collaborative leadership in an organizational context: A research agenda. Journal of Human Resource &Leadership, 6(1), 48–71. https://doi.org/10.53819/81018102t2050
- Bender, M., Baker, P., Harris, J. L., Hites, L., LaPointe, R. J., Murphy, E. A., Roussel, L., Spiva, L., Stanley, J. M., Thomas, P. L., & Williams, M. (2019). Advancing the clinical nurse leader model through academic-practice-policy partnership. Nursing Outlook, 67(4), 345–353. https://doi.org/10.1016/j.outlook.2019.02.007
- Kwame, A., & Petrucka, P. M. (2021). A literature-based study of patient-centered care and communication in nurse-patient interactions: Barriers, facilitators, and the way forward. BMC Nursing, 20(1). https://doi.org/10.1186/s12912-021-00684-2
- Mlambo, M., Silén, C., & McGrath, C. (2021). Lifelong learning and nurses’ continuing professional development, a meta-synthesis of the literature. BMC Nursing, 20(62), 1–13. https://doi.org/10.1186/s12912-021-00579-2
- Moeta, M. E., & du Rand, S. M. (2019). Use of scenarios to explore conflict management practices of nurse unit managers in public hospitals. Curationis, 42(1). https://doi.org/10.4102/curationis.v42i1.1943
- Price, S., & Reichert, C. (2019). The importance of continuing professional development to career satisfaction and patient care: Meeting the needs of novice to mid- to late-career nurses throughout their career span. Administrative Sciences, 7(2), 1–13. https://doi.org/10.3390/admsci7020017
READ MORE >>
Organizational Analysis The Nurse Leader Sample PaperHealthcare organizational a ...
Organizational Analysis The Nurse Leader Sample Paper
Healthcare organizational analysis is crucial in ensuring that healthcare facilities run effectively and efficiently. The analysis helps to identify areas that require improvement and strategies that can be implemented to enhance the quality of patient care. Effective leadership and management are integral to contemporary healthcare and essential for any organization’s success. Nurse leaders, in particular, are vital in delivering high-quality patient care and promoting positive outcomes for patients and staff.
This paper examines the key characteristics that differentiate leadership and management, comparing and contrasting their respective roles and functions. The paper also aims to explore how trends, issues, theories, and evidence can be utilized as guidelines for making effective management decisions and evaluate the effectiveness of communication patterns in successful leadership and management.
Nurse Manager
The provision of healthcare relies on the role of a nurse manager in ensuring the efficient functioning of healthcare organizations. As the demand for nursing services continues to grow with an estimated projection of 15% by 2026 due to an aging population, an increase in the number of people with chronic conditions, and the emphasis on preventive care, nurse managers play an essential role in managing resources effectively to ensure optimal patient care (Cox, 2019). Their responsibilities include overseeing finances, staff, materials, and time.
Therefore, nurse managers must possess unique skills such as financial management, negotiation, recruitment and development of staff, conflict resolution, staying updated on technological advancements, and effective leadership to succeed in their roles.
I have the privilege of working under the leadership of a highly qualified and experienced Nurse Manager in my practice as a nurse in a busy health organization. She has a Bachelor of science in nursing (BSN) degree and a Master of science in nursing (MSN) degree from accredited universities, as well as certification as a nurse leader (CNL) and in basic life support (BLS) and advanced cardiovascular life support (ACLS) making her well-equipped to manage the daily operations of the nursing staff and ensuring quality patient care.
She has consistently demonstrated exemplary leadership skills and a commitment to providing the highest level of patient care in her five years as a nurse manager. She is dedicated to staying up-to-date with the latest developments in the nursing field. As an active member of several professional organizations, she regularly attends conferences, workshops, and seminars. She also subscribes to and reads professional journals to stay informed on best practices in nursing leadership and management.
One of my Nurse Manager’s most effective traits is her commitment to providing quality patient care. She sets a high standard for her staff to follow and consistently exceeds expectations as a leader. Additionally, her dedication to ongoing professional development ensures that she stays current with the latest nursing developments.
While I share my Nurse Manager’s commitment to providing quality patient care and regularly read professional journals to stay informed, I have a different perspective on developing policies and procedures. While my supervisor collaborates with other healthcare professionals to develop policies and procedures that align with the hospital’s mission and goals, I prefer a more flexible approach to accommodate each patient’s needs.
Nurse Leader
The nurse manager employs a transformational leadership style in carrying out organizational duties. As a transformational leader, she inspires her staff to exceed their expectations and achieve greater patient outcomes while fostering trust and mutual respect between the leaders and the team. Transformational leadership is an effective leadership style in nursing that can lead to improved patient outcomes, increased job satisfaction, better communication, higher levels of engagement, improved patient safety, and reduced nurse burnout (Asif et al., 2019). This leadership style has enabled her to lead her staff in providing high-quality patient care.
One effective way the nurse manager handles her responsibilities effectively is her commitment to ongoing professional development. She attends conferences, workshops, and seminars and reads professional journals, enabling her to stay up-to-date with the latest developments in nursing. This enhances her knowledge and skills and enables her to share this knowledge with her team and implement best practices in patient care (Mlambo et al., 2021).
The second effective method she uses to handle her responsibilities is her ability in managing resources effectively. This includes overseeing finances, staff, materials, and time. She must make strategic decisions about resource allocation to ensure optimal patient care. Her financial management, negotiation, and staff development skills have enabled her to succeed in this regard.
Thirdly, she is committed to providing quality patient care. She sets a high standard for her staff to follow and consistently exceeds expectations as a leader. This commitment to quality patient care fosters a sense of pride and purpose among her team members, who are motivated to provide the best possible outcomes for their patients. Finally, her effective communication skills are another example of her leadership effectiveness.
Communication is a vital component of successful leadership and management in healthcare settings, and the nurse manager ensures that her team is kept informed of changes and updates to policies and procedures (Brown, 2020). She also encourages open and honest communication among team members, which fosters a sense of trust and respect within the team and ultimately leads to better patient outcomes.
The nurse manager also demonstrates effective leadership skills in decision-making, strategic planning, and problem-solving. These skills enable her to make informed decisions and act to address challenges as they arise (Cakir & Adiguzel, 2020). However, one area where she could improve is in delegating tasks to team members. While delegation is an important leadership skill, the nurse manager tends to take on many tasks herself rather than delegating them to others, which can lead to burnout and reduced efficiency.
Communication
Effective communication is essential to successful leadership and management in healthcare organizations. One of the effective types of communication employed by the nurse manager is verbal communication. She communicates regularly with her team members to ensure they are aware of updates and changes to policies and procedures. She also encourages open and honest communication among team members, which fosters a sense of trust and respect within the team (Brown, 2020). The nurse manager, however, should utilize digital tools such as video conferencing to enhance the effectiveness of verbal communication further to reach a wider audience.
The nurse manager also uses written communication to inform her team members of changes to policies and procedures. She writes memos and emails to share important information with her team. The nurse manager should consider utilizing online platforms such as Google Docs or Slack, making it easier for her to communicate with her team members and ensure that her team can access the most up-to-date information.
The nurse manager also uses non-verbal communication as another type of communication. She often uses non-verbal cues such as body language, facial expressions, and eye contact to convey her message. This is particularly important when communicating with patients, as it can help to create a sense of trust and mutual respect (Ali, 2019). To further improve the effectiveness of non-verbal communication, the nurse manager should consider utilizing visual aids such as charts and diagrams to help her team better understand her message.
Conclusion
The nurse manager plays a vital role in healthcare provision and oversees finances, staff, materials, and time. She must possess a unique set of skills such as financial management, negotiation, recruitment and development of staff, conflict resolution, staying updated on technological advancements, and effective leadership to succeed in her role.
