Our Previous Samples
to access the articles will be among the instructional subjects. To establish a ...
READ MORE >>
2019). In the process of facilitating this nurse’s quest for clinical evidenc ...
Best Places to Complete the Search
The nurse has various areas in the workplace where she can find evidence-based information. The library is the first place she could go for this information search. The library has hardcopy guidelines and books. The hospital’s library also contains practice guidelines and hospital protocols for care for common conditions such as sepsis. Therefore
READ MORE >>
NURS-FPX4030 Assessment 1 Locating Credible Databases and Research SOLVED Exampl ...
NURS-FPX4030 Assessment 1 Locating Credible Databases and Research SOLVED Example
Owing to the complexity of the human body and its physiological functions, care must be provided only by professionals and following evidence obtained from the current literature.
Evidence-based practice is applying the best available evidence from any credible source to guide optimal nursing practice, aiming to improve the quality and safety of patient care (Kim et al., 2020).
The ability to use evidence-based evidence necessitates the presence of an experienced practicing healthcare professional who has legitimately gained the credibility to function as a care provider.
Day-to-day challenges for nurses range from making a diagnosis to designing an appropriate care plan for patients. To address this, a nurse must understand how to obtain scholarly resources and identify databases and websites that contain credible medical and nursing data.
As such, the purpose of this paper, with reference to a case scenario provided, is to highlight what it entails in locating evidence in a nursing practice scenario.
Also Read:
NURS-FPX4030 Assessment 2 Determining the Credibility of Evidence and Resources
NURS-FPX4030 Assessment 3 PICOT Questions and an Evidence-Based Approach
NURS-FPX4030 Assessment 4 Remote Collaboration and Evidence-Based Care
Role as a Baccalaureate-prepared Nurse Supervising Clinical Staff Nurses with regard to Communication and Collaboration in Locating Evidence for Application in Nursing Practice Scenario
Summary Brief of the Nursing Practice Scenario
During my duties at a nationally recognized hospital in terms of nursing and medical student education and training, I was assigned to supervise three nurses who work in the medical-surgical department. During daily ward rounds, I assign specific patients to the nurses and participate in my shift report.
A new nurse approaches me, having just completed orientation and training a week before, and expresses his difficulty making a diagnosis in one of the patients assigned to him. Knowing the importance of evidence-based practices in patient outcomes, I am responsible for assisting the nurse in locating the literature that will be useful in caring for the patient.
Communication and Collaboration Strategies
Communication and collaboration are critical pillars of nursing practice that when done well, benefit both patients and caregivers. Because I am responsible for directing the nurses during their clinical rotation, I am responsible for communicating with the one who requires assistance locating evidence-based practice.
First, I would devote time to educating the nurse on evidence-based practice. This will be accomplished by carefully considering both my and the nurse’s schedules and arriving at a convenient time for both of us. A face-to-face communication strategy would be the most effective in conveying the gravity of the situation.
During the meeting, I would be courteous to the nurse and recognize his lack of knowledge as a strength and a need to learn. Even though there is a hierarchical ranking in nursing based on academic and professional achievements, everyone in the healthcare sector is considered a colleague (Schot et al., 2020).
As a result, the decision to communicate with junior colleagues in the most welcoming and cautious manner is informed. Demonstrating kindness and sincerity is an additional communication and collaboration strategy when addressing the issue.
By doing so, I will communicate to the nurse that people progress from ignorance to knowledge and that ignorance is merely an ethereal, transient state that can be corrected. Furthermore, because people have different learning strengths and styles, it is best to hold the meeting in a location where computers and medical databases are easily accessible to demonstrate to the nurse what is expected of her.
Best Places to complete the Research and the Type of Resources to access to find Pertinent Information
Besides being a teaching hospital, the facility also takes pride in having the most modern computer laboratory, where staff can access medical databases whenever they want. Aside from the computer laboratory, each department has its computer and a stable internet connection to assist staff in accessing evidence-based practice data.
The medical-surgical floor, nurses and physician workstations, research department, patient monitoring room, theatre, IT/health informatics room, and imaging department are among the departments with computers and a stable internet that the nurses can use.
While having access to a computer is necessary, the real deal is being able to obtain relevant medical sources and literature from the internet. According to Kim et al. (2020), the search for evidence-based practice information begins with being aware of credible medical databases.
Some online reputable medical databases that will be very useful during this practicum are PubMed, CINAHL, Medline, Google Scholar, ProQuest, and the Cochrane Library.
Assuming the patient has diabetes, the search for evidence-based practice information begins by entering relevant search details into medical databases. The search strategy is important because it determines the types of sources obtained.
Typing the words “diabetes mellitus,” “diagnosis of diabetes mellitus,” “management of diabetes mellitus,” “diabetes mellitus guidelines,” and many other specific word combinations can assist in locating the sources.
Article journals, guidelines from national ministries of health or professional bodies, hospital guidelines and guidebooks, and recommendations or fact sheets from federal agencies like the CDC, as well as information from non-profit health organizations like the American Diabetes Association (ADA), are all resources I would like to find.
Even though the information in the various medical databases has been peer reviewed and is credible, it is up to the searcher to determine the most reliable data.
Five Sources of Online Information used to locate Evidence-Based Practice for the Nursing Practice Scenario.
The five online resources listed below can be used to provide evidence-based valuable information in the management of the assigned patient. Guidelines from the ADA, the International Society for Pediatric and Adolescent Diabetes (ISPAD), and the International Working Group on the Diabetic Foot (IWGDF) are among the sources.
An article journal containing information on insights into diabetes management, as well as an ADA consensus report, are also included. The links to the articles are provided and attached to the reference section, as are the documents. The order in which the sources are arranged below is determined by the relevance and superiority of the information.
- American Diabetes Association. (2020). 8. Obesity management for the treatment of type 2 diabetes: Standards of Medical Care in diabetes-2020. Diabetes Care, 43(Suppl 1), S89–S97. https://doi.org/10.2337/dc20-S008
- Danne, T., Phillip, M., Buckingham, B. A., Jarosz-Chobot, P., Saboo, B., Urakami, T., Battelino, T., Hanas, R., & Codner, E. (2018). ISPAD Clinical Practice Consensus Guidelines 2018: Insulin treatment in children and adolescents with diabetes. Pediatric Diabetes, 19 Suppl 27, 115–135. https://doi.org/10.1111/pedi.12718
- Lipsky, B. A., Senneville, É., Abbas, Z. G., Aragón-Sánchez, J., Diggle, M., Embil, J. M., Kono, S., Lavery, L. A., Malone, M., van Asten, S. A., Urban?i?-Rovan, V., Peters, E. J. G., & International Working Group on the Diabetic Foot (IWGDF). (2020). Guidelines on diagnosing and treating foot infection in persons with diabetes (IWGDF 2019 update). Diabetes/Metabolism Research and Reviews, 36 Suppl 1(S1), e3280. https://doi.org/10.1002/dmrr.3280
- Davies, M. J., D’Alessio, D. A., Fradkin, J., Kernan, W. N., Mathieu, C., Mingrone, G., Rossing, P., Tsapas, A., Wexler, D. J., & Buse, J. B. (2018). Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia, 61(12), 2461–2498. https://doi.org/10.1007/s00125-018-4729-5
- Alam, S., Hasan, M. K., Neaz, S., Hussain, N., Hossain, M. F., & Rahman, T. (2021). Diabetes mellitus: Insights from epidemiology, biochemistry, risk factors, diagnosis, complications, and comprehensive management. Diabetology, 2(2), 36–50. https://doi.org/10.3390/diabetology2020004
Why the Sources provide the Best Evidence for the Chosen Diagnosis
The sources used are from the most reliable medical databases and were authored by medical experts. Furthermore, some of the sources come from internationally recognized health organizations that have long been trusted to provide reliable medical information. Moreover, the sources chosen were published within the last five years, ensuring that the information is up to date and applicable in practice. The reasons stated above predict the reliability and credibility of the sources and, thus, why they were chosen to impact practice concerning the nursing practical scenario provided.
Conclusion
Caring for patients necessitates knowledge and expertise in nursing and related fields. Apprenticeship or evidence-based literature can be used to gain knowledge and expertise. As a result, it is critical for a nurse to develop research skills that allow them to search for information online and sift through it to find evidence-based practice data to use.
As part of my job, I assist nurses doing clinical rotations in the medical-surgical department to locate evidence-based practice literature they can implement. Using various communication and collaborative strategies, nurses learn about medical databases, information search strategies, and how to assess the information’s relevance, reliability, and credibility.
NURS-FPX4030 Assessment 1 Locating Credible Databases and Research SOLVED References
- Alam, S., Hasan, M. K., Neaz, S., Hussain, N., Hossain, M. F., & Rahman, T. (2021). Diabetes mellitus: Insights from epidemiology, biochemistry, risk factors, diagnosis, complications, and comprehensive management. Diabetology, 2(2), 36–50. https://doi.org/10.3390/diabetology2020004
- American Diabetes Association. (2020). 8. Obesity management for the treatment of type 2 diabetes: Standards of Medical Care in diabetes-2020. Diabetes Care, 43(Suppl 1), S89–S97. https://doi.org/10.2337/dc20-S008
- Danne, T., Phillip, M., Buckingham, B. A., Jarosz-Chobot, P., Saboo, B., Urakami, T., Battelino, T., Hanas, R., & Codner, E. (2018). ISPAD Clinical Practice Consensus Guidelines 2018: Insulin treatment in children and adolescents with diabetes. Pediatric Diabetes, 19 Suppl 27, 115–135. https://doi.org/10.1111/pedi.12718
- Davies, M. J., D’Alessio, D. A., Fradkin, J., Kernan, W. N., Mathieu, C., Mingrone, G., Rossing, P., Tsapas, A., Wexler, D. J., & Buse, J. B. (2018). Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia, 61(12), 2461–2498. https://doi.org/10.1007/s00125-018-4729-5
- Kim, M., Mallory, C., & Valerio, T. (2020). Statistics for evidence-based practice in nursing (3rd ed.). Jones and Bartlett. https://books.google.at/books?id=5LEEEAAAQBAJ
- Lipsky, B. A., Senneville, É., Abbas, Z. G., Aragón-Sánchez, J., Diggle, M., Embil, J. M., Kono, S., Lavery, L. A., Malone, M., van Asten, S. A., Urban?i?-Rovan, V., Peters, E. J. G., & International Working Group on the Diabetic Foot (IWGDF). (2020). Guidelines on the diagnosis and treatment of foot infection in persons with diabetes (IWGDF 2019 update). Diabetes/Metabolism Research and Reviews, 36 Suppl 1(S1), e3280. https://doi.org/10.1002/dmrr.3280
- Schot, E., Tummers, L., & Noordegraaf, M. (2020). Working on working together. A systematic review of how healthcare professionals contribute to interprofessional collaboration. Journal of Interprofessional Care, 34(3), 332–342. https://doi.org/10.1080/13561820.2019.1636007
NURS-FPX4030 Making Evidence-Based Decisions Instructions
NURS-FPX4030 Assessment 1 Locating Credible Databases and Research SOLVED Introduction
Welcome to your Capella University online course, NURS-FPX4030 – Making Evidence-Based Decisions
Baccalaureate-prepared nurses use the best available evidence in the processes of clinical reasoning and judgement, which lead to interventions that result in desired patient, systems, and population outcomes.
This course focuses on the development of generalist nursing practice competencies for evidence-based decision making. In this course, you will access a variety of databases and other sources of evidence. By analyzing the credibility of evidence, you will work toward defining evidence-based solutions and plans to improve outcomes in care.
NURS 4030 Assessment 1 Supporting Resources
Related resources are provided for each assessment. Additional resources that may be useful throughout your courses have been gathered for easy access. Refer to the link in the courseroom navigation panel to access these resources.
Kaltura Activities
For one of the assessments in this course, you are required to create a video recording using Kaltura or similar software. Refer to Using Kaltura for more information about this courseroom tool.
To create your recording, you will need a built-in or external microphone and, for video, a webcam.
Note: If you require the use of assistive technology or alternative communication methods to participate in this activity, please contact DisabilityServices@Capella.edu to request accommodations.
Your Online ePorfolio
Creating an ePortfolio is not required in the BSN program, but you may find it helpful to create one to attach to your professional resume while job hunting. Online ePortfolios serve two key purposes: 1) to support learning and reflection, and 2) to be used as a showcase tool.
Your learning journey can be documented, and ePortfolios contribute to lifelong learning and growth through reflection and sharing. Online ePortfolios can also be shared with employers and peers to present artifacts that demonstrate your accomplishments at Capella.