She exemplifies leadership in her commitment to providing quality patient care and staying up-to-date with the latest developments in the nursing field. The nurse manager’s commitment to ongoing professional development, resource management, effective communication, and effective decision-making are all critical components of successful leadership and management in healthcare organizations.
References
- Ali, M. (2019, January 15). Communication skills 3: Non-verbal communication. Nursing Times. https://www.nursingtimes.net/clinical-archive/assessment-skills/communication-skills-3-non-verbal-communication-15-01-2018/
- Asif, M., Jameel, A., Hussain, A., Hwang, J., & Sahito, N. (2019). Linking transformational leadership with nurse-assessed adverse patient outcomes and the quality of care: Assessing the role of job satisfaction and structural empowerment. International Journal of Environmental Research and Public Health, 16(13), 2381. https://doi.org/10.3390/ijerph16132381
- Brown, A. (2020). Communication and leadership in healthcare quality governance. Journal of Health Organization and Management, 34(2), 144–161. https://doi.org/10.1108/jhom-07-2019-0194
- Cakir, F. S., & Adiguzel, Z. (2020). Analysis of leader effectiveness in organization and knowledge sharing behavior on employees and organization. SAGE Open, 10(1), 1–14. Sagepub. https://doi.org/10.1177/2158244020914634
- Cox C. A. (2019). Nurse manager job satisfaction and retention: A home healthcare perspective. Nursing Management, 50(7), 16–23. https://doi.org/10.1097/01.NUMA.0000558512.58455.68
- Mlambo, M., Silén, C., & McGrath, C. (2021). Lifelong learning and nurses’ continuing professional development, a meta-synthesis of the literature. BMC Nursing, 20(62), 1–13. https://doi.org/10.1186/s12912-021-00579-2
READ MORE >>
Organizational Change and Decision-making Sample PaperChange decision-making is ...
Organizational Change and Decision-making Sample Paper
Change decision-making is an integral part of a manager’s daily activities. whether reshuffling the department employees or delegating tasks, the daily decisions managers make have a significant impact on the organization. However, according to McConnell (2018), it is always good practice to involve the team in the process because bringing people into the conversation about any apparent change would make them ‘own’ the process. In this case, though, the administrator did not involve the working supervisors when making the decision to fire the office manager. This was wrong because the supervisors would feel ignored, a phenomenon that would breed conflict, distrust and disharmony (Sharma et al, 2018).
The business office staff would then develop an overriding negative attitude towards the effected change because they were not involved or consulted in the decision to replace the office manager. This can derail the supervisors’ engagement, productivity and performance; ultimately having a negative impact on their productivity (Tappen et al, 2017). Furthermore, deciding to replace the office manager with an outsider create a sense of insecurity among the supervisors, dwelling with them through that they could lose their jobs to outsiders at any time.
This attitude might have a direct impact on the supervisor’s behaviour towards the new office manager, which could possibly affect the new office manager’s performance (Zhao et al, 2021). They might fail to effectively interact and integrate him into the organization, especially with the view that he or she is an outsider. Consequently, the productivity of the supervisors, as well as that of the new office manager, may quickly decrease, affecting the organization’s ability to achieve its objectives.
Every change to the familiar can cause frustration, resistance and friction, and that is why there needs to be employee involvement in every change process. Replacing the office manager is a significant change of team structure that may be accompanied by a change in new expectations, new workflows and new behavior. These apparent changes may be jarring to the supervisors and cause undesirable attitudes in them.
References
- McConnell, C. R. (2018). The effective health care supervisor. Jones & Bartlett Learning.
- Sharma, N., Herrnschmidt, J., Claes, V., Bachnick, S., De Geest, S., Simon, M., & MatchRN?
- Study Group. (2018). Organizational readiness for implementing change in acute care hospitals: an analysis of a cross?sectional, multicentre study. Journal of advanced nursing, 74(12), 2798-2808. https://doi.org/10.1111/jan.13801
- Tappen, R. M., Wolf, D. G., Rahemi, Z., Engstrom, G., Rojido, C., Shutes, J. M., & Ouslander, J. (2017). Barriers and facilitators to implementing a change initiative in long-term care utilizing the INTERACT™ quality improvement program. The health care manager, 36(3), 219. doi: 10.1097/HCM.0000000000000168
- Zhao, Y., Liao, L., Feng, H., Chen, H., & Ning, H. (2021). Enablers and barriers to implementing care quality improvement program in nursing homes in China. BMC geriatrics, 21(1), 1-10. https://link.springer.com/article/10.1186/s12877-021-02488-0
READ MORE >>
Organizational Needs Assessment NR703Organizational Needs Assessment NR703NR703 ...
Organizational Needs Assessment NR703
Organizational Needs Assessment NR703
NR703 Week 2 Organizational Needs Assessment
Assignment
Purpose
The purpose of this assignment is to identify a practice problem based on an organizational needs assessment, including the identification of the practice gap and formulation of the practice question. This assignment will allow for the assimilation of professional leadership competencies in project management as a DNP-prepared nurse. Assignment content supports professional formation, communication, and dissemination skills relevant to the DNP-prepared nurse.
Please note that this is the first part of a 3-part assignment submitted in Weeks 2, 5, and 7. You will receive corrective feedback from your course faculty on the Week 2 and Week 5 assignments that you will use to prepare the Week 7 assignment.
Also Read:
NR703 Week 3 Leading Interprofessional Teams Discussion
NOTE: All NR703 assignments and their requirements should be discussed in relation to your proposed or hypothetical DNP practicum project. **No DNP practicum project will be approved for implementation until the second practicum course, NR-705 Project & Practicum II
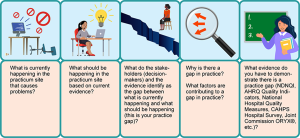
Instructions
Complete the Organizational Needs Assessment: Practice Gap Identification Table on a healthcare organization of your choice. This will be submitted as Table 1.
- Link (Word doc): Organizational Needs Assessment: Practice Gap Identification TemplateLinks to an external site.
Include the following in your paper:
- Introduction
- Introduce the topic and establish the importance of an organizational needs assessment.
- Present a clear purpose statement.
- Create an organizing (outline) statement for the paper that matches the required level 1 headings (except for listing the conclusion).
- Problem: Using the information that you gathered on the Organizational Needs Assessment: Practice Gap Identification (Table 1), describe the practice problem by explaining these elements:
- Describe a specific location (hospital unit, community health clinic, surgical suite, primary care practice).
- Identify the key stakeholders (decision-makers).
- Explain the practice problem as would be identified by the stakeholders.
- Practice Gap
- In 1-2 organized paragraphs, summarize your findings in table 1, the Organizational Needs Assessment: Practice Gap Identification. Ensure the table is placed after the reference list starting on its own page with the heading Table 1.
- Practice Question: Define and briefly explain the project’s intended population, evidence-based intervention, and measurable outcomes (PICOT):
- Population: Describe the specific characteristics of the population that is the focus of the intervention.
- Intervention: Citing evidence listed in the Johns Hopkins Individual Evidence Summary Tool (Table 2) which was initiated in NR-716, describe the evidence-based intervention. There should be a total of three (3) references listed in Table 2 for this assignment. If necessary, add one research study or systematic review to support your intervention unless one already exists on the table from your previous courses.
- Comparison: State “compared to current practice” for the purposes of this assignment.
- Create and explain specific outcome measurements based on the current evidence you have collected in the Johns Hopkins Individual Evidence Summary Tool (attached as Table 2). If needed, add one research study or systematic review that supports your proposed outcome measurements.
- The source can be the same one that was used to support the intervention as long as it speaks to measurable outcomes. There should be a total of three (3) references listed in Table 2 for this assignment.
- Time: Time frame for the project implementation. (Practicum projects are typically 8 – 10 weeks long).
- State the Practice Question. Example: (P) For the critical care team in X hospital’s ICU, (I) does the implementation of the medical sepsis protocol (C) compared to the current practice (O) reduce the incidence of medical sepsis diagnoses in ICU patients as measured before and after the intervention (T) over a 10-week period?
- Conclusion
- Recap the paper’s purpose statement and organizing (outlining) statement of the three level 1 headings (not including the conclusion).
- Draw major conclusions from the body of your paper.
- Summarize the importance of effective communication for the DNP-prepared nurse in performing the practice gap and problem identification.
- References
- Create the reference page.
- Ensure each reference has a matching citation.
- Include a minimum of three (3) scholarly references (all three references on the Johns Hopkins Table should be included).
- Tables
- Add the completed Table 1 & Table 2 after the reference list. For directions on how to copy a table in Microsoft Word go to the following link:
- Link (webpage): Move or Copy a TableLinks to an external site.
- Table 2, the Johns Hopkins Individual Evidence Summary Tool, is attached (after Table 1) & completely filled out with at least three (3) quantitative research studies at a minimum. (NOTE: a minimum of three [3] references should be included on the reference list, including those in Table 2).
- Add the completed Table 1 & Table 2 after the reference list. For directions on how to copy a table in Microsoft Word go to the following link:
Table 1: Organizational Needs Assessment: Practice Gap Identification
What is currently happening in the practicum site that causes the problem?What should be happening in the practicum site based on current evidence*?What do the stakeholders (decision-makers) identify as the gap between what is currently happening and what should be happening (this is your practice gap)?Why is there a gap in practice?What factors are contributing to the gap in practice?
What evidence* do you have to demonstrate there is a practice gap (e.g., NDNQI, AHRQ Quality Indicators, National Hospital Quality Measures, HCAHPS, Joint Commission ORYX®, etc.)?*Reference & citation required.[Add text][Add text][Add text][Add text][Add text][Add text][Add text][Add text][Add text][Add text]
PICOT Problem Statement:
P (Population – example: For critical care team in X hospital ICU…)
I (Intervention – example: Does the implementation of the medical sepsis protocol…)
C (Comparison – example: Compared to current practice). NOTE: “C” is most commonly used for research projects, not DNP translation science projects. “C,” or Comparison intervention, is implied for DNP projects, although you will see instances where the C does not apply.
O (Outcome, measurable – example: Reduce the incidence of medical sepsis in patients as measured before and after…)
T (Time – Usually 8-10 weeks for a DNP practicum project)
Review the rubric below for the grading criteria.
APA Guidelines
Use the current Publication Manual of the American Psychological Association (APA Manual) and the Chamberlain Guidelines for Writing Professional Papers: Graduate Programs (located in the Canvas Resources menu under the Writing Center) to complete this assignment. Follow these guidelines when completing each component. Contact your course faculty if you have questions.
- Use the standard APA Paper Template (located in the Canvas Resources: Writing Center) to format this assignment.
- Turn on Grammarly to check the correctness of the grammar and punctuation as you write. (Note: if you have not already done so, please download the free version at Grammarly.com before constructing the assignment.)
- Use the title, “Organizational Needs Assessment,” for your project and construct a title page using the APA paper template.
- Use the following prescribed Level 1 headings for this paper (do not include the outline letters):
- Problem
- Practice Gap
- Practice Question
- Conclusion
Writing Requirements (APA format)
- Length: 3-4 pages (not including title page, references page, or attachments)
- 1-inch margins
- Double-spaced pages
- 12-point Times New Roman
- Headings & subheadings
- In-text citations
- Title page
- Reference page
- Standard English usage and mechanics
- CARE Plan paragraph development structure
Program Competencies
This assignment enables the student to meet the following program competences:
- Applies organizational and system leadership skills to affect systemic changes in corporate culture and to promote continuous improvement in clinical outcomes. (PO 6)
- Appraises current information systems and technologies to improve health care. (POs 6, 7)
- Creates a supportive organizational culture for flourishing collaborative teams to facilitate clinical disease prevention and promote population health at all system levels. (PO 8)
Course Outcomes
This assignment enables the student to meet the following course outcomes:
- Compare and contrast theories of organizational behavior and leadership. (PCs 2, 4; PO6)
- Investigate the role of advanced nursing practice in innovation and transformation to propose solutions impacting healthcare systems. (PCs 2, 4; PO 6)
- Differentiate attributes of effective leaders and followers in influencing healthcare. (PCs 2, 4; PO 6)
- Formulate selected strategies for leadership and influence across healthcare systems. (PC 6; PO 8)
Due Date
- By 11:59 p.m. MT on Sunday
- Late Assignment Policy applies
Rubric
Organizational Needs Assessment NR703 Week 2 Assignment Grading Rubric
W2 Assignment Grading RubricCriteriaRatingsPtsThis criterion is linked to a Learning Outcome IntroductionRequirements:
1. Introduce the topic and establish the importance of an organizational needs assessment.
2. Present a clear purpose statement.
3. Create an organizing statement for the paper that matches the level 1 headings (except for listing the conclusion).
Includes all requirements and provides an in-depth introduction.
9 ptsIncludes 2 requirements and/or provides a sufficient introduction.
8 ptsIncludes 1 requirement and/or provides a partial introduction.
0 ptsProvides an undeveloped introduction.
10 ptsThis criterion is linked to a Learning Outcome Problem: Using the information that you gathered on the Organizational Needs Assessment: Practice Gap Identification (Table 1), describe the practice problem.Requirements:
1. Describe a specific location (hospital unit, community health clinic, surgical suite, primary care practice).
2. Identify the key stakeholders (decision makers).
3. Relate the practice problem identified by the stakeholders.
Includes all requirements and provides an in-depth description of the problem.
27 ptsIncludes at least 2 requirements and/or provides a sufficient description of the problem.
24 ptsIncludes at least 1 requirement and/or provides a partial description of the problem.
0 ptsProvides an undeveloped description of the problem.
30 ptsThis criterion is linked to a Learning Outcome Practice GapRequirements:
1. In 1-2 organized paragraphs, summarize your findings in Table 1, the Organizational Needs Assessment: Practice Gap Identification
2. Include a thoroughly completed Organizational Needs Assessment: Practice Gap Identification Table as Table 1, placed after the reference list.
30 ptsIncludes Table 1 and provides an in-depth summary of the Organizational Needs Assessment: Practice Gap Identification (Table 1).
27 ptsIncludes Table 1 and provides a sufficient summary of the Organizational Needs Assessment: Practice Gap Identification (Table 1).
24 ptsIncludes no Table 1 and/or provides a partial summary of the Organizational Needs Assessment: Practice Gap Identification (Table 1).
0 ptsProvides no Table 1 and/or an undeveloped summary of the Organizational Needs Assessment: Practice Gap Identification (Table 1).
30 ptsThis criterion is linked to a Learning Outcome Practice Question: Define and briefly explain the project’s intended population, evidence-based intervention, and measurable outcomes (PICO).Requirements:
1. Population. Describe the specific characteristics of the population that is the focus of the intervention.
2. Intervention. Citing evidence listed in the Johns Hopkins Individual Evidence Summary Tool (Table 2), which was initiated in NR-716, describe the evidence-based intervention.
3. Comparison: State “compared to current practice” for the purposes of this assignment.
4. Outcome. Create and explain specific outcome measurements based on the current evidence collected in the Johns Hopkins Individual Evidence Summary Tool (attached as Table 2, placed after Table 1).