Using ePortfolio to Build Your Career
As you are preparing to tell your story in the professional world, leverage your ePortfolio artifacts to demonstrate the knowledge and competencies you have gained through your program in professional conversations, performance reviews, and interviews.
To do that, reflect on the knowledge and skills you have gained from your courses and the elements you have put in your portfolio, along with how you have already applied these things to your professional life or how you might apply them in the future.
Next, create your story or talking points to tell your professional story.
Saving Your Documents to ePortfolio
You will need a place to store your documents in an organized fashion so that you can access them at a later date. Do not rely on the courseroom to store your assignments for you as you will lose access to the courseroom after you have completed the course. Capella uses a cloud-based portfolio platform to facilitate your organization of the artifacts you create throughout your program.
To make an online portfolio useful, it is essential that it is organized clearly and that important files of any format are accessible. Read the Online ePortfolio Guidelines [PDF] to ensure you set up your online portfolio correctly. For more information on ePortfolio, visit the Campus ePortfolio page.
Privacy Statement
Capella complies with privacy laws designed to protect the privacy of personal information. While you may voluntarily share your own information publicly, you are obligated to protect the personal information of others that may be associated with your academic or professional development.
Before sharing information and material in any ePortfolio that is set up to be shared externally to your program at Capella, please consider privacy obligations in relation to protected populations who may be included or referenced in your academic or clinical work.
Refer to the Family Educational Rights and Privacy Act (FERPA) and/or the Health Insurance Portability and Accountability Act (HIPAA) if you have specific questions or concerns about your choices.
Course Competencies
To successfully complete this course, you will be expected to:
- Interpret findings from scholarly quantitative, qualitative, and outcomes research articles and studies.
- Analyze the relevance and potential effectiveness of evidence when making a decision.
- Apply an evidence-based practice model to address a practice issue.
- Plan care based on the best available evidence.
- Apply professional, scholarly communication strategies to lead practice changes based on evidence.
NURS 4030 Assessment 1 : Locating Credible Databases and Research Instructions
Create a 2-4 page resource that will describe databases that are relevant to EBP around a diagnosis you chose and could be used to help a new hire nurse better engage in EBP.
NURS 4030 Assessment 1 Introduction
Evidence-based practice (EBP) integrates the best evidence available to guide optimal nursing care, with a goal to enhance safety and quality. EBP is crucial to nursing practice because it incorporates the best evidence from current literature, along with the expertise of the practicing nurse. The concern for quality care that flows from EBP generates a desired outcome.
Without these factors, a nurse cannot be an effective leader. It is important to lead not only from this position but from knowledge and expertise. To gain the knowledge, you require a good understanding of how to search for scholarly resources, as well as identify which databases and websites are credible for the purposes of implementing evidence-based changes in practice.
Your Online e-Portfolio
Creating an ePortfolio is not required in the BSN program, but you may find it helpful to create one to attach to your professional resume while job hunting. Online ePortfolios serve two key purposes: 1) to support learning and reflection, and 2) to be used as a showcase tool.
Your learning journey can be documented, and ePortfolios contribute to lifelong learning and growth through reflection and sharing. Online ePortfolios can also be shared with employers and peers to present artifacts that demonstrate your accomplishments at Capella.
Professional Context for NURS-FPX4030 Assessment 1 Locating Credible Databases and Research SOLVED
As a baccalaureate-prepared nurse, you will be responsible for providing patient-centered, competent care based on current evidence-based best practices. You will be required to do research, analysis, and dissemination of best evidence to stay abreast of these best practices. Understanding where to go to find credible sources and locate evidence, as well as which search terms to use, is the foundation of incorporation of best practices.
Scenario to use in NURS-FPX4030 Assessment 1 Locating Credible Databases and Research SOLVED
You are supervising three nurses working on the medical-surgical floor of a local teaching hospital. This hospital is nationally recognized as a leader in education and has a computer lab with an online library where staff has access to medical research databases (that is, CINAHL, PubMed, Medline, and Cochrane library) and online sources of all hospital policies, procedures, and guidelines, and computers at nurse workstations that also have access to these resources.
(For this scenario, use the Capella University Library to simulate the hospital’s online library.) You have given the nurses their patient assignments and you have all participated in shift report.
A new nurse who just completed orientation and training a week ago approaches you and tells you that one of the assigned patients has a diagnosis he or she is very unfamiliar with. Knowing that patient-centered care based on best practices is imperative to positive patient outcomes, you want to assist this nurse to find research that can be utilized to provide the best care for this patient.
Describe how you would communicate with this nurse to encourage him or her to research the diagnosis. Assume you will assist in the quest to locate evidence, then describe where you would go within the facility and what resources you would look for. These resources may include websites, journals, facility policies or guidelines, or any other sources of online information.
You may choose the diagnosis for the patient in this scenario or health care issue/diagnosis of your choice. Or you may choose something you would find interesting to research or that applies to a clinical problem/diagnosis you would be interested in addressing.
Create a list of at least five sources that could be used to find evidence, with the best source listed first, and explain why the sources you chose are best to find evidence for the diagnosis you chose and the clinical scenario.
You are only evaluating the sources of evidence (database, website, policy database or website, journal article, et cetera). You are not actually completing a search and selecting evidence. Consider the following examples: a nursing journal in CINAHL may not be the best source of evidence for information on how to administer medications through a central-venous catheter, whereas a hospital policy database found on a website may not be the best source of information on caring for a patient with a rare chromosomal abnormality.
Preparation for NURS-FPX4030 Assessment 1 Locating Credible Databases and Research SOLVED
To help ensure you are prepared to complete this assessment, review the following resources related to the Capella library. These resources will provide you an overview of the types of tools, resources, and guides available in the library. This may be useful in forming a better understanding of the library to apply to the hypothetical situation laid out in the scenario of this assessment.
- BSN Program Library Research Guide.
- Evidence-Based Practice in Nursing & Health Sciences.
- Databases A-Z: Nursing & Health Sciences.
- Get Critical Search Skills.
Remember, it is also appropriate to look toward databases and resources outside of the Capella library, such as organizational policies, professional organizations, and government health care resources.
You are encouraged to complete the Evaluating the Credibility of Evidence activity. This activity offers an opportunity to practice evaluating the credibility of evidence. These skills will be necessary to complete Assessment 1 successfully and is for your own practice and self-assessment. Completing this activity is also a way to demonstrate course engagement.
NURS-FPX4030 Assessment 1 Locating Credible Databases and Research Instructions
The purpose of this assessment is to understand where to find evidence that can be applied to clinical scenarios and to learn effective communication and collaboration with clinical staff during the process of evidence location. As a baccalaureate-prepared nurse, you will not only use research for self-improvement in your clinical role, but you will also serve as a mentor to supervised nursing staff.
Therefore, you will need to be able to communicate and collaborate effectively to guide them toward resources to find research, as well as support them through the initial evidence location process. In doing so, nurses can gain access to evidence that can be analyzed and utilized to stay current on best practices. This allows them to provide safe, patient-centered care and improve patient outcomes.
For this NURS 4030 Assessment 1 assessment:
- Describe your role as a baccalaureate-prepared nurse supervising clinical staff nurses with regard to communication and collaboration in locating evidence for application to a nursing practice scenario.
- Compile a list of five online databases or other online sources (that is, websites, journals, facility policies or guidelines, et cetera) that can be used to research evidence to apply to this scenario or clinical practice issue/diagnosis and describe to which of these you would direct a nurse colleague to search for evidence.
- Describe where you might go in the work place to complete this research and how you would access the desired, relevant research within research databases or other online sources.
Be sure to address the following in this assessment, which correspond to the grading criteria in the scoring guide. Please study the scoring guide carefully so that you will know what is needed for a distinguished score.
- Describe communication strategies to encourage nurses to research the diagnosis/practice issue, as well as strategies to collaborate with the nurses to access resources.
- Describe the best places to complete research and what types of resources you would want to access to find pertinent information for the diagnosis/health care issue within the context of a specific health care setting.
- Identify five sources of online information (medical journal databases, websites, hospital policy databases, et cetera) that could be used to locate evidence for a clinical diagnosis/practice issue.
- Explain why the sources of online information selected should provide the best evidence for the chosen diagnosis/health care issue.
- Communicate using writing that is clear, logical, and professional with correct grammar and spelling using current APA style.
Note: While you are not selecting and evaluating specific evidence to help with the clinical diagnosis/practice issue, you should still be citing the literature and best practices to support your description of your communication and collaboration approach.
Additionally, it is appropriate to cite best practices related to EBP and evaluating databases to support your explanation as to why you selected the five sources of online information that you did.
Example Assessment: You may use the following to give you an idea of what a Proficient or higher rating on the scoring guide would look like:
- Assessment 1 Example [PDF].
Additional Requirements
Your assessment should meet the following requirements:
- Length of submission: 2-4 pages (not including the title page or the reference page) description of communication, collaboration, and evidence location process, including a list of databases or other sources with description of why they are appropriate for clinical scenario diagnosis/health care issue (that is, something that would be useable in professional practice for other nurses). Be sure to include an APA-formatted reference page at the end of your submission.
- Number of references: Cite a minimum of three sources of scholarly or professional evidence that supports your findings and considerations. Resources should be no more than five years old.
- APA formatting: References and citations are formatted according to current APA style.
Competencies Measured

By successfully completing this assessment, you will demonstrate your proficiency in the course competencies through the following assessment scoring guide criteria:
- Competency 1: Interpret findings from scholarly quantitative, qualitative, and outcomes research articles and studies.
- Explain why the sources selected should provide the best evidence for the chosen diagnosis/health care issue.
- Competency 2: Analyze the relevance and potential effectiveness of evidence when making a decision within the context of a specific health care setting.
- Describe the best places to complete research within the workplace environment and what types of resources one would want to access to find pertinent information for the diagnosis/health care issue.
- Competency 4: Plan care based on the best available evidence.
- Identify five sources of online information (medical journal databases, websites, hospital policy databases, et cetera) that could be used to locate evidence for a diagnosis/health care issue and three out of five should be specific to the diagnosis/health care issue.
- Competency 5: Apply professional, scholarly communication strategies to lead practice changes based on evidence.
- Describe communication strategies to encourage nurses to research a diagnosis/health care issue, as well as strategies to collaborate with the nurses to access resources.
- Organize content so ideas flow logically with smooth transitions; contains few errors in grammar/punctuation, word choice, and spelling.
- Apply APA formatting to in-text citations and references exhibiting nearly flawless adherence to APA format.
NURS-FPX4030 Assessment 1 Locating Credible Databases and Research SOLVED Scoring Guide
CRITERIA NON-PERFORMANCE BASIC PROFICIENT DISTINGUISHED
Describe communication strategies to encourage nurses to research a diagnosis, as well as strategies to collaborate with the nurses to access resources. Does not describe communication strategies to encourage nurses to research a diagnosis, as well as strategies to collaborate with the nurses to access resources. Lists communication strategies to encourage nurses to research a diagnosis, as well as strategies to collaborate with the nurses to access resources.
Describes communication strategies to encourage nurses to research a diagnosis, as well as strategies to collaborate with the nurses to access resources. Describes communication strategies to encourage nurses to research a diagnosis, as well as strategies to collaborate with the nurses to access resources. Additionally, notes specific benefits of strategies in helping to build professional competence or a positive professional relationship. Cites literature to support discussion.
Describe the best places to complete research within the workplace environment and what types of resources one would want to access to find pertinent information for a diagnosis. Does not describe the best places to complete research within the workplace environment and what types of resources one would want to access resources to find pertinent information for a diagnosis. Lists the best places to complete research within the workplace environment and what types of resources one would want to access resources to find pertinent information for a diagnosis.
Describes the best places to complete research within the workplace environment and what types of resources one would want to access resources to find pertinent information for a diagnosis. Describes the best places to complete research within the workplace environment and what types of resources one would want to access resources to find pertinent information for a diagnosis. Notes one or more
READ MORE >>
NURS-FPX4030 Assessment 2 Determining the Credibility of Evidence and Resources ...
NURS-FPX4030 Assessment 2 Determining the Credibility of Evidence and Resources Example Paper
Even as patient care evolves and the healthcare transformation is visible, change is a constant factor. With the evolution of disease processes and ingenuity in the mechanisms of some diseases, such as cancer, it is critical and prudent to embrace new practice methods. This calls for the incorporation of evidence-based research findings into nursing practice in the hopes of improving patient care quality and safety.
As the nursing profession evolves and healthcare transforms, more opportunities for nurses to engage in leadership roles that include incorporating evidence-based research findings into practice become available (Kim and colleagues, 2020). To do so, nurses must understand the criteria used to certify the credibility of resources, which is critical in deciding which to use in practice.