5. Time. State the time length for the project (i.e., 8-10 weeks).
6. State the Practice Question.
7. Table 2, the Johns Hopkins Individual Evidence Summary Tool, is attached & completely filled out with at least three (3) quantitative research studies at a minimum. (NOTE: all three [3] references should be included on the reference list).
Includes Table 2 and all data requirements and provides an in-depth summary of the practice question.
36 ptsIncludes Table 2, no fewer than 5 of the requirements, and provides a sufficient summary of the practice question.
32 ptsIncludes Table 2, no fewer than 4 of the requirements, and provides a partial summary of the practice question.
0 ptsIncludes no attached Table 2, fewer than 4 of the requirements, and/or provides an undeveloped summary of the practice question.
40 ptsThis criterion is linked to a Learning Outcome ConclusionRequirements:
1. Recap the paper’s purpose and organizing (outline) criteria that revisit the three level 1 headings (not including the conclusion).
2. Draw major conclusions from the body of your paper.
3. Summarize the importance of effective communication competencies for the DNP-prepared nurse in performing the practice gap and problem identification.
Includes all requirements and provides an in-depth summary in the conclusion.
9 ptsIncludes at least 2 requirements and/or provides a sufficient summary in the conclusion.
8 ptsIncludes at least 1 requirement and/or provides a partial summary in the conclusion.
0 ptsProvides an undeveloped summary in the conclusion.
10 ptsThis criterion is linked to a Learning Outcome ReferencesRequirements:
1. Create the reference page using the APA template and the Chamberlain Guidelines for Writing Professional Papers.
2. Ensure each reference has a matching citation that follows the formatting guidelines in the APA manual/ Chamberlain Guidelines for Writing Professional Papers.
3. Include at least three (3) scholarly references at a minimum (including those from the Johns Hopkins Table)
Includes all requirements of the reference section, at least three scholarly references with matching citations, and the reference page is formatted without errors.
9 ptsIncludes at least 2 requirements for the reference section, and/or the reference page is formatted with 1-2 errors.
8 ptsIncludes 2 requirements for the references, and/or the reference page is formatted with several errors.
0 ptsIncludes fewer than 1 requirement for the reference section, and/or the reference page is formatted with multiple errors.
10 ptsThis criterion is linked to a Learning Outcome APA Style and Organization for Scholarly PapersRequirements:
1. Use prescribed level I headings for section organization.
2. Format the paper using APA formatting conventions.
3. Length of APA formatted paper is 3-4 pages (excluding title page, reference page, and tables).
Includes all requirements of APA style and standards.
9 ptsIncludes 2 requirements of APA style and standards.
8 ptsIncludes 1 requirement of APA style and standards
0 ptsIncludes no requirement of APA style and standards that conforms to APA style.
10 ptsThis criterion is linked to a Learning Outcome Clarity of WritingRequirements:
1. Use of standard English grammar and sentence structure.
2. No spelling errors or typographical errors.
3. Organized and logical presentation of ideas in paragraphs (CARE Plan), sentences, and phrases
Includes all requirements of clarity of writing.
9 ptsIncludes 2 requirements of clarity of writing.
8 ptsIncludes 1 requirement of clarity of writing.
0 ptsIncludes no clarity of writing requirements that conform to standard English (APA) style.
10 ptsTotal Points: 150PreviousNext
NR703 Week 2 Lesson 2 Leading through Translational Science Change Frameworks
Organizational Needs Assessment
A primary role of DNP-prepared nurses is translating evidence into practice. You have already been conceptualizing the topic areas you are interested in developing for your DNP practice change project and have begun collecting evidence for them in a Johns Hopkins Individual Evidence Summary Tool (Dang & Dearholt, 2018).
However, you may not have considered what your practicum site needs, which may not be what you have envisioned. That raises several questions.
- What do the stakeholders or practicum site decision-makers want you to do?
- What answers to practice gaps do stakeholders invested in your project need answered?
- Is the idea you have practical for the practicum site?
- Does the organization have a larger project or agenda that a DNP project might serve?
So, the first thing a DNP-prepared nurse must do to implement a practice change project is to understand what needs to be done and why. An organizational needs assessment is the foundational planning step that you must take for your DNP practice change project. Benjamin Franklin once said, “By failing to prepare, you are preparing to fail.” You cannot prepare unless you know what needs to be done, and that may not necessarily be what you have in mind.
As Yogi Berra once quipped, “If you don’t know where you’re going, you’ll end up someplace else.”
Many nurses conceptualize an organizational needs assessment by using the familiar nursing process format (ADPIE).
ADPIE Image Description
The needs assessment also drives the three primary conceptual project areas shown here in this Conceptual Project Portrait.
Conceptual Project Portrait Image Description
Practice Gap Identification
In this week’s assignment, you will construct an organizational needs assessment at a hypothetical practicum site. This will give you practice in performing the task and reinforce that a needs assessment to identify the practice gap is the foundational starting point for your practice change project. (Typical practicum sites include advanced practice setting, acute hospital care, LTC, community setting [church], health department, and home care.)
To perform a needs assessment with the practicum site stakeholders, use the following guide to help you understand what gaps are occurring between current practice and evidence-based practice.
Practice Gap Identification Image Description
Review the following examples:
Practice ProblemWhat is currently happening in the practicum site that causes problems?What should be happening in the practicum site based on current evidence?What do the stakeholders (decision-makers) and the evidence identify as the gap between what is currently happening and what should be happening (this is your practice gap)?Why is there a gap in practice? What factors are contributing to a gap in practice?What evidence do you have to demonstrate there is a practice gap (NDNQI, AHRQ Quality Indicators, National Hospital Quality Measures, CAHPS Hospital Survey, Joint Commission ORYX®, etc.)?Pediatric PracticeThere are no clinical practice guidelines being used for the management of obese patients in a pediatric setting.Nurse Practitioners (NPs) should be using evidence-based clinical practice guidelines to better manage children who are obese.Approximately 40% of the patient population have been identified as being obese; however, there are no clear guidelines in place for the NPs to use/follow when planning patient care.Potential issue with lack of knowledge associated with updated guidelines for pediatric obesity.Physician-owned facility; potential lack of NP autonomy regarding practice.
Comments provided by the NPs.NPs report they want to be able to better manage and plan care for pediatric patients who are obese.
National best-practice identifies that clinical practice guidelines should be used.
Diagnostic indicators by incidence demonstrate an increase in obesity at this practice.
Long-Term Care FacilityThe current practice for the prevention of unassisted falls is ineffective.Unassisted falls, including falls with injuries, should not occur in the facility.Stakeholders (particularly administrator, DON, & corporate governance) and ACHA survey results have established that there is an unacceptable rate of unassisted falls in the facility that is not being adequately addressed.The current falls prevention process is not being followed.Specifically, the gap in practice revealed
· The initial fall risk factor assessment was not completed consistently.
· Patients’ medications were not always reviewed for fall risk.
· Patients with frequent toileting needs are not always assisted in a timely manner.
MDS assessment data for fallsNursing Home Compare (NHC) measures
Internal QI data reports per unit
Internal Falls Prevention Audit
Risk Management data & litigation results
NR703 Week 2 References
Bunting, M. (2016). The mindful leader: 7 practices for transforming your leadership, our organization and your life. John Wiley & Sons Australia, Ltd.
Dang, D., & Dearholt, S. (2018). Johns Hopkins nursing evidence-based practice: Model and guidelines. Sigma Theta Tau International.