As a result, using evidence-based practice models to help nurses incorporate scholarly findings into practice is vital. This analysis aims to determine what factors contribute to the credibility of resources obtained to assist in solving a practical nursing scenario.
Quality, Safety, or a Chosen Diagnosis that could benefit from an Evidence-Based Approach

The chosen diagnosis, diabetes mellitus (DM), serves as the foundation for the subsequent discussion. Diabetes is a chronic metabolic condition characterized by high blood sugar levels caused by a lack of insulin secretion, action, or both. Type 1 diabetes and type 2 diabetes are the most common types of diabetes. Type 1 diabetes is caused by a lack of insulin secretion, which usually occurs due to autoimmune destruction of the beta cells of the islet of Langerhans. Contrarily, while it can also result from insulin deficiency, the vast majority of type 2 DM cases are caused by insulin resistance in the peripheral cells (American Diabetes Association, ADA, 2020).
Diabetes epidemiology, in terms of morbidity, mortality, and treatment costs, reveals the disease’s gravity and the need for evidence-based practice to solve it. According to Sapra and Bhandari (2022), one in every eleven people worldwide has diabetes, with the vast majority (90%) having type 2 diabetes. While type 1 diabetes affects children, adolescents, and young adults, type 2 diabetes primarily affects adults. To account for the predisposition of type 1 diabetes in childhood, Sapra and Bhandari (2022) state that 45% of children with type 1 diabetes present before age ten.
The incidence of type 1 diabetes has been increasing by 2-5 percent per year in Europe, Australia, and the Middle East, and by about 2% per year in most age and ethnic groups in the United States (Sapra & Bhandari, 2022). Type 2 diabetes is estimated to affect approximately 9% of the US population, with a higher prevalence of 25% among those aged 65 and older (Sapra & Bhandari, 2022). Despite the troubling statistics, it is expected that the prevalence of diabetes will rise, with higher-income individuals being disproportionately affected.
According to the World Health Organization, diabetes is the ninth leading cause of death worldwide. Diabetes accounted for 1.37 million deaths from 1990 to 2025, according to a review by Lin et al. (2020), with the number expected to rise to 1.59 million by 2025. Furthermore, on March 22, 2018, the ADA (2018) published new research stating that the total cost of diagnosed diabetes increased to $327 billion in 2017, up from $245 billion in 2012. According to this discovery, diabetes imposes a significant economic burden on society.
In addition to the complications that diabetes causes, both acute and long-term, it is only logical that an evidence-based approach is developed to reduce its burden. The good news is that most DM risk factors are avoidable and can be significantly reduced when preventive measures are implemented using evidence-based strategies. Besides being useful tools for comparing and contrasting health events and populations, analyzing diabetes morbidity, mortality, and cost trends can help determine the most appropriate health interventions for a specific population.
Criteria for Determining Credibility of Resources
It is critical to follow a specific criterion when determining the credibility of a resource. The criterion includes evaluating the resources’ currency, relevance, authority, accuracy, and purpose (CRAAP) (Columbia College, 2022). Currency refers to the resource’s timeliness, and a journal article or website published within the last five years is often recommended first.
The importance of a resource for the researcher’s needs is referred to as its relevance, and the most helpful question to ask is whether the information relates to the topic or answers the researcher’s question (Columbia College, 2022). Concerning the authority, who is the resource’s author, what are their credentials, and with which organization is the author affiliated? In terms of medical and nursing knowledge, the author should, at the very least, be an expert in a field related to nursing or medicine.
Regarding accuracy, the questions to ask are where the information comes from. Has the information been reviewed, does evidence back it up, or can it be confirmed by another source or personal knowledge? (Columbia College, 2022) Finally, the information’s purpose is an essential factor in determining the resource’s credibility.
Here, the researcher asks whether the information’s purpose is to inform, tell, or educate and whether the intention has been served. Is the information a fact, opinion, or propaganda? Some medical databases have classified journal articles based on their relevance and publication dates, making it easier to determine the credibility of a resource.
Analysis of the Credibility and Relevance of Evidence and Resources within the Context of the Chosen Diagnosis
All of the resources selected to provide evidence-based practice solutions to the patient’s problem are credible and contain high-quality information. All of the sources were authored by experts in various fields of health and were published within the last five years. Furthermore, the information in the sources has been peer reviewed/supported by evidence, making it accurate, relates to the topic and thus relevant, and verified to serve the purpose for which they were intended.
ADA (2020), Alam et al. (2021), Danne et al. (2018), Davies et al. (2018), and Lipsky et al. (2020) all address specifics of diabetes and have all met the CRAAP criteria in assessing credibility. As a result, it is safe to conclude that the sources contain evidence-based information that can be implemented as effective practices in solving the patient’s problem.
Evidence-Based Practice Model and the Importance of Incorporating Credible Evidence into the EBP Model
To use scholarly information, care providers must learn the art of leveraging evidence-based practice models. A potential change to the patient’s solution would be the use of telemedicine to ensure continuous care and education. In this case, translating evidence-based evidence into practice will necessitate using the Ottawa Model, an interactive model for transferring research knowledge into practice (Nilsen, 2020).
In the Ottawa model, the initial procedure for implementing innovation is an assessment of the barriers and supports, followed by monitoring the interventions and the degree of use, and finally, an evaluation of outcomes (Nilsen, 2020). Each stage includes several initiatives to implement innovation or guidelines and increase evidence-based practice across a healthcare setting. As the demand for quality-improvement measures to improve care quality and safety grows, so does the demand for evidence-based models or templates.
Conclusion
Given the changing times and transformations in healthcare, nurses must stay current on practice information. In doing so, nurses benefit greatly from evidence obtained online from reputable medical and nursing databases. On the other hand, obtaining reliable information necessitates understanding the processes of retrieving the sources and assessing their credibility. Therefore, nurses must not only use existing resources but also learn how to find new ones.
Assessing a source’s credibility is a process that requires careful consideration of several factors, such as currency, relevance, accuracy, authority, and purpose. Owing to the burden of diabetes in terms of morbidity, mortality, and cost implications, evidence-based strategies must be implemented to prevent the disease’s consequences for patients and healthcare as a whole. The advancements in technology that can improve the use of telemedicine, as well as the preventable nature of diabetes risk factors that can be leveraged in the fight, provide hope.
NURS-FPX4030 Assessment 2 Determining the Credibility of Evidence and Resources References
Alam, S., Hasan, M. K., Neaz, S., Hussain, N., Hossain, M. F., & Rahman, T. (2021). Diabetes mellitus: Insights from epidemiology, biochemistry, risk factors, diagnosis, complications, and comprehensive management. Diabetology, 2(2), 36–50. https://doi.org/10.3390/diabetology2020004
American Diabetes Association. (2018). Economic costs of diabetes in the U.s. in 2017. Diabetes Care, 41(5), 917–928. https://doi.org/10.2337/dci18-0007
American Diabetes Association. (2020). 8. Obesity management for the treatment of type 2 diabetes: Standards of Medical Care in diabetes-2020. Diabetes Care, 43(Suppl 1), S89–S97. https://doi.org/10.2337/dc20-S008
Columbia College. (2022). Evaluating the Credibility of Your Sources. Columbia College and Columbia Engineering. https://www.cc-seas.columbia.edu/integrity/evaluating-credibility
Danne, T., Phillip, M., Buckingham, B. A., Jarosz-Chobot, P., Saboo, B., Urakami, T., Battelino, T., Hanas, R., & Codner, E. (2018). ISPAD Clinical Practice Consensus Guidelines 2018: Insulin treatment in children and adolescents with diabetes. Pediatric Diabetes, 19 Suppl 27, 115–135. https://doi.org/10.1111/pedi.12718
Davies, M. J., D’Alessio, D. A., Fradkin, J., Kernan, W. N., Mathieu, C., Mingrone, G., Rossing, P., Tsapas, A., Wexler, D. J., & Buse, J. B. (2018). Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia, 61(12), 2461–2498. https://doi.org/10.1007/s00125-018-4729-5
Kim, M., Mallory, C., & Valerio, T. (2020). Statistics for evidence-based practice in nursing (3rd ed.). Jones and Bartlett. https://books.google.at/books?id=5LEEEAAAQBAJ
Lin, X., Xu, Y., Pan, X., Xu, J., Ding, Y., Sun, X., Song, X., Ren, Y., & Shan, P.-F. (2020). Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Scientific Reports, 10(1), 14790. https://doi.org/10.1038/s41598-020-71908-9
Lipsky, B. A., Senneville, É., Abbas, Z. G., Aragón-Sánchez, J., Diggle, M., Embil, J. M., Kono, S., Lavery, L. A., Malone, M., van Asten, S. A., Urban?i?-Rovan, V., Peters, E. J. G., & International Working Group on the Diabetic Foot (IWGDF). (2020). Guidelines on the diagnosis and treatment of foot infection in persons with diabetes (IWGDF 2019 update). Diabetes/Metabolism Research and Reviews, 36 Suppl 1(S1), e3280. https://doi.org/10.1002/dmrr.3280
Nilsen, P. (2020). Overview of theories, models, and frameworks in implementation science. In Handbook on Implementation Science (pp. 8–31). Edward Elgar Publishing. https://doi.org/10.4337/9781788975995.00008
Sapra, A., & Bhandari, P. (2022). Diabetes Mellitus. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK551501/
NURS-FPX4030 Assessment 2 Determining the Credibility of Evidence and Resources Instructions
Develop a 2-4 page scholarly paper in which you describe a quality or safety issue, or a chosen diagnosis, and then identify and analyze credible evidence that could be used as the basis for applying EBP to the issue.
Introduction
The goal of using evidence-based research findings is to enhance safety and quality of patient care and ensure optimal outcomes are achieved. It is not uncommon to hear a nurse say, “why change it as we’ve always done it this way.” However, this is no longer acceptable in today’s practice environment.
The profession of nursing has evolved, and the expectation is that the professional nurse has a scientific foundation to support the care that is provided. As the profession of nursing continues to evolve and engage in health care transformation, baccalaureate-prepared nurses are expanding taking on leadership roles that include incorporating EBPs.
To be able to do this, the nurse needs to understand the criteria and makes a resource credible, as this is crucial when deciding if the research is valid and reliable for implementation into health care settings. The nurse will need to incorporate the use of evidence-based practice models. EBP models are designed to assist the nurse in developing a plan to gather evidence to answer a practice problem or question. It is a systematic approach to direct the user to incorporate scholarly findings into current practice. These EBP models lead the nurse through the decision-making process of evaluating the literature to determine the best practice evidence for the practice issue or question.
It would be an excellent choice to complete the Vila Health Determining the Credibility of Evidence activity prior to developing the report. The activity is a media simulation that offers an opportunity to review a scenario and work on determining the credibility of presented evidence. These skills will be necessary to complete Assessment 2 successfully. This media simulation is one potential source of context on which to base your assessment submission. This will take just a few minutes of your time and is not graded.
Professional Context
As a baccalaureate-prepared nurse, you will be responsible for locating and identifying credible and scholarly resources to incorporate the best available evidence for the purposes of enhancing clinical reasoning and judgement skills. When reliable and relevant evidence-based findings are utilized, patients, health care systems, and nursing practice outcomes are positively impacted.
Scenario
For this assessment, you may choose from the following options as the context for the quality or safety issue or chosen diagnosis/health issue for researching and completing this assessment:
- The specific diagnosis/health issue you identified in your previous assessment.
- The simulation Vila Health: Determining the Credibility of Evidence.
- A personal practice experience in which a sentinel event occurred.
Instructions
The purpose of this analysis is to better understand what constitutes credibility of journal articles as well as websites. The role of the baccalaureate-prepared nurse in incorporating evidence-based research continues to growth in clinical practice. As quality improvement (QI) measures to reduce safety risks continue to be emphasized, the need for evidence-based models and evidence-based templates is growing.
This type of systematic approach to incorporating evidence-based findings allows nurses to make clinical and operational decisions based upon the best available evidence. When the most up-to-date evidence-based findings are utilized, patient-centered care improves outcomes and enhances the patient experience.
Below is a quick review table of several well-known Evidence-Based Practice Models used to guide exploration:
Evidence-Based Practice ModelsIowa Model of Evidence-Based PracticeStetler ModelOttawa ModelPARiHS (Promoting Action on Research Implementation in Health Services) ModelACE (Academic Center for Evidence-Based Practice) Star ModelARCC (Advancing Research and Clinical Practice Through Close Collaboration) ModeJohn Hopkins ModelKTA (Knowledge-to-Action) ModelFor this assessment:
- Explain the criteria that should be used when determining the credibility of journal articles as well as websites.
- Support your explanations with references to the literature or research articles that describe criteria that should be used to determine credibility.
- Your identification and determination of credibility should be done within the context of your chosen scenario for this assessment. For example, if you choose to use the provided Vila Health scenario, your initial identification of resources should be of resources that will best help address the presented issue. However, if you are locating resources to help provide evidence-based care for the diagnosis/health care issue you identified in the first assessment, you may want to begin your literature and evidence search from the databases that were identified. Any of the three scenario options are acceptable. So, pick the one that most interests you.
Be sure to address the following in this assessment, which correspond to the grading criteria in the scoring guide. Please study the scoring guide carefully so that you will know what is needed for a distinguished score.
- Describe a quality or safety issue, or a chosen diagnosis, that could benefit from an evidence-based approach.
- Explain criteria that should be considered when determining credibility of resources such as journal articles and websites.
- Analyze the credibility and relevance of evidence and resources within the context of a quality or safety issue, or a chosen diagnosis.
- This is where you are selecting the specific resources to help address the issue in your chosen scenario.
- Identify the Evidence-Based Practice model and explain the importance of incorporating credible evidence into the EBP model used to address a quality or safety issue, or a chosen diagnosis/health care issue. Review the literature below and choose the appropriate model for your diagnosis/health care issue.
- Selecting a model for evidence-based practice changes. [PDF] and Evidence-Based Practice Models help explain the various evidence-based nursing models.
- Communicate using writing that is clear, logical, and professional with correct grammar and spelling using current APA style.
Additional Requirements
Your assessment should meet the following requirements:
- Length of submission: 2-4-page scholarly paper, this does not include the APA-formatted title page and reference list.
- Number of references: Cite 3-5 sources of scholarly or professional evidence that support your findings and considerations. Resources should be no more than five years old.
- APA formatting: References and citations are formatted according to current APA style.
Portfolio Prompt: Remember to save the final assessment to your ePortfolio so that you may refer to it as you complete the final capstone course.
Competencies Measured
By successfully completing this assessment, you will demonstrate your proficiency in the course competencies through the following assessment scoring guide criteria:
- Competency 2: Analyze the relevance and potential effectiveness of evidence when making a decision.
- Explain criteria that should be considered when determining credibility of resources such as journal articles and websites.
- Analyze the credibility and relevance of evidence and resources within the context of a quality or safety issue, or a chosen diagnosis.
- Competency 3: Apply an evidence-based practice model to address a practice issue.
- Identify an evidence-based practice model (such as Iowa, Stetler, John Hopkins, etc.) and explain the importance of incorporating credible evidence into an EBP model used to address a quality or safety issue, or a chosen diagnosis/health care issue.
- Competency 4: Plan care based on the best available evidence.
- Describe a quality or safety issue, or a chosen diagnosis, that could benefit from an evidence-based approach.
- Competency 5: Apply professional, scholarly communication strategies to lead practice changes based on evidence.
- Organize content so ideas flow logically with smooth transitions; contains few errors in grammar/punctuation, word choice, and spelling.
- Apply APA formatting to in-text citations and references exhibiting nearly flawless adherence to APA format.
Resources: Promoting Evidence-Based Practice
- The resources below explore promoting EBP:
- Conway, A., Dowling, M. & Devane, D. (2019). Implementing an initiative promote evidence-informed practice: part 2—healthcare professionals’ perspectives of the evidence rounds programme. BMC Medical Education, 19.
- This article covers the translation of research into clinical practice and discusses the dissemination and implementation of EBP.
- Pol-Castañeda, S., Rodríguez-Calero, M. Á., Zaforteza-Lallemand, C., Villafáfila-Gomila, C. J., Blanco-Mavillard, I., Ferrer-Cruz, F., & Joan De Pedro-Gómez. (2020). Moving evidence into practice by advanced practice nurses in hospitalization wards. protocol for a multicentre quasi-experimental study in three hospitals in Spain. International Journal of Environmental Research and Public Health, 17(10), 3473.
- This article presents a project that aims to evaluate the impact of the incorporation of the Advanced Practice Nurse role on the implementation of EBP at three levels: Context, nurses’ perceptions, and clinical outcomes.
- Albarqouni L., Hoffmann T., Straus S., Rydland, N., Olsen, N. R., Young, T., Illic, D., Shaneyfelt, T., Haynes, B., Guyatt, G., & Glasziou, P. (2018). Core competencies in evidence-based practice for health professionals: Consensus statement based on a systematic review and Delphi Survey. Journal American Medical Association Network Open, 1(2).
- This article discusses core competencies in evidence-based practice (EBP) that health professionals should meet? Core competencies inform the development of EBP curricula for health professionals. Evidence-based practice (EBP) is necessary for improving the quality of health care as well as patient outcomes.
- Ives E., J. & Pappas, S. (2020). The value of nursing research. The Journal of Nursing Administration, 50(5), 243-244.
- Innovations in patient care, nursing, and the practice environment are hallmarks of organizations receiving American Nurses Credentialing Center (ANCC) Magnet Recognition. This article examines the growing importance of nursing research on patient care and outcomes and the role of Magnet hospitals as research pacesetters for the nursing profession. The authors discuss the critical difference between research and evidence-based practice, why both are important, and how organizations can develop the structures and processes to inspire and advance a robust culture of clinical inquiry.
- Hagle, M., Dwyer, D., Gettrust, L, Lusk, D., Peterson, K., Tennies, S. (2020). Development and implementation of a model for research, evidence-based practice, quality improvement, and innovation. Journal of Nursing Care Quality, 35(2).102-107.
- This article provides a discussion on algorithm with steps and decision points for nurses to follow based on a question from a clinical issue or problem. The model was approved by nursing-shared governance and is used for guiding relevant projects. The I3 Model guides the nurse in inquiry or improvement while supporting a culture of innovation in professional practice.
- Mackey, A. & Bassendowski. S. (2020). The history of evidence-based practice in nursing education and practice. Journal of Professional Nursing, 33(1).51-55.
- This article will discuss evidence-based practice as it continues to advance the nursing discipline. Evidence-based practice is foundational to undergraduate and graduate nursing education and is a way for the nursing discipline to minimize the theory to practice gap. This article discusses the concept of evidence-based practice from a historical perspective as it relates to nursing in the educational and practice domains.
- The concept of evidence-based practice is defined, and the similarities and differences to evidence-based medicine discussed. It is crucial that registered nurses be proactive in their quest for research knowledge, so the gap between theory and practice continues to close. Utilizing nursing best practice guidelines, reviewing, and implementing applicable research evidence, and taking advantage of technological advances are all ways in which nursing can move forward as a well-informed discipline.
- Whalen, M., Baptiste, D., L. & Maliszewski, B. (2020). Increasing nursing scholarship through dedicated human resources. The Journal of Nursing Administration, 50(2). 90-94.
- This article shares as the role of nursing grows in healthcare, the engagement of frontline nurses in evidence-based practice, quality improvement, and research is becoming the expectation and no longer the exception. Clinical nurses are in a unique position to inform and implement scholarly projects. The purpose of this staff development and the capacity-building project was to increase the output of scholarly work among frontline nurses through the formalization of nursing inquiry support via designated nursing inquiry project coordinators.
- Gawlinski, A., & Rutledge, D. (2008). Selecting a model for evidence-based practice changes. [PDF]. AACN Advanced Critical Care, 19(3) 291-300.
- This website explains the various evidence-based nursing models.
- Springer Publishing. (n.d.). Evidence-Based Practice Models. https://connect.springerpub.com/content/book/978-0-8261-2759-4/back-matter/bmatter1
- This website also explains the various evidence-based nursing models.
READ MORE >>
NURS-FPX4030 Assessment 4 Remote Collaboration and Evidence-Based Care Example P ...
NURS-FPX4030 Assessment 4 Remote Collaboration and Evidence-Based Care Example Paper
Hello everyone, and welcome to my presentation. My name is (insert name here). In this presentation, I will use Caitlyn Bergan’s scenario to emphasize the importance of implementing evidence-based practice and encouraging remote collaboration in promoting care quality for patients in remote settings.
Before delving into an in-depth analysis of the case study, it is valid to argue that the Vila health scenario underscores the importance of interdisciplinary collaboration between healthcare professionals, patients, and families in ensuring effective utilization of telemedicine technologies when physical distance is a fundamental factor for quality care delivery. This presentation will explain an evidence-based care plan for Caitlyn while emphasizing the role of interdisciplinary collaboration in promoting telehealth technologies.
Evidence-Based Care Plan

Caitlyn Bergan’s scenario presents various challenges when delivering care for patients with cystic fibrosis in remote settings. Although healthcare professionals at the Valley City Regional Hospital embrace interdisciplinary collaboration to ensure an effective transition for Caitlyn, they are aware of various constraints that hamper telehealth and remote collaboration. For instance, pediatricians, social workers, and nurses are willing to provide education to Caitlyn’s mother (Janice) and coordinate care with caregivers at McHenry. Although they successfully engage Janice through virtual platforms such as Skype, the telemedicine modalities seem insufficient and constrained by inflexible consultation scheduling and communication patterns.
Providing care to cystic fibrosis patients in remote settings requires consistent collaboration and communication between healthcare professionals and home-based caregivers (Desimone et al., 2021). According to Vagg et al. (2021), it is essential to implement interventions such as virtually monitoring adherence to nebulized treatments using telemedicine, installing mobile-health (mHealth) apps to improve patient progress, including nutrition and social welfare, and using teleconferencing platforms such as zoom to maintain interdisciplinary communication.
Although healthcare professionals at Valley City Regional Hospital maintain contact with Janice, additional information regarding strategies to monitor Caitlyn’s medication adherence and effective telehealth alternative tools are necessary for guaranteeing care continuity.
Evidence-based Practice Model for Developing the Care Plan
Johns Hopkins Evidence-Based Practice (JHEBP) model can be ideal in inspiring an evidence-based care plan for Caitlyn Bergan. Dang et al. (2021) argue that the JHEBP framework encourages caregivers to develop clinical questions, select and appraise evidence, and translate information to clinical activities and processes.
This model emphasizes the PET (Practice-Evidence-Translation) strategy that enables nurses to inquire about clinical problems, search and appraise evidence, and translate evidence into practical interventions. Finally, the JHEBP model encourages healthcare professionals to embrace interdisciplinary collaboration when implementing evidence-based practice. As a result, it is ideal for promoting evidence-based practices for delivering care to Caitlyn.
Relevance of the Evidence
Notably, providing care to patients with cystic fibrosis in remote settings by using telehealth modalities requires healthcare professionals to incorporate evidence-based and proven interventions. Johns Hopkins Evidence-Based Practice (JHEBP) model requires nursing researchers to consider sources’ currency, relevance, authority, and precision when appraising them.
Based on these thresholds, I selected studies by Desimone et al. (2021) and Vagg et al. (2021) as ideal evidence sources for informing the evidence-based care plan. According to Desimone et al. (2021), the necessary components for successful telemedicine include the ability to upload self-monitoring information to clinicians, robust internet connectivity, billing systems to ensure reimbursements, Health Insurance Portability and Accountability (HIPAA) compliance, and devices to connect to virtue visits.
On the other hand, the study by Vagg et al. (2021) elaborates on the importance of virtual monitoring of vital signs, utilizing virtual communication tools to track and communicate patients’ adherence to nebulizer treatments, and flexible teleconferencing to maintain consistent and timely communication between healthcare professionals, patients, and caregivers in remote settings. Undoubtedly, it is possible to apply these suggestions when developing a telehealth plan for Caitlyn Bergan.
Benefits and Strategies to Mitigate Challenges in Interdisciplinary Collaboration to Plan Care
Telehealth technologies face multiple challenges that compromise the effectiveness of telemedicine and interdisciplinary collaboration. Weißenfeld et al. (2021) contend that individual and community education levels, connectivity issues, data privacy concerns, economic issues, and unfamiliarity with telemedicine technologies frustrate telehealth.
Healthcare professionals can mitigate these challenges by educating patients, families, and communities on the usability of telemedicine technologies, linking remote communities to available telemedicine resources, implementing flexible virtual consultation schedules, and providing affordable billing alternatives to families to ensure internet connectivity. As I conclude this presentation, it is vital to note that solving telehealth technology problems translates to various benefits, including reducing care costs, improved virtual communication, distant patient diagnostics and treatment, and care continuity.