Nadler, R., Carswell, J. J., & Minda, J. P. (2020). Online mindfulness training increases well-being, trait emotional intelligence, and workplace competency ratings: A randomized waitlist-controlled trial. Frontiers in Psychology, 11, 1-19. https://doi.org/10.3389/fpsyg.2020.00255
READ MORE >>
Organizational Risk Management Interview HLT 308Organizational Risk Management I ...
Organizational Risk Management Interview HLT 308
Organizational Risk Management Interview HLT 308
WEEK 4 HLT 308 Organizational Risk Management Interview
Requires Lopeswrite
Assessment Description
The purpose of this assignment is to gain real-world insight into how risk management programs operate within health care organizations.
Select a local health care organization where you can conduct an interview with an employee who is involved in risk management processes. This organization can be your current employer or a different health care facility in your community. Acute care, urgent care, large multi?provider private medical clinics, assisted living facilities, and community/public health clinical facilities are all ideal options to complete the requirements of this assignment. Select an individual who can provide sufficient information regarding how their organization manages risk within its facility to answer the questions below.
In your interview, address the following:
- Risk management strategies used in the organization’s risk control program, along with specific examples.
- How the facility’s educational risk management program addresses key professional, legal, and ethical issues, such as prevention of negligence, malpractice litigation, and vicarious liability.
- Policies the facility has implemented that address how to manage emergency triage in high?risk areas of health care service delivery (e.g., narcotics inventories, declared pregnancy policies, blood-borne disease sector, etc.).
- Challenges the organization faces in managing and controlling high-risk health care (e.g., infectious diseases, nuclear medicine, abortion, class 4 narcotics/opioids, etc.).
- Strategies the facility utilizes to monitor, evaluate, and maintain compliance within its risk management program.
After conducting the interview, compose a 750?1,000 word summary analysis of the interview that includes the questions above, in conjunction with the interviewee’s responses. In addition, include the following elements in your response:
- An assessment of the organization’s risk management program, including how it attends to high-risk health care and legal concerns.
- Action steps you would take to improve one area of the organization’s risk management program, along with your rationale for doing so.
Cite appropriate references as needed to support your statements and rationale.
Prepare this assignment according to the guidelines found in the APA Style Guide, located in the Student Success Center. An abstract is not required.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
REFERENCES MUST BE BETWEEN 2019-2023
Organizational Risk Management Interview – Rubric
Rubric Criteria
Risk Management Strategies Used in the Risk Control Program
Criteria Description
Risk Management Strategies Used in the Risk Control Program
Risk management strategies used in the risk control program are comprehensive. The submission incorporates analysis of supporting evidence insightfully and provides specific examples with relevance. Level of detail is appropriate.
How the Risk Management Program Addresses Key Professional, Legal, and Ethical Issues
Criteria Description
How the Risk Management Program Addresses Key Professional, Legal, and Ethical Issues
A description of how the risk management program addresses key professional, legal, and ethical issues is comprehensive, supported by detailed, relevant examples. Level of detail is appropriate.
4: Facility Policies for Managing Emergency Triage in High-Risk Areas of Health Care Service Delivery
Criteria Description
Facility Policies for Managing Emergency Triage in High-Risk Areas of Health Care Service Delivery
An explanation of the facility policies for managing emergency triage in high-risk areas of health care service delivery is present and comprehensive. The submission incorporates analysis of supporting evidence insightfully and provides specific examples with relevance. Level of detail is appropriate.
Challenges the Organization Faces in Managing and Controlling High-Risk Health Care
Criteria Description
Challenges the Organization Faces in Managing and Controlling High-Risk Health Care
A comprehensive description of the challenges the organization faces in managing and controlling high-risk health care is provided. The submission incorporates analysis of supporting evidence insightfully and provides specific examples with relevance. Level of detail is appropriate.
Strategies the Facility Utilizes to Monitor and Maintain Its Risk Management Program
Criteria Description
Strategies the Facility Utilizes to Monitor and Maintain Its Risk Management Program
A description of the strategies the facility utilizes to monitor and maintain its risk management program is comprehensive. The submission incorporates analysis of supporting evidence insightfully and provides specific examples with relevance. Level of detail is appropriate.
Assessment of the Risk Management Program Inclusive of Health and Legal Concerns
Criteria Description
Assessment of the Risk Management Program Inclusive of Health and Legal Concerns
An assessment of the risk management program inclusive of high-risk health care and legal concerns is comprehensive. The submission incorporates analysis of supporting evidence insightfully and provides specific examples with relevance. Level of detail is appropriate.
Proposed Action Steps to Improve the Risk Management Program Inclusive of Rationale
Criteria Description
Proposed Action Steps to Improve the Risk Management Program Inclusive of Rationale
An inventory of the proposed action steps to improve the risk management program inclusive of rationale is comprehensive. The submission incorporates analysis of supporting evidence insightfully and provides specific examples with relevance. Level of detail is appropriate.
Thesis Development and Purpose
Criteria Description
Thesis Development and Purpose
Thesis is comprehensive and contains the essence of the paper. Thesis statement makes the purpose of the paper clear.
Argument Logic and Construction
Criteria Description
Argument Logic and Construction
Clear and convincing argument presents a persuasive claim in a distinctive and compelling manner. All sources are authoritative.
Mechanics of Writing (includes spelling, punctuation, grammar, language use)
Criteria Description
Mechanics of Writing (includes spelling, punctuation, grammar, language use)
Writer is clearly in command of standard, written, academic English.
Paper Format (use of appropriate style for the major and assignment)
Criteria Description
Paper Format (use of appropriate style for the major and assignment)
All format elements are correct.
Documentation of Sources
Criteria Description
Documentation of Sources (citations, footnotes, references, bibliography, etc., as appropriate to assignment and style
Sources are completely and correctly documented, as appropriate to assignment and style, and format is free of error.
HLT308 WEEK 5(A) Educational Program on Risk Management Part Two – Slide Presentation
Assessment Description
The purpose of this assignment is to create an educational risk management presentation.
Building upon the outline for an educational session you created in the Educational Program on Risk Management Part One: Outline of Topic 2 assignment, develop a 12-15 slide PowerPoint presentation that expands in greater detail on how and why your organization should implement your proposed risk management strategy. Incorporate any instructor feedback from the Topic 2 assignment into this presentation and include talking points in the speaker notes section of each slide.
Keep in mind that the PowerPoint is meant to serve as a visual aide to bolster your presentation and is intended to highlight main ideas and key points. Do not use dense blocks of text or more than 7 bullet points of text per slide. However, you may include supplementary images, graphs, and data where relevant.
To successfully complete this assignment, include the following sections as per your outline from Topic 2, though you may include any additional sections as needed:
- Introduction
- Rationale
- Support
- Implementation
- Challenges
- Evaluation
- Opportunities
You are required to support your statements with a minimum of six citations from appropriate credible sources.
Refer to the resource, “Creating Effective PowerPoint Presentations,” located in the Student Success Center, for additional guidance on completing this assignment in the appropriate style.
While APA style is not required for the body of this assignment, solid academic writing is expected, and documentation of sources should be presented using APA formatting guidelines, which can be found in the APA Style Guide, located in the Student Success Center.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are not required to submit this assignment to LopesWrite.
REFERENCES MUST BE BETWEEN 2019-2023
Reflective Analysis: Risk Management and the Role of Managed Care
Educational Program on Risk Management Part Two – Slide Presentation – Rubric
View Rubric
Introduction
Criteria Description
Introduction
Introduction slides are informative and thorough in explaining why increased attention to the proposed risk management strategy is needed. Specific examples are provided where appropriate.
Rationale
Criteria Description
Rationale
Rationale slides are informative and thorough in explaining why the proposed risk management strategy is lacking in the selected plan. Specific examples are provided as to how its implementation will better meet compliance standards.