Thank you for your time
NURS-FPX4030 Assessment 4 Remote Collaboration and Evidence-Based Care References
Dang, D., Dearholt, S., Bissett, K., Ascenzi, J., & Whalen, M. (2021). Johns Hopkins Evidence-Based Practice for Nurses and healthcare professionals: Model and guidelines (4th ed.). SIGMA Theta Tau International.
Desimone, M. E., Sherwood, J., Soltman, S. C., & Moran, A. (2021). Telemedicine in cystic fibrosis. Journal of Clinical & Translational Endocrinology, 26, 100270. https://doi.org/10.1016/j.jcte.2021.100270
Vagg, T., Shanthikumar, S., Morrissy, D., Chapman, W. W., Plant, B. J., & Ranganathan, S. (2021). Telehealth and virtual health monitoring in Cystic Fibrosis. Current Opinion in Pulmonary Medicine, 27(6), 544–553. https://doi.org/10.1097/mcp.0000000000000821
Weißenfeld, M., Goetz, K., & Steinhäuser, J. (2021). Facilitators and barriers for the implementation of telemedicine from a local government point of view – a cross-sectional survey in Germany. BMC Health Services Research, 21(1), 1-9. https://doi.org/10.1186/s12913-021-06929-9
NURS-FPX4030 Assessment 4 Remote Collaboration and Evidence-Based Care Instructions
Create a 5-10 minute video of yourself, as a presenter, in which you will propose an evidence-based plan to improve the outcomes for the Vila Health patient and examine how remote collaboration provided benefits or challenges to designing and delivering the care.
Introduction
As technologies and the health care industry continue to evolve, remote care, diagnosis, and collaboration are becoming increasingly more regular methods by which nurses are expected to work. Learning the ways in which evidence-based models and care can help remote work produce better outcomes will become critical for success.
Additionally, understanding how to leverage EBP principles in collaboration will be important in the success of institutions delivering quality, safe, and cost-effective care. It could also lead to better job satisfaction for those engaging in remote collaboration.
Professional Context
Remote care and diagnosis is a continuing and increasingly important method for nurses to help deliver care to patients to promote safety and enhance health outcomes. Understanding best EBPs and building competence in delivering nursing care to remote patients is a key competency for all nurses. Additionally, in some scenarios, while you may be delivering care in person you may be collaborating with a physician or other team members who are remote. Understanding the benefits and challenges of interdisciplinary collaboration is vital to developing effective communication strategies when coordinating care. So, being proficient at communicating and working with remote health care team members is also critical to delivering quality, evidence-base care.
Scenario
The Vila Health: Remote Collaboration on Evidence-Based Care simulation provide the context for this assessment.
NURS-FPX4030 Assessment 4 Remote Collaboration and Evidence-Based Care Instructions
Before beginning this assessment, make sure you have worked through the following media:
- Vila Health: Remote Collaboration on Evidence-Based Care.
You may wish to review Selecting a model for evidence-based practice changes. [PDF] and Evidence-Based Practice Models, which help explain the various evidence-based nursing models.
For this assessment, you are a presenter! You will create a 5-10-minute video using Kaltura or similar software. In the video:
- Propose your evidence-based care plan that you believe will improve the safety and outcomes of the patient in the Vila Health Remote Collaboration on Evidence-Based Care media scenario. Add your thoughts on what more could be done for the client and what more information may have been needed.
- Discuss the ways in which an EBP model and relevant evidence helped you to develop and make decisions about the plan you proposed
- Wrap up your video by identifying the benefits of the remote collaboration in the scenario, as well as discuss strategies you found in the literature or best practices that could help mitigate or overcome one or more of the collaboration challenges you observed in the scenario.
Be sure you mention any articles, authors, and other relevant sources of evidence that helped inform your video. Discuss why these sources of evidence are credible and relevant. Important: You are required to submit an APA-formatted reference list of the sources you cited specifically in your video or used to inform your presentation. You are required to submit a narrative of all your video content to this assessment and to SafeAssign.
The following media is an example learner submission in which the speaker successfully addresses all competencies in the assessment.
- Exemplar Kaltura Reflection.
- Please note that the scenario that the speaker discusses in the exemplar is different from the Vila Health scenario you should be addressing in your video. So, the type of communication expected is being model, but the details related to the scenario in your submission will be different.
Make sure that your video addresses the following grading criteria:
- Propose your own evidence-based care plan to improve the safety and outcomes for a patient based on the Vila Health Remote Collaboration on Evidence-Care media scenario.
- Explain the ways in which you used an EBP model to help develop your plan of care for the client.
- Reflect on which evidence you found in your search that was most relevant and useful when making decisions regarding your care plan.
- Identify benefits and strategies to mitigate the challenges of interdisciplinary collaboration to plan care within the context of a remote team.
- Communicate in a professional manner that is easily audible and uses proper grammar, including a reference list formatted in current APA style.
Refer to Using Kaltura as needed to record and upload your video.
Note: If you require the use of assistive technology or alternative communication methods to participate in this activity, please contact DisabilityServices@Capella.edu to request accommodations. If, for some reason, you are unable to record a video, please contact your faculty member as soon as possible to explore options for completing the assessment.
Additional Requirements
Your assessment should meet the following requirements:
- Length of video: 5-10 minutes.
- References: Cite at least three professional or scholarly sources of evidence to support the assertions you make in your video. Include additional properly cited references as necessary to support your statements.
- APA reference page: Submit a correctly formatted APA reference page that shows all the sources you used to create and deliver your video. Be sure to format the reference page according to current APA style. Submit a narrative of all of your video content.
Portfolio Prompt: Remember to save the final assessment to your ePortfolio so that you may refer to it as you complete the final capstone course.
Competencies Measured
By successfully completing this assessment, you will demonstrate your proficiency in the following course competencies and scoring guide criteria:
- Competency 2: Analyze the relevance and potential effectiveness of evidence when making a decision.
- Reflect on which evidence you collected that was most relevant and useful when making decisions regarding the care plan.
- Competency 3: Apply an evidence-based practice model to address a practice issue.
- Explain the ways in which you used the specific evidence-based practice model to help develop the care plan identifying what interventions would be necessary. This requires a particular evidence-based model, such as the Johns Hopkins, Iowa, Stetler, or other.
- Competency 4: Plan care based on the best available evidence.
- Propose your evidence-based care plan to improve the safety and outcomes for the Vila Health patient with a discussion of new content for the care plan.
- Competency 5: Apply professional, scholarly communication strategies to lead practice changes based on evidence.
- Identify benefits and propose strategies to mitigate the challenges of interdisciplinary collaboration to plan care within the context of a remote team.
- Communicate via video with clear sound and light, and include a narrative of video content.
- Provide a full reference list that is relevant and evidence-based (published within five years), exhibiting nearly flawless adherence to APA format.
Resources: Communication
- The resources below explore communication in health care:
- Ratna, H. (2019). The importance of effective communication in healthcare practice. Harvard Public Heath Review, 23. https://harvardpublichealthreview.org/23-article-ratna/
- This article discusses the importance of communication in healthcare by presenting approaches to communication as well as discussing barriers.
- Cayley, W. (2018). Four evidence-based communication strategies to enhance patient care. https://www.aafp.org/fpm/2018/0900/p13.html
- This article presents four difference evidence-based strategies to approach patients and communicate with patients.
Resources: Evidence-Base Practice Models and Examples of Application
- The resources below explore EBP models and examples of their application:
- NewsRx. (2017, Jul 07). Nursing – evidence-based nursing; studies from University of Iowa add new findings in the area of evidence-based nursing (Iowa model of evidence-based practice: Revisions and validation). Health & Medicine Week.
- This article examines the Iowa model for EBP. The specific example in which the model is presented is oncology nursing, but there are valuable lessons to learn about applying evidence-based models to nursing practice no matter what your personal focus might be.
- Indra, V. (2018). A review on models of evidence-based practice. Asian Journal of Nursing Education and Research, 8(4), 549-552.
- In this paper, review on models of evidence-based practice is discussed.
- Cacchione, P., Jayakumar, K., Lavenberg, J., Leas, B., Mitchell, M., Mull, N., & Umscheid, C. (2019). Impact of a hospital evidence-based practice center (EPC) on nursing policy and practice. Worldviews Evid Based Nurs, 16(1), 4-11.
- This article examines evidence-based practice center work to inform nursing policy and practice.
- Chan, E., Glass, G. F., & Phang, K. N. (2020). Evaluation of a hospital-based nursing research and evidence-based practice mentorship program on improving nurses’ knowledge, attitudes, and evidence-based practice. The Journal of Continuing Education in Nursing, 51(1), 46-52.
- This article presents nine nurses in an acute hospital in Singapore that participated in a mentorship program throughout 2015. The evidence-based practice questionnaire was used to measure the program’s effectiveness. This article examines how using an evidence-based model can help in the implementation of care guidelines.
- Gawlinski, A., & Rutledge, D. (2008). Selecting a model for evidence-based practice changes. [PDF]. AACN Advanced Critical Care, 19(3) 291-300.
- This website explains the various evidence-based nursing models.
- Springer Publishing. (n.d.). Evidence-Based Practice Models. https://connect.springerpub.com/content/book/978-0-8261-2759-4/back-matter/bmatter1
- This website also explains the various evidence-based nursing models.
Resources: Technology and Telehealth Resources
- The resources below explore technology and telehealth resources:
- Peters, M. D. J. (2018). Engaging nurses and midwives with evidence-based healthcare. Australian Nursing and Midwifery Journal, 25(11), 24.
- This article discusses future national public hospital funding and healthcare reform. Australia’s healthcare sector and nursing and midwifery professional practice must be supported by the collection, sharing, linkage, analysis, implementation, and evaluation of high quality data and evidence from research as well as expert and consumer sources.
- RHIhub. (n.d.). Telehealth use in rural healthcare. https://www.ruralhealthinfo.org/topics/telehealth
- This online resource repository could be helpful in examining ways in which telehealth care is delivered, as well as how you might blend evidence-based care delivery to telehealth patients.
- van Houwelingen, C. T. M., Ettema, R. G. A., Kort, H. S. M., & ten Cate, O. (2017). Internet-generation nursing students’ view of technology-based health care. Journal of Nursing Education, 56(12), 717-724.
- This article presents the results of a study that examined the views of younger first-year nursing students with regard to a variety of technologies.
- Vila Health: Remote Collaboration on Evidence-Based Care.
- This media simulation will provide the context for your Assessment 4.
Resources: Theory and Decision Making
- The resources below explore theory and decision making:
- Barret, D. (2017). Rethinking presence: A grounded theory of nurses and teleconsultation. Journal of Clinical Nursing, 26(19/20), 157-159.
- The article presents a potential evidence-based and theory approach to delivering effective remote patient care.
- Nibbelink, C. W., Brewer, B. B. (2018). Decision-making in nursing practice: An integrative literature review. Journal of Clinical Nursing, 27(5/6), 917-928.
- This literature review examines the various ways that decision-making strategies, and the evidence that informs though strategies, are demonstrated in practice.
READ MORE >>
these nurses bridge the clinical and technological care delivery to meet effici ...
Informaticists also ensure that the team gets access to a high-quality electronic source of health information that would influence evidence-based decision-making. More importantly
READ MORE >>
Assessment 1 Instructions: Nursing Informatics in Health Care NURS-FPX4040 Examp ...
Assessment 1 Instructions: Nursing Informatics in Health Care NURS-FPX4040 Example
Nursing Informatics in Healthcare
The integration of technology in healthcare is increasingly embraced. The reasons for increased incorporation include the demonstrated benefits in improving patient outcomes, improving workflow, and reducing patient and healthcare professionals’ resistance to such innovations. The latter is attributed to the incorporation of information management and patient care technologies in nursing curricula, particularly at the baccalaureate level (Reid et al., 2021).
While the project has assisted nurses in demonstrating knowledge and skills in information management and patient care technologies, they are also expected to use the tools at the bedside or organizational levels. Having attended a meeting where a nurse informaticist conducted a presentation on her roles and impact on patient and organizational outcomes, I realized how the role would impact my organization. Drawing from evidence-based literature on the impact of a nurse informaticist on patient care, workflow, costs, and return on investment, the purpose of this paper is to create a proposal for a new nurse informaticist position.
Nursing Informatics and the Nurse Informaticist
The quest for cost-effective and high-quality patient care has resulted in greater integration of technology in healthcare. With the increased incorporation of technologies comes a new challenge: developing a unified definition of the use of technology in healthcare. Because of the lack of a consistent taxonomy, there has been consensus on definitions within healthcare informatics, with each country developing and adopting its own.
All definitions, however, are heavily influenced by the International Medical Informatics Association (IMIA), which defines nursing informatics as a science and a practice that integrates nursing, information communication technologies (ICT), and professional knowledge to promote people’s health (Honey et al., 2022). Honey et al. (2022) state definitions from Australia, the United States, and Canada to gain a common understanding of nursing informatics across diverse geographical contexts.
Nursing informatics is defined by the Australian Nursing and Midwifery Accreditation Council (ANMAC) in Australia as the knowledge and skills required by registered nurses to integrate nursing practice, computer and information science in data management, communication, and decision-making in nursing practice (Honey et al., 2022). In the United States, the American Nurse Association (ANA) Council of Computer Application in Nursing defines nursing informatics as a specialty that integrates nursing science, computer, and information science in the identification, collection, processing, and management of data to support nursing practice (Honey et al., 2022).
According to the Canadian Organization for the Advancement of Computers in Health (COACH), nursing informatics is the use of any information technology by nurses to influence patient care (Honey et al., 2022). Nursing science, ICT, professional knowledge, and the influence on patient care are consistent themes that appear in all definitions of nursing informatics.
With the global implementation of health informatics projects, the nurse informaticist’s role is expanding in various clinical settings. The need for innovative technological solutions to improve care, such as mobile applications, interactive decision aids, web-based technologies, and electronic health records (EHR), broadens the scope of nurse informaticists and gives them a more defining role. According to King et al. (2020), the primary role of a nurse informaticist is to support technological advances that improve patient care, safety, and quality.
Nurse informaticists contribute to such advancements by educating staff on new yet-to-be-implemented technologies, leading quality and process improvement initiatives, and evaluating the impact of technology on care before its implementation. Their education, certification, training, and practice experience position them more appropriately in designing and implementing technological interventions and fulfilling their other scopes of practice.
Nurse Informaticists and Other Healthcare Organizations
Healthcare organizations have had a variety of heartwarming experiences with nurse informaticists. In one case, Billings Clinic, a Magnet-designated non-profit health organization in Montana, northern Wyoming, and the western Dakotas, shares its experience with nurse informaticists. The Billings Clinic Cancer Center serves over 1800 patients annually and employs more than 70 registered nurses (RNs) in the cancer unit (Billings Clinic, 2018).
The Chief Nursing Officer (CNO) observed that the cerebellar toxicity assessment of patients receiving high-dose Cytarabine was inconsistently documented in the medical records by the nursing staff during care for patients receiving high-dose Cytarabine in the cancer unit. As a result, the CNO sought assistance from a nursing informaticist, who created a new evidence-based assessment tool. According to the CNO, the tool improved the assessment and documentation of therapy-related complications (Billings Clinic, 2018). The Billings Clinic scenario is representative of many other healthcare organizations that employ nurse informaticists.
Nurse informaticists must collaborate with other care providers to achieve the goals of a nursing informatics project. In the clinical scenario described above, for example, the nurse informaticist would collaborate with other RNs, a medical oncologist, a gynecologic oncologist, a surgical oncologist, a radiation oncologist, a pediatric oncologist, and a general surgeon. Furthermore, for the assessment and documentation tool to be successfully implemented, oncology nurse informaticists would collaborate with informaticists from other departments, including the pharmacy.
According to the CNO, the oncology nurse informaticist follows regulatory standards in designing, building, and maintaining order sets to ensure smooth operation (Billings Clinic, 2018). The CNO also reported that the system was so efficient that laboratory and vital sign monitoring, therapies, referrals, and nursing orders were all available with a single click (Billings Clinic, 2018). This would make the job of medical oncologists or any other professional who would be reviewing the patient for treatment continuation easier.
Impact of Full Nurse Engagement in Healthcare Technology
The inclusion of nurse informaticists in healthcare has implications for patient care, cost, workflow, and the privacy of patient’s health information. Sensmeier and Anderson (2020) and Williams (2019) assert that nursing informatics provides a platform for solving several patient problems. Technology is used in all processes, from patient triage upon hospital admission to discharge following recovery or any prompting factors.
For example, a computerized physician order entry (CPOE) system detects incorrect dosages, frequencies, routes, and durations of therapy in medication prescriptions (Sensmeier & Anderson, 2020; Williams, 2019). Early detection and treatment of cerebellar toxicity caused by high-dose Cytarabine therapy were critical in reducing mortality rates in the clinical scenario at Billings Clinic Cancer Center. Regarding workflow, a nurse informaticist ensures that the majority of the tasks involved in data assessment and documentation are accessible with a single click.
Management of symptoms and toxicities, laboratory and vital sign monitoring, therapies, referrals, and nursing orders are all available with a single click at Billings Clinic Cancer Center (Billings Clinic, 2018). This would improve workflow because all care providers who would need to access the patients’ information for review would be able to do so easily. A nurse informaticist will also implement measures to protect patient’s health information in accordance with the Health Insurance Portability and Accountability Act (HIPAA) privacy and confidentiality rules.
While patients’ privacy refers to the non-disclosure of their health information, confidentiality refers to the avoidance of unauthorized individuals accessing their protected health information (Bani Issa et al., 2020). Nurse informaticists assist in the implementation of patient privacy and confidentiality safeguards such as data encryption, biometrically enabled system logins and password-protected logins. In addition, nurse informaticists may assist in the installation of anti-hack software, which prevents breaches into information systems, to ensure the security of the patient’s health information (Koppel & Kuziemsky, 2019).
Concerning cost implications, recent studies on healthcare systems across the U.S. show that $760 billion to $935 billion, which represents 25% of total U.S. healthcare spending, is wasted annually (Shrank et al., 2019). Nurse informaticists and other health informatics specialists help reduce costs in various ways, one of which is the prediction of health outcomes using analytics, which aids in accurate budgeting for resources required and thus prevents overspending.
Additionally, health informatics drives process improvement initiatives in billing, human resource management, and marketing, lowering costs (Kruse & Beane, 2018). According to a website that analyzes health IT news in the U.S., the Mercy Hospital Network saved more than $4 million in one year by implementing a nursing analytics dashboard (Fox & Ang, 2018). The various examples provided justify the importance of a nurse informaticist to a healthcare organization, which would be used to decide whether or not to hire one.
Opportunities and Challenges
As the field of health informatics expands, so does the number of healthcare professionals working in it. This presents an opportunity for health and technology enthusiasts who want to collaborate with healthcare providers to improve patient outcomes. Furthermore, it has enabled the opportunity to work in close collaboration with other health stakeholders to identify patient needs that would require technology as a solution. However, while health informatics offers promising benefits in resolving patient problems, it also presents challenges.
The flaws in the equipment, techniques, observation, and data collection tools may lead to misleading conclusions (Otokiti, 2019). Further, data artifacts may give misleading impressions or result in an inability to predict trends in specifically identified health issues. Moreover, due to the high likelihood of system breaches, health informatics interventions are increasingly needed to protect patients’ security, privacy, and confidentiality.
Summary of Recommendations: Takeaways
The increased use of technology in healthcare has broadened the scope of health informatics specialists. Nurse informaticists are best suited to assist hospitals in implementing health informatics projects due to their nursing practice experience and knowledge of ICT. Their impact on improving patient care, lowering healthcare costs, improving workflow, and protecting patients’ privacy and confidentiality are critical in informing their employment in healthcare organizations.
While the opportunities for improving patient care are obvious, potential challenges exist, raising concerns about upgrading measures to protect patient privacy and confidentiality in the event of a system breach. However, as multiple evidence-based studies show, the benefits nurse informaticists bring to healthcare organizations outweigh the risks, justifying their increased importance in healthcare.
NURS-FPX4040 Assessment 1 Nursing Informatics in Health Care SOLVED References
Bani Issa, W., Al Akour, I., Ibrahim, A., Almarzouqi, A., Abbas, S., Hisham, F., & Griffiths, J. (2020). Privacy, confidentiality, security, and patient safety concerns about electronic health records. International Nursing Review, 67(2), 218–230. https://doi.org/10.1111/inr.12585
Billings Clinic. (2018). Billings Clinic: Cancer Center 2018 annual report. Billingsclinic.com. https://www.billingsclinic.com/app/files/public/8c09bf04-0e03-40b1-8ac8-b1cc520fd9f9/Cancer-Ctr-Report-3-2019.pdf
Fox, A., & Ang, A. (2018, March 26). How Mercy Hospital Network saved $4.3 million with nursing analytics dashboard. Healthcare IT News. https://www.healthcareitnews.com/news/how-mercy-hospital-network-saved-43-million-nursing-analytics-dashboard
Honey, M., Ronquillo, C., & Lee, T. T. (2022). Nurses and midwives in the digital age: Selected papers, posters and panels from the 15th International Congress in Nursing Informatics. IOS Press. https://books.google.at/books?id=0tluEAAAQBAJ
King, B. D., Riemann, L. A., & Brant, J. M. (2020). Oncology nurse informaticists: An evolving role to support nursing practice. Clinical Journal of Oncology Nursing, 24(3), 324–327. https://doi.org/10.1188/20.CJON.324-327
Koppel, R., & Kuziemsky, C. (2019). Healthcare data are remarkably vulnerable to hacking: Connected healthcare delivery increases the risks. Studies in Health Technology and Informatics, 257, 218–222. https://www.ncbi.nlm.nih.gov/pubmed/30741199
Kruse, C. S., & Beane, A. (2018). Health information technology continues to show positive effect on medical outcomes: Systematic review. Journal of Medical Internet Research, 20(2), e41. https://doi.org/10.2196/jmir.8793
Otokiti, A. (2019). Using informatics to improve healthcare quality. International Journal of Health Care Quality Assurance, 32(2), 425–430. https://doi.org/10.1108/IJHCQA-03-2018-0062
Reid, L., Maeder, A., Button, D., Breaden, K., & Brommeyer, M. (2021). Defining nursing informatics: A narrative review. Studies in Health Technology and Informatics, 284, 108–112. https://doi.org/10.3233/SHTI210680
Sensmeier, J., & Anderson, C. (2020). Tracking the impact of nursing informatics. Nursing Management, 51(9), 50–53. https://doi.org/10.1097/01.NUMA.0000694880.86685.c1
Shrank, W. H., Rogstad, T. L., & Parekh, N. (2019). Waste in the US health care system: Estimated costs and potential for savings: Estimated costs and potential for savings. JAMA: The Journal of the American Medical Association, 322(15), 1501–1509. https://doi.org/10.1001/jama.2019.1s3978
Williams, A. (2019). Nursing informaticians address Patient Safety to improve usability of Health Information technologies. Studies in Health Technology and Informatics, 257, 501–507. https://www.ncbi.nlm.nih.gov/pubmed/30741247
Also read:
NURS-FPX4040 Assessment 2 Protected Health Information PHI
NURS-FPX4040 Assessment 3 Evidence-Based Proposal and Annotated Bibliography on Technology in Nursing
NURS-FPX4040 Assessment 4 Informatics and Nursing Sensitive Quality Indicators
NURS-FPX4040 Assessment 1 Nursing Informatics in Health Care SOLVED Instructions
- Write a 4-5 page evidence-based proposal to support the need for a nurse informaticist in an organization who would focus on improving health care outcomes.
Introduction
As you begin to prepare this assessment, you are encouraged to complete the Team Perspectives of the Nurse Informaticist activity. Completion of this will help you succeed with the assessment as you explore the nurse informaticist’s role from the different perspectives of the health care team. Completing activities is also a way to demonstrate engagement.
Nurses at the baccalaureate level in all practice areas are involved in nursing informatics through interaction with information management and patient care technologies. Nurses must not only demonstrate knowledge of and skills in health information and patient care technologies, but also how to use these tools at the bedside and organizational levels. Moreover, nurses need to recognize how information gathered from various health information sources can impact decision making at the national and state regulatory levels.
Scenario
For this assessment, assume you are a nurse attending a meeting of your state’s nurses association. A nurse informaticist conducted a presentation on her role and its impact on positive patient and organizational outcomes in her workplace. You realize that your organization is undergoing many technological changes. You believe this type of role could provide many benefits to your organization.
You decide to pursue proposing a nurse informaticist role in your organization. You speak to your chief nursing officer (CNO) and human resources (HR) manager, who ask you to prepare a 4–5 page evidence-based proposal to support the new role. In this way, they can make an informed decision as to whether the addition of such a role could justify the return on investment (ROI). They need your proposal before an upcoming fiscal meeting.
This is not an essay, but instead, it is a proposal to create a new Nurse Informaticist position.
One important part of this assessment is the justification of the need for a nurse informaticist in a health care organization and references from relevant and timely scholarly or professional resources to support the justification for creating this nurse informaticist position. The term justify means to show or prove that the nurse informaticist position brings value to the organization. This justification must include evidence from the literature to support that this position will provide a return on investment for the organization.