Criteria Description
Support
Support data slides are informative and thorough in showing how the data indicate a need for the proposed risk management initiative. Specific examples are provided where appropriate.
Implementation
Criteria Description
Implementation
Implementation slides are informative and thorough in explaining the specific actionable steps by which the selected health care organization can implement the proposed risk management initiative.
Challenges
Criteria Description
Challenges
Challenges slides are informative and thorough in explaining potential obstacles to the risk management implementation. Slides also provide specific examples of solutions for navigating or preempting predicted obstacles.
Evaluation Strategy
Criteria Description
Evaluation Strategy
Evaluation strategy slides are informative and thorough in providing specific examples of how the evaluation plan will assess alignment with the short-term, long-term, and end goals of the risk management program.
Opportunities
Criteria Description
Opportunities
Opportunities slides are informative and thorough in providing additional risk management improvements along with detailed support for the recommended changes.
Incorporation of Instructor Feedback From Previous Assignment
Incorporation of instructor feedback from previous assignment is comprehensive.
Presentation of Content
Criteria Description
Presentation of Content
The content is written clearly and concisely. Ideas universally progress and relate to each other. The project includes motivating questions and advanced organizers. The project gives the audience a clear sense of the main idea.
Layout
Criteria Description
Layout
The layout is visually pleasing and contributes to the overall message with appropriate use of headings, subheadings, and white space. Text is appropriate in length for the target audience and to the point. The background and colors enhance the readability of the text.
Language Use and Audience Awareness (includes sentence construction, word choice, etc.)
Criteria Description
Language Use and Audience Awareness (includes sentence construction, word choice, etc.)
- 5: Excellent
10 points
The writer uses a variety of sentence constructions, figures of speech, and word choice in distinctive and creative ways that are appropriate to purpose, discipline, and scope.
Mechanics of Writing (includes spelling, punctuation, grammar, language use)
Criteria Description
Mechanics of Writing (includes spelling, punctuation, grammar, language use)
Writer is clearly in control of standard, written, academic English.
Documentation of Sources
Criteria Description
Documentation of Sources (citations, footnotes, references, bibliography, etc., as appropriate to assignment and style)
Sources are completely and correctly documented, as appropriate to assignment and style, and format is free of error. Research and citations are supportive of the rationale presented. Sources are distinctive and addresses all of the issues stated in the assignment criteria.
READ MORE >>
Organizational Systems and Quality Leadership C489 Task 2 Root Cause Analysis � ...
Organizational Systems and Quality Leadership C489 Task 2
Root Cause Analysis – Purpose for conducting an RCA
Root Cause Analysis (RCA) is a systematic retrospective approach of discovery by a team of four to six care professionals across the healthcare institution, which looks into the system flaws that led to an adverse event in care. The RCA process has six steps that are followed in an attempt to identify ways in which the identified flaws might be corrected by a process improvement plan to prevent a reoccurrence (Institute for Healthcare Improvement [IHI], n.d. – b).
A1. RCA Steps – The 6 steps of the Institute for Healthcare Improvement (IHI) RCA
There are six steps to an RCA as defined by the IHI; One, identify what happened. Two, determine what should have happened, Three, determine the factors that led to the event. Four, determine what effect each factor caused that contributed to the cascading string of events that ultimately resulted in the adverse event in the first place. Five, generate a recommended action list to prevent the event from occurring again. Six, write a summary and share it with all departments and care teams to assist knowledge and process to prevent the adverse event from re-occurring in the healthcare system as a whole (IHI, n.d. – b).
A2. Causative and Contributing Factors – Factors leading to the sentinel event
Step One: The 67-year-old male patient with a simple left hip fracture was over sedated, improperly monitored and stopped breathing. The over sedation led to a depressed respiratory response and cessation of breathing which resulted in ventricular fibrillation, leading to cardiac arrest and eventual brain death due to anoxic brain injury. The patient’s brain death and removal from artificial life-sustaining ventilation led to his subsequent death (Western Governors University [WGU], n.d.).
Step Two: Instead of death the patient should have received conscious sedation and reduction of his left hip while having continuous electrocardiography (ECG) monitoring, blood pressure (BP) monitoring, and pulse oximeter monitoring administered by available respiratory therapy staff until fully awake with stable vital signs (VSS), no nausea or vomiting (N/V), and able to void per hospital policy, then sent home for full recovery (WGU, n.d.).
Step Three: The multifactorial errors leading to this event include; Concomitant ordering and administration of benzodiazepine and opioids. The ordering and administering of a double or second dose of concomitant benzodiazepine and opioids in a short time frame from the first administration is a contributing error, essentially doubling down on the first error. Not adhering to the hospital’s standard protocol for conscious sedation monitoring is another significant factor that led to harm in this case. Not summoning the extra available nursing and respiratory staff when a new emergency was inbound, caused the existing staff to become distracted with other care duties and contributed to errors in this case. Not placing the at-risk patient on oxygen was another factor in the string of events. Simply resetting the oximetry alarm was another error. Not calling a rapid response immediately when the patient’s oximetry reading was 85% was yet another significant error (WGU, n.d.).
Step Four: The effects each error caused were significant. None was more significant than the first by not following hospital protocol for conscious sedation; however, each subsequent error compounded the first error. Concomitant ordering and administration of benzodiazepine and opioids are known respiratory depressive medications, double dose administrations of those concomitant medications within minutes of the first concomitant medication administration acted dramatically to quickly depress the 67-year-old patient’s respiratory system to such a degree that the patient experienced complete respiratory failure and cardiac arrest via atrial fibrillation within 8 minutes from the RN’s last assessment. The resulting respiratory failure likely resulted in cardiac arrest via atrial fibrillation which stopped blood flow to the brain resulting in brain anoxia and ultimately led to the brain death of the patient (WGU, n.d.).
According to Beers criteria, benzodiazepine muscle relaxants like diazepam are not recommended for use in older adults due to their sedative effects, thus the physician should have considered other alternatives (Arnstein, 2010). The physician additionally ordered the sedating medication oxycodone concomitantly, not just once, but two times within minutes of each other (WGU, n.d.). The physician and registered nurse both should have been aware of warnings by the Food and Drug Administration (FDA) and the manufacturers of diazepam against concomitant use of benzodiazepines and opioids and utilized a more conservative approach to this patient’s sedation needs but did not, leading to eventual respiratory failure (Chaverneff, 2019; WGU, n.d.).
The registered nurse should have questioned the physician on ordering concomitant double doses of oxycodone and diazepam (WGU, n.d.). In questioning the doctor’s initial order the RN could have averted disaster and prevented error. The RN had the opportunity to question his second such order and could have prevented the dangerously sedative combination of medications given to this older adult patient for the second time within minutes of the first concomitant administration (Arnstein, 2010).
Even after administering the concomitant double doses of oxycodone and diazepam, the registered nurse likely could have averted the remaining cascade of events if she had placed the patient on the hospital’s standard protocol for conscious sedation monitoring. Additionally, even if the RN did not follow the hospital’s standard protocol implementation, she likely could have averted disaster had she placed the patient on oxygen due to the known respiratory depressive nature of the drugs she administered.
Respiratory therapy and extra nursing staff should have been summoned when it became apparent that another emergency patient was inbound to insure the existing patients’ stability was being appropriately and safely monitored and disaster may have been averted.
The LPN should have fully assessed the patient and called for help when the oximetry alarm first went off rather than simply resetting it, which led to the patient’s ultimate respiratory failure and anoxic brain damage. Had the LPN fully assessed the patient and noted the depressed or absent respirations she could have called for a rapid response minutes before it was eventually called, and possibly averted anoxic brain damage in the patient.