Preparation for NURS-FPX4040 Assessment 1 Nursing Informatics in Health Care SOLVED
To successfully prepare for this assessment, you will need to complete these preparatory activities:
- Review assessment resources and activities.
- Conduct independent research on the nursing knowledge and skills necessary to interact with health information and patient care technology.
- Focus your research on current resources available through peer-reviewed articles, professional websites, government websites, professional blogs, wikis, job boards, and so on.
- Consult the BSN Program Library Research Guide for help in identifying scholarly and authoritative sources.
- Interview peers in your network who are considered information technology experts.
- Ask them about how information technology advances are impacting patient care at the bedside, at the organizational level, and beyond.
Proposal Format
The chief nursing officer (CNO) and human resources (HR) manager have asked you to include the following headings in your proposal and to be sure to address the bullets following each heading:
Nursing Informatics and the Nurse Informaticist
- What is nursing informatics?
- What is the role of the nurse informaticist?
Nurse Informaticists and Other Health Care Organizations
- What is the experience of other health care organizations with nurse informaticists?
- How do these nurse informaticists interact with the rest of the nursing staff and the interdisciplinary team?
Impact of Full Nurse Engagement in Health Care Technology
- How does fully engaging nurses in health care technology impact:
- Patient care?
- Protected health information (security, privacy, and confidentiality)?
- In this section, you will explain evidence-based strategies that the nurse informaticist and interdisciplinary team can use to effectively manage patients’ protected health information, particularly privacy, security, and confidentiality. Evidence-based means that they are supported by evidence from scholarly sources.
- Workflow?
- Costs and return on investment?
Opportunities and Challenges
- What are the opportunities and challenges for nurses and the interdisciplinary team with the addition of a nurse informaticist role?
- How can the interdisciplinary team collaborate to improve quality care outcomes through technology?
Summary of Recommendations
- What are 3–4 key takeaways from your proposal about the recommended nurse informaticist role that you want the CNO and the HR manager to remember?
- This is the section where the justification for the implementation of the nursing informaticist role is addressed. Remember to include evidence from the literature to support your recommendation.
Additional Requirements for NURS-FPX4040 Assessment 1 Nursing Informatics in Health Care SOLVED
- Written communication: Ensure written communication is free of errors that detract from the overall message.
- Submission length: 4–5 double-spaced pages, in addition to title and references pages.
- Font: Times New Roman, 12 point.
- Citations and References: Cite a minimum of three current scholarly and/or authoritative sources to support your ideas. In addition, cite a minimum of one current professional blog or website to support your central ideas. Current means no more than five years old.
- APA formatting: Be sure to follow APA formatting and style guidelines for citations and references. For an APA refresher, consult the Evidence and APA page on Campus.
Competencies Measured in NURS-FPX4040 Assessment 1 Nursing Informatics in Health Care SOLVED
By successfully completing this assessment, you will demonstrate your proficiency in the following course competencies and scoring guide criteria:
- Competency 1: Describe nurses’ and the interdisciplinary team’s role in informatics with a focus on electronic health information and patient care technology to support decision making.
- Define nursing informatics and the role of the nurse informaticist.
- Explain how the nurse collaborates with the interdisciplinary team, including technologists, to improve the quality of patient care.
- Justify the need for a nurse informaticist in a health care organization.
- Competency 2: Implement evidence-based strategies to effectively manage protected health information.
- Explain evidence-based strategies that the nurse and interdisciplinary team can use to effectively manage patients’ protected health information (privacy, security, and confidentiality).
- Competency 5: Apply professional, scholarly communication to facilitate use of health information and patient care technologies.
- Follow APA style and formatting guidelines for citations and references.
- Create a clear, well-organized, and professional proposal that is generally free from errors in grammar, punctuation, and spelling.
Nursing Informatics in Health Care Scoring Guide
CriteriaNon-performanceBasicProficientDistinguishedDefine nursing informatics and the role of the nurse informaticist.Does not define nursing informatics and the role of the nurse informaticist.Defines nursing informatics and the role of the nurse informaticist, but the description lacks detail or is missing important information.Defines nursing informatics and the role of the nurse informaticist.Defines nursing informatics and the role of the nurse informaticist. References current data, evidence, or standards to support and refine definition.Explain how the nurse informaticist collaborates with the interdisciplinary team, including technologists, to improve the quality of patient care.Does not explain how the nurse informaticist collaborates with the interdisciplinary team, including technologists, to improve the quality of patient care.Identifies but does not explain how the nurse informaticist collaborates with the interdisciplinary team, including technologists, to improve the quality of patient care.Explains how the nurse informaticist collaborates with the interdisciplinary team, including technologists, to improve the quality of patient care.Explains how the nurse informaticist collaborates with the interdisciplinary team, including technologists, to improve the quality of patient care. Makes explicit reference to scholarly or professional resources to support explanation.Justify the need for a nurse informaticist in a health care organization.Does not justify the need for a nurse informaticist in a health care organization.Proposes but does not justify the need for a nurse informaticist in a health care organization.Justifies the need for a nurse informaticist in a health care organization.Justifies the need for a nurse informaticist in a health care organization and references relevant and timely scholarly or professional resources to support the justification.Explain evidence-based strategies that the nurse informaticist and interdisciplinary team can use to effectively manage patients’ protected health information (privacy, security, and confidentiality).Does not explain evidence-based strategies that the nurse informaticist and interdisciplinary team can use to effectively manage patients’ protected health information (privacy, security, and confidentiality).Describes but does not explain evidence-based strategies that the nurse informaticist and interdisciplinary team can use to effectively manage patients’ protected health information (privacy, security, and confidentiality).Explains evidence-based strategies that the nurse informaticist and interdisciplinary team can use to effectively manage patients’ protected health information (privacy, security, and confidentiality).Explains evidence-based strategies that the nurse informaticist and interdisciplinary team can use to effectively manage patients’ protected health information (privacy, security, and confidentiality), with reference to specific data, evidence, or standards to support the explanation.Follow APA style and formatting guidelines for citations and references.Does not follow APA style and formatting guidelines for citations and references.Partially follows APA style and formatting guidelines for citations and references.Follows APA style and formatting guidelines for citations and references.Follows APA style and formatting guidelines for citations and references with flawless precision and accuracy.Create a clear, well-organized, and professional proposal that is generally free from errors in grammar, punctuation, and spelling.Does not create a clear, well-organized, and professional proposal that is generally free from errors in grammar, punctuation, and spelling.Creates a proposal that lacks clarity and/or has errors in grammar, punctuation, and spelling.Creates a clear, well-organized, and professional proposal that is generally free from errors in grammar, punctuation, and spelling.Creates a clear, comprehensive, well-organized, and professional proposal that is error-free in grammar, punctuation, and spelling.NURS-FPX4040 Assessment 1 Nursing Informatics in Health Care SOLVED Example 2
McGonigle and Mastrian (2021) defined nursing informatics as the nursing subspecialty that enables nurses to master data, information, know-how, and wisdom through subspecialties that combine nursing science with information and computer science (p.56). Information technology has changed nursing care and transformed healthcare practice by assisting care delivery, supplementing decision-making, and predicting future trends in care using data. The used potential of technology to improve patient safety and quality of care is enormous (Schoenbaum & Carroll, 2020).
However, technology keeps advancing and better methods are incorporated into practice. However, these technologies still require human interaction and human input to influence patient care. This proposal describes the role of a nurse informaticist, especially in an interdisciplinary team, explains the impact of full nurse engagement in technology, and finally suggests opportunities and predicts challenges that including a nurse informaticist in an interdisciplinary team creates.
Nursing Informatics and the Nurse Informaticist
Recent developments in healthcare, including the COVID-19 pandemic, opened our eyes to the need to harness the potential of technology in making healthcare efficient and meeting the needs of many patients remotely. Before this, the National League for Nursing, through their new vision, had urged nursing education programs to teach and prepare them for practice in the era of healthcare technologies (McBride & Tietze, 2022). However, the workload from clinician care needs and care efficiency needs can overwhelm the individual nurses, thus the need for interdisciplinary collaboration.
Nurse informaticists are specialists trained with scientific and artistic knowledge and skills in utilizing data science to influence care through communication, decision-making, and daily monitoring workflow in healthcare systems. Their role is crucial in an interdisciplinary team approach to care because they enable the interdisciplinary teams to work efficiently. Nurse informaticists can influence policymaking and implementation, technical capacity, and patient outcomes.
Nurse informaticists have played an important role in the selection and implementation of appropriate technologies to meet patient care needs in various hospitals. Enhancing technology usability by matching user needs and vendor software features is another way nurse informaticists have ensured that organizations get worth for their expenditures on technologies and that patients have received safe care by using appropriate, safe, and high-yield technologies.
Nurse Informaticists and Other Health Care Organizations
Various institutions have implemented the informaticist role in the clinical and administrative care hierarchies. Nurse informaticists support other nurses, healthcare professionals, patients, and other stakeholders by enabling information structures, information processes, and information technologies.
According to (McBride & Tietze, 2022), nurse informaticists have improved patient safety and reduced care-associated costs (P.10). The achievements of these outcomes have been possible through safe medication administration systems using technology, predicting patient care changes through the prediction of patterns of previous outcomes, and easy documentation, retrieval and access of patient records.
Nursing Education for the Healthcare Informatics (NEHI) developed a mo
READ MORE >>
whether they come into contact with the information directly or indirectly. Sin ...
READ MORE >>
NURS-FPX4040 Assessment 2 Protected Health Information PHI ExampleProtected Heal ...
NURS-FPX4040 Assessment 2 Protected Health Information PHI Example
Protected Health Information (PHI): Privacy, Security, and Confidentiality Best Practices
Protected health information PHI is the personal information collected by healthcare professionals for the aim of patient identification. Protected health information includes demographic information, the medical history of a patient, their tests and laboratory results, the patient’s health conditions, and the patient’s insurance information. The HIPAA requires healthcare institutions to maintain safeguards that ensure confidentiality, privacy, integrity, and unavailability of protected health information to unauthorized persons.
The act also lays out guidelines for running health apps that potentially use, store, or transmit protected health information. HIPAA does not necessarily cover data collected by these apps. However, the healthcare institution applying the app is required to have a HIPAA compliance officer evaluating the app before implementation to ensure that it safeguards patients’ privacy, security, and confidentiality (HIPAA Journal, 2022).
Privacy, security, and confidentiality
Protection of the patient’s privacy and treating their information with confidentiality protects them from security issues that would develop when unauthorized persons access their information. Patient privacy is the protection of the information that the institution collects about the individual. It is the right one to determine for themselves when and how personal information can be accessed or shared.
Confidentiality is the protection of sharing information with unauthorized persons. Security is the level at which personal information is restricted and allowed for those authorized only. According to Keshta and Odeh (2021), concerns about patient privacy, security, and confidentiality include failing to safeguard various information directly affecting patients’ families. Also, accessing personal patient information would expose the patients to security risks such as being conned.
Importance of the interdisciplinary collaboration in safeguarding sensitive electronic health information
The interdisciplinary team has the role of safeguarding electronic health information, whether they come into contact with the information directly or indirectly. Since the consequences of breaching the protection of electronic health information may affect the entire healthcare institution, each interdisciplinary team member needs to maintain privacy, security, and confidentiality safeguards. It is the role of the interdisciplinary team to promote patient safety. One way to promote patient safety is by safeguarding patient privacy and confidentiality and ensuring patient security. Effective safeguarding of sensitive electronic patient information requires the collaboration of the interdisciplinary team (Keshta & Odeh, 2021).
Evidence relating to social media usage and PHI
The issue of electronic health information and the protection of protected health information should be taken seriously by all interprofessional team members. It is worth noting that the US government takes inappropriate social media use by the healthcare team very seriously. It has legal complications ranging from license termination, individual fines, and even fines to the healthcare organization. When caught in social media misconduct, healthcare institutions also set consequences for the interdisciplinary team. A healthcare professional may be suspended from working in the institution or initiate legal action. The misconduct may also cause the institution to attract financial penalties or even affect its licensure.
Our institution’s evidence-based strategies to prevent and reduce confidentiality, privacy, and security breaches, especially related to social media use, include staff training, disciplinary action taken against the staff found breaching and taking legal action (Zhou et al., 2018). The institution has annual social media and information technology training for all staff members, whereby the staff is reminded of the safety issues of social media use. There are also set steps to report social media misconduct and breaches, and all the staff members are aware of the consequences.
Professional Staff Update
Every member of staff should be careful when using social media so that we can maintain patient safety. We need to safeguard the patient’s privacy, confidentiality, and security to achieve desired patient outcomes and make our work safe.