The combination of oxycodone and diazepam may have been the trigger for eventual respiratory failure, however, the lack of respiratory and ECG heart rate monitoring to prevent respiratory failure is the most significant error in the cascade of events that led to this patient’s demise. The nursing staff was operating blind without a full picture of the patient’s condition due to a lack of following the hospital’s standard protocol for conscious sedation ECG monitoring or patient respirations (WGU, n.d.). Had the nursing staff had the appropriate respiratory therapy staff and ECG monitors in place, the rapid respiratory and cardiac failure could have been averted.
- Improvement Plan – Process Improvement Plan (IP) “Action Plan” to prevent reoccurrence
The most preventable error that occurred was the medical doctor and registered nurse not following hospital protocol for conscious sedation of the patient (WGU, n.d.). The simple act of ensuring the patient received the hospital’s protocol of continuous electrocardiography (ECG) monitoring, blood pressure (BP) monitoring, and pulse oximeter monitoring administered by available respiratory therapy staff until they are fully awake with stable vital signs (VSS), and no nausea or vomiting (N/V), is the needed IHI process improvement “action plan” (WGU, n.d.; IHI, n.d. – b).
The proposed action plan would involve one simple change; a software upgrade to the electronic health record (HER) medication administration record (MAR). The change would disallow the procedure from starting when conscious sedation is chosen as the means of sedation unless the respiratory therapy staff authenticates as a double witness, with the physician or registered nurse, that the hospital protocol is in place before the computer system will allow administration of any sedating medications. This one simple improvement action plan would ensure that the procedure could never start unless the respiratory therapy staff was on location and had authenticated the procedure for conscious sedation with appropriate monitoring.
B1. Change Theory – Phases of Lewin’s Change Theory and implementation within the IP
Kurt Lewin broke the idea of change into three (3) distinct phases: Unfreezing, Change, and Refreezing (Schein, 1999). The step of Unfreezing may cause resistance against the proposed change because individuals are frozen, or aligned to a specific and particular way of doing things, their current homeostasis. Change involves creating a new pattern towards a new equilibrium, a new homeostasis or new normal. Refreezing is achieved when the new pattern becomes the norm, homeostasis, and current reality of doing (Schein, 1999).
For the IP in this scenario, the following aspects of Lewin’s phases of change are described with strategies for utilizing his theory to implement a new action plan to ensure the hospital protocol is utilized every time a patient requires conscious sedation;
Stage 1- Unfreezing:
Hospital administration will implement mandatory attendance to an education forum on conscious sedation and review the sentinel event that resulted in the death of a patient. During education, the new EHR software module will be rolled out and individual computer stations will be available to each employee participant to walk through each step of the process with a conscious sedation practice patient. The steps will include the medical provider entering a standard order for conscious sedation. The standard order will notify the respiratory therapist and registered nurse that the procedure for their patient is due now.
Each participant, the physician, registered nurse, and respiratory therapist will arrive at the practice patient. The registered nurse will scan the patient armband then click on the conscious sedation order to administer the ordered medications. Up will pop a required authentication for the respiratory therapist to authenticate his/her presence and affirm that continuous electrocardiography (ECG), blood pressure (BP), pulse oximeter monitoring is in place and functioning for the procedure. Once the respiratory therapist has authenticated his/her presence and affirmed that protocol equipment is in place, then and only then will the registered nurse or physician be able to administer any medication for conscious sedation, ensuring that at no time does any patient risk unmonitored respiratory or cardiac failure without immediate notice by lifesaving professionals while sedating and respiratory depressing medications are being administered.
The authenticated software will then allow the scanning of the required medications for conscious sedation and the registered nurse will then be able to administer them per orders. In this way, the team of medical professionals can practice care in a fail-safe way of providing conscious sedation within the hospital policy to prevent adverse events of unmonitored respiratory or cardiac failure during or throughout recovery from a procedure. This change will enable the hospital system and healthcare team to achieve the desired outcome of safe conscious sedation during the change process towards full adoption of the change, from test pilot to full implementation.
Stage 2 – Change:
Implementation of change involves a new way of doing things and eventual acceptance of this new way. In this stage, people are unfrozen from the way they previously did things and begin doing them differently. This is the stage in which people are unfrozen, and implement the change to a new and better way of doing things. Great care must be taken during this stage to have clear communication, to ally people’s fear regarding the change and to ensure that no consequences occur for mistakes during change adoption.
This is the stage in which hospital leadership must take great care to listen to the providers that are required to do actual work under the newly proposed action plan (Schein, 1999). The observational team will have to visually watch the steps of the process, listen to feedback from participants using the system and modify or revise steps to ensure the implemented action plan meet the needs of the providers caring for patients, all while meeting the purpose for the change; meeting the goal of successful conscious sedation protocol implementation for every patient that requires it.
In the change phase, the process moves from the piloting phase into full system-wide implementation. The change occurs over a short time, but change can cause resistance from participants as they move from the way they used to do things, to the new way of doing things (Schein, 1999). When participants begin to embrace the change and more fully understand its merits, then the action plan can move from change into the final phase of refreezing.
Stage 3 – Refreezing:
Refreezing occurs when the entire staff moves from the stage of transition (change) to a much more stable state of equilibrium in which people accept, embrace and or internalizes the new way of doing things. The stage of Refreezing is the ultimate stage in which people accept or internalize the new ways of working and have fully adopted the change. Refreezing becomes the new normal, the new homeostasis, the way to do things (Schein, 1999).
- General Purpose of FMEA – Purpose of FMEA
The Fail Modes and Effects Analysis (FMEA) is a systematic and proactive approach to evaluate a process by a team of individuals and invested stakeholders. The FMEA attempts to identify areas of a process that might fail and attempts to consider a deeper look into how and why a step or entire process might fail. Further, the FMEA also seeks to determine the effect a particular failure might have on the desired outcome. The FMEA is preventive in nature seeking to identify potential areas that may fail before they do. Lastly, the FMEA seeks discovery into the parts of the process needing to be re-worked for the entire process to be successful (Institute for Healthcare Improvement [IHI], n.d. – a; Schneider, 2017).
C1. Steps of FMEA Process
The first step of the FMEA is to select a process to be evaluated, either a new process before it is implemented, or an existing or modified process. The second step is to recruit a multidisciplinary team for the evaluation including those that will implement the process; those with specialized knowledge, and others that may be necessary for ultimate success. The third step is to list all the steps in the process that are to be evaluated. The fourth step is to list all the failure modes, their causes, and their effects. As part of the identification of potential failure modes, the team will assign ratings for likelihood the failures will occur, be detected, and how severe a particular failure will be. The team will then assign a risk priority number (RPN) and identify actions to reduce the occurrence of a failure mode from being realized. The fifth step would be for the team to use the RPNs to plan improvements to a particular step or steps in the process to increase the viability of the overall process by starting with the failure mode with the highest RPN. The team would then seek to address the areas within the highest RPN steps within the newly designed process and implement modifications or changes to those areas to mitigate the possibility of failure in the high-risk steps of the new process (IHI, n.d. – a).
The members of the team would typically involve key stakeholders for the process change with specific knowledge of the various areas that will be disrupted. For this scenario, physicians, nurses, respiratory therapists, nurse managers, physician managers, technology specialists, and hospital administrators would be involved in the action plan implementation.
C2. FMEA Table – Steps, failure modes, scales of severity, occurrence, and detection identified
Steps in the Improvement Plan Process:Failure ModeLikelihood of Occurrence (1-10)Likelihood of Detection (1-10)Severity (1-10)Risk Priority Number (RPN)1 Mandatory attendance to new software double verification trainingNot all RN, RT and MD participants are trained5161502 RN & RT notified of sedation procedure and arrive togetherEither the RN or RT does not arrive together in a timely manner6182883 Conscious Sedation Protocol dual Authentication confirmed by RTRT brings all equipment, ECG, Pulse Oximeter and BP monitor216244 Medication administered by RN with protocol monitoring by standby RTRN waits for RT to authenticate protocol before giving meds1133Total RPN (Sum of all RPN’s): 447
(IHI, n.d. – a)
- Intervention Testing – Steps of pilot testing on proposed interventions to improve care
To test-pilot the interventions, I would engage the Emergency Department (ED) first. The ED has one of the highest likely needs for conscious sedation of patients. Further, provider engagement would likely be higher in the ED due to the fact that the prior sentinel event occurred to one of their patients.
After mandatory in-person training and confirmation that all medical providers have completed the test-patient training and are familiar with the new software double verification authentication procedure, roll out of the new process could occur.
Part of the test-pilot roll out would include an observation team made up of the ED Nurse Manager and Medical Director for oversight on each of the first ten (10) conscious sedation patients. The oversight team will be utilized to verify that the new steps are working as planned and that staff has the needed support and supplies to implement the plan seamlessly for each patient.
Upon first notification by a physician that orders have been written for a conscious sedation procedure, the observation team would verify the time of response from order placement in the Electronic Health Record (EHR) by the prescribing provider to the acknowledgment by the RN. Secondarily the observation team would verify the time it takes the RN and RT to jointly arrive at the patient bedside with ECG, BP and Pulse Oximetry monitoring equipment. The upon placement of the ECG, BP and Pulse Oximetry monitoring equipment, the team would then observe any challenges the RN or RT face in double verification before medication administration could occur.
Upon successful conscious sedation verification by the physician, the ordered procedure would begin and be completed by the physician and other providers, and monitoring would be continued by the RN and RT, to ensure continuous BP, ECG, and pulse oximetry monitoring is maintained until the patient is symptom free, fully awake, with VSS, no N/V, and able to void per hospital policy.
If any hiccups are noted and changes are required after the first ten patients, the FMEA table would be redone and procedures modified until the FMEA team is confident the process has been successfully implemented. Based on a successful pilot or re-pilot of the proposed change and implementation system-wide, patients requiring conscious sedation before a procedure starts will receive better care because; no sedating medications can be administered without proper respiratory and cardiac monitoring equipment having been dually verified as onsite and are monitoring appropriately.
- Demonstrate Leadership – Professional nurse leadership competencies in an action plan
Any nurse can be an advocate for improvement in an action plan. It is a natural part of their role to show professional leadership competencies in the promotion of quality care for the patients they serve. The increase in quality care will result in improved patient outcomes. Improved patient outcomes will further fuel their keen eye in spotting areas where quality improvement initiatives can be implemented system-wide under their leadership and direction.
Promoting Quality Care:
During the course of change, any nurse can demonstrate professional leadership and actively lead in a myriad of ways relative to the process of and for change. As a natural part of their function, nurses are front line advocates for quality patient care. Nurses assess and field patient’s needs in an ongoing manner throughout their shifts. As such, nurses are often the first voice for change because they see firsthand the inefficiencies of the healthcare system and are ever seeking to improve the quality of care they deliver. They are often the first voice pressing forward their ideas to improve the quality of care being delivered by the entire team and healthcare system. Secondarily their licensure and jobs are at stake if care is subpar so they are ever pressing forward quality care ideas to ensure improvements are realized for nursing staff, and the patients they care for.
Improving Patient Outcomes:
Nurses see firsthand what poor care looks like, whether it is personal patient self-care or community-based deficits of care and are therefore seeking to improve patient outcomes in a full scope quality improvement manner, not just the care they deliver in-house. Patient outcomes cannot occur without proper nurse-led patient healthcare education and instruction for care by the nurse involved in care. Patient outcomes are improved by daily reinforcement by the nurse of the needed lifestyle changes a patient faces to make a lasting change in their lives. The continuous reinforcement changes the trajectory of a patient’s lifestyle activities from one that originally resulted in that patient’s hospitalization to a new and improved set of lifestyle choices. While the nurse is not always successful in establishing an ingrained acceptance by the patient for a new set of lifestyle choices, the nurse’s advocacy does improve overall outcomes.
Nurse-led Quality Improvement:
Nurses are frequently involved in nurse-led initiates because of these previously mentioned factors. Their initiatives frequently improve patient outcomes and their work is highly influential in shaping quality improvement activities that result naturally in improved fiscal saving to healthcare organizations according to the American Association of Critical Care Nurses (AM Nurse, 2014).
E1. Involving Professional Nurse in RCA and FMEA Processes
As a professional nurse, my utilization of the RCA and FMEA processes was further deepened by taking this course. I was recently involved in an RCA process at my hospital for a patient of mine that fell which resulted in an in-place fracture of her neck. It was very fulfilling to have been in this class and being asked to participate in both the RCA and FMEA processes at work but to also go through the processes of this course work and patient scenario.
As was reiterated in this course, and at my hospital, the RCA and FMEA processes were not in any way punitive towards the caregivers involved in the adverse event but rather were exceedingly beneficial. The entire RCA and FMEA process I went through at my work benefitted the entire hospital and resulted in the implementation of several improvement initiatives regarding what to do after a fall.
Any professional nurse should embrace the use of the RCA and FMEA processes because they are empowering. The RCA and FMEA processes allow any person, but specifically, a nurse caring for their patient, to demonstrate leadership qualities by advocating for process change based on the events leading up to and after an event. A professional nurse will carefully reflect on the RCA and FMEA processes occurring before or after any adverse event to consider all elements for change that could alter or prevent adverse events from occurring in the future.
References
- AM Nurse. (2014). Improved patient outcomes, savings from nurse-led initiatives. American Nurse, 46(4), 4. Available from http://search.ebscohost.com.wgu.idm.oclc.org/login.aspx?direct=true&db=ccm&AN=103909709&site=eds-live&scope=site
- Arnstein, P. (2010). Balancing analgesic efficacy with safety concerns in the older patient. Pain Management Nursing, 11(2), S11–S22. doi:10.1016/j.pmn.2010.03.003
- Chaverneff, F. (2019, January 11). Benzodiazepine and opioid prescribing in the elderly: What are the risks? Retrieved from https://www.clinicalpainadvisor.com/home/conference-highlights/painweek-2017/benzodiazepine-and-opioid-prescribing-in-the-elderly-what-are-the-risks/
- Institute for Healthcare Improvement. (n.d. – a). Failure Modes and Effects Analysis (FMEA) Tool. (n.d.). Available from http://www.ihi.org/resources/Pages/Tools/FailureModesandEffectsAnalysisTool.aspx
- Institute for Healthcare Improvement. (n.d. – b). Patient Safety 104: Root Cause and Systems Analysis. Retrieved from https://srm–c.na60.content.force.com/servlet/fileField?id=0BE0c000000LYai
- Schein, E. H. (1999). Kurt Lewin’s Change Theory in the field and in the classroom: Notes toward a model of managed learning. Reflections, 1(1), 59–74. doi: 10.1162/152417399570287
- Schneider, A. (Producer). (2017, October 31). Failure modes and effects analysis. Available from https://wgu.hosted.panopto.com/Panopto/Pages/Viewer.aspx?id=675fb8c8-60db-49bd-a1e0-d2201cc45c05
- Western Governors University. (n.d.). Patient Scenario. Available from https://tasks.wgu.edu/student/001036767/course/10460005/task/1235/overview
READ MORE >>