Social Media Best Practices
- Healthcare professionals should have a clear distinction between social media and work.
- Care providers should not post content that may bring privacy and security concerns to the patient.
- Care providers should not post patients’ personal information on social media platforms, especially personal identification information.
- Doctors and nurses should not post any diagnostic or medical history on social media without the patient’s consent.
- Avoid sharing any sensitive patient information on social media platforms.
- Social media misconduct should be reported to the disciplinary of the institution or the relevant authority.
Social Media Risks to Patient Information
The profound use of social media in healthcare poses a significant risk to sensitive patient information (Terrase et al., 2019). Patient information that hackers access may have detrimental effects on the patient’s safety and security. Personal information can be used to contact the patient and the patient’s family in the name of the healthcare institution.
Some hackers can also use patient information to illegally access insurance reimbursements that cater to the patient’s treatment expenses. Also, healthcare professionals’ accounts can be hacked, and patient information can be shared by malicious hackers, thus attracting legal implications to the owner of the hacked accounts. Therefore, it is integral for all healthcare staff in the interdisciplinary team to maintain good social media use and avoid as much as sharing patient information on their accounts.
NURS-FPX4040 Assessment 2 Protected Health Information PHI References
Keshta, I., & Odeh, A. (2021). Security and privacy of electronic health records: Concerns and challenges. Egyptian Informatics Journal, 22(2), 177-183. https://doi.org/10.1016/j.eij.2020.07.003
Terrasse, M., Gorin, M., & Sisti, D. (2019). Social media, e?health, and medical ethics. Hastings Center Report, 49(1), 24-33. https://doi.org/10.1002/hast.975
What is Protected Health Information? January 2, 2022. HIPAA Journal. Accessed on July 11, 2022. https://www.hipaajournal.com/what-is-protected-health-information/
Zhou, L., Zhang, D., Yang, C. C., & Wang, Y. (2018). Harnessing social media for health information management. Electronic Commerce Research and Applications, 27, 139–151. https://doi.org/10.1016/j.elerap.2017.12.003
NURS-FPX4040 Assessment 2 Protected Health Information PHI Instructions: Privacy, Security, and Confidentiality Best Practices
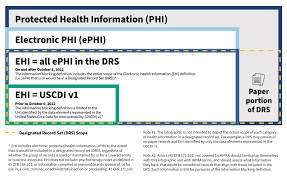
In this assessment, assume you are a nurse in an acute care, community, school, nursing home, or other health care setting. Before your shift begins, you scroll through Facebook and notice that a coworker has posted a photo of herself and a patient on Facebook.
The post states, ”I am so happy Jane is feeling better. She is just the best patient I’ve ever had, and I am excited that she is on the road to recovery.”
You have recently completed your annual continuing education requirements at work and realize this is a breach of your organization’s social media policy. Your organization requires employees to immediately report such breaches to the privacy officer to ensure the post is removed immediately and that the nurse responsible receives appropriate corrective action.
You follow appropriate organizational protocols and report the breach to the privacy officer. The privacy officer takes swift action to remove the post. Due to the severity of the breach, the organization terminates the nurse.
Based on this incident’s severity, your organization has established a task force with two main goals:
Educate staff on HIPAA and appropriate social media use in health care.
Prevent confidentiality, security, and privacy breaches.
The task force has been charged with creating a series of interprofessional staff updates on the following topics:
- Social media best practices.
- What not to do: Social media.
- Social media risks to patient information.
- Steps to take if a breach occurs.
You are asked to select one or more of the topics and create the content for a staff update containing a maximum of two content pages. This assessment is not a traditional essay. It is a staff educational update about PHI.
Consider creating a flyer, pamphlet, or PowerPoint slide. Remember it should not be more than two pages (excluding a title and a reference page).
The task force has asked team members assigned to the topics to include the following content in their updates in addition to content on their selected topics:
- What is protected health information (PHI)?
- Be sure to include essential HIPAA information.
- What are privacy, security, and confidentiality?
- Define and provide examples of privacy, security, and confidentiality concerns related to the use of technology in health care.
- Explain the importance of interdisciplinary collaboration to safeguard sensitive electronic health information.
What evidence relating to social media usage and PHI do interprofessional team members need to be aware of? For example:
- How many nurses have been terminated for inappropriate social media use in the United States?
- What types of sanctions have health care organizations imposed on interdisciplinary team members who have violated social media policies?
- What have been the financial penalties assessed against health care organizations for inappropriate social media use?
- What evidence-based strategies have health care organizations employed to prevent or reduce confidentiality, privacy, and security breaches, particularly related to social media usage?
Notes
Your staff update is limited to two double-spaced content pages. Be selective about the content you choose to include in your update so you can meet the page length requirement. Include need-to-know information. Omit nice-to-know information.
Many times people do not read staff updates, do not read them carefully, or do not read them to the end. Ensure your staff update piques staff members’ interest, highlights key points, and is easy to read. Avoid overcrowding the update with too much content.
Also, supply a separate reference page that includes two or three peer-reviewed and one or two non-peer-reviewed resources (for a total of 3-5 resources) to support the staff update content.
Additional Requirements for NURS-FPX4040 Assessment 2 Protected Health Information PHI
- Written communication: Ensure the staff update is free from errors that detract from the overall message.
- Submission length: Maximum of two double-spaced content pages.
- Font and font size: Use Times New Roman, 12-point.
- Citations and references: Provide a separate reference page that includes 2–3 current, peer-reviewed and 1–2 current, non-peer-reviewed in-text citations and references (total of 3–5 resources) that support the staff update’s content. Current mean no older than 5 years.
- APA format: Be sure your citations and references adhere to APA format. Consult the APA Style and Format page for an APA refresher.
NURS-FPX4040 Assessment 2 Protected Health Information PHI Example 2
Electronic health records (EHRs) provide an e-version of protected health information, including patients’ demographics, progress notes, vital signs, past medical history, immunizations, and lab reports (CMS, 2021). In this sense, EHRs enable healthcare professionals to manage data by automating access to patients’ information.
Despite these benefits, handling data in electronic health records increases the likelihood of cyber security threats, including ransomware, hacking, unauthorized access, and phishing.
Therefore, this assessment elaborates on best practices for safeguarding patient data, laws related to protecting sensitive electronic health information, the importance of interdisciplinary approaches, and the essence of educating nurses about social media usage.
Laws Related to Protecting Sensitive Electronic Health Information
The Health Insurance Portability and Accountability Act (HIPAA) of 1996 remains the most profound policy for institutionalizing strategies for safeguarding data privacy, security, and confidentiality. The law emphasizes providing consent to patients when sharing their identifiable information with other healthcare professionals or between health organizations.
According to the Centers for Disease Control and Prevention (CDC, 2018), HIPAA covers various entities, including healthcare providers, health plans, healthcare clearinghouses, and business associates.
In this sense, these entities must adhere to set provisions, including ensuring confidentiality, integrity, and availability of all electronically protected health information, detecting and safeguarding information against anticipated threats, and protecting data against anticipated, impermissible uses or disclosures. At the minimum, healthcare organizations must ensure that patients know data disclosure and privacy guidelines.
Importance of Interdisciplinary Collaboration in Protecting Sensitive Electronic Health Information
The Health Insurance Portability and Accountability Act (HIPAA) requires healthcare professionals and organizations to comply with data privacy, security, and confidentiality protocols.
However, healthcare professionals face a daunting endeavor to adhere to these guidelines when interdisciplinary collaboration is lacking. Holden et al. (2018) contend that interprofessional team performance is a fundamental approach that allows caregivers to consolidate diverse expertise to solve complex challenges in holistic and comprehensive ways.
In this sense, nurses should collaborate with physicians, organizational management, nurse informaticists, patients, and IT experts to develop collective safeguards for patient information.
Evidence-based Approaches to Mitigate Information Risks
Health organizations can safeguard data privacy, security, and confidentiality by implementing three safeguards: physical, administrative, and technical safeguards. According to Kruse et al. (2017), physical strategies (safeguards) for ensuring data security, privacy, and confidentiality include installing radio frequency identification devices (RFIDs), promoting workstation security, physical access controls, and assigning security responsibilities.
On the other hand, administrative strategies include risk analysis and management, system security evaluation, staff education, and hiring chief information security officers (Kruse et al., 2017, p. 127). Finally, technical security approaches encompass entity authentication, system audits, data/documents encryption, virus checking, and access control to ensure data confidentiality. Undoubtedly, the success of these interventions depends massively upon interdisciplinary collaboration and leadership commitment.
Educating Nurses about Social Media Use
Nurses are susceptible to inadvertently violating or exposing protected health information to threats as they interact on various social media platforms. Often, posting online blogs sharing pictures, audio, and videos may accidentally reveal patients’ vital information. Therefore, it is essential to educate nurses on the tenets of e-professionalism. According to Isik and Jalland (2019), e-professionalism defines social media’s legal and ethical implications.
While e-professionalism is relatively a new paradigm of safeguarding patient data, it guarantees patient satisfaction and enables nurses to provide professional content on social media platforms. Also, educating nurses about proper social media usage enlightens them about the legal and ethical implications of violating data privacy policies. As a result, it emerges as a profound administrative safeguard for ensuring data privacy, security, and confidentiality.
Conclusion
Although electronic health records automate data and promote clinical practices, they expose patients’ sensitive data to multiple threats, including phishing, hacking, and unauthorized disclosures. As a result, it is essential to emphasize interdisciplinary collaboration to implement physical, technical, and administrative safeguards.
In the same breath, educating nurses regarding e-professionalism prevents the likelihood of inadvertently violating data privacy, security, and confidentiality. Also, staff education enlightens them on the potential legal and ethical ramifications of exposing protected health information to potential cyber security threats.
NURS-FPX4040 Assessment 2 Protected Health Information PHI References
- Centers for Disease Control and Prevention. (2018, September 14). Health Insurance Portability and accountability act of 1996 (HIPAA). Retrieved from https://www.cdc.gov/phlp/publications/topic/hipaa.html
- Centers for Medicare and Medicaid Services. (2021, January 12). Electronic Health Records. Retrieved from https://www.cms.gov/Medicare/E-Health/EHealthRecords
- Holden, R., Binkheder, S., Patel, J., & Viernes, S. (2018). Best practices for health informatician involvement in interprofessional health care teams. Applied Clinical Informatics, 09(01), 141-148. https://doi.org/10.1055/s-0038-1626724
- Isik, B., & Jallad, S. (2019). The potential of social media and nursing education: E-professionalism, nurse educator–learner role, benefits, and risks. New Trends and Issues Proceedings on Advances in Pure and Applied Sciences, (11), 30-38. https://doi.org/10.18844/gjpaas.v0i11.4310
- Kruse, C., Smith, B., Vanderlinden, H., & Nealand, A. (2017). Security techniques for electronic health records. Journal of Medical Systems, 41(8), 1-9. https://doi.org/10.1007/s10916-017-0778-4
NURS-FPX4040 Assessment 2 Protected Health Information PHI Instructions: Protected Health Information (PHI): Privacy, Security, and Confidentiality Best Practices
Prepare a 2-page interprofessional staff update on HIPAA and appropriate social media use in health care.
Introduction
As you begin to consider the assessment, it would be an excellent choice to complete the Breach of Protected Health Information (PHI) activity. The activity will support your success with the assessment by creating the opportunity for you to test your knowledge of potential privacy, security, and confidentiality violations of protected health information. The activity is not graded and counts towards course engagement.
Health professionals today are increasingly accountable for the use of protected health information (PHI). Various government and regulatory agencies promote and support privacy and security through a variety of activities. Examples include:
- Meaningful use of electronic health records (EHR).
- Provision of EHR incentive programs through Medicare and Medicaid.
- Enforcement of the Health Insurance Portability and Accountability Act (HIPAA) rules.
- Release of educational resources and tools to help providers and hospitals address privacy, security, and confidentiality risks in their practices.
Technological advances, such as the use of social media platforms and applications for patient progress tracking and communication, have provided more access to health information and improved communication between care providers and patients.
At the same time, advances such as these have resulted in more risk for protecting PHI. Nurses typically receive annual training on protecting patient information in their everyday practice. This training usually emphasizes privacy, security, and confidentiality best practices such as:
- Keeping passwords secure.
- Logging out of public computers.
- Sharing patient information only with those directly providing care or who have been granted permission to receive this information.
Today, one of the major risks associated with privacy and confidentiality of patient identity and data relates to social media. Many nurses and other health care providers place themselves at risk when they use social media or other electronic communication systems inappropriately. For example, a Texas nurse was recently terminated for posting patient vaccination information on Facebook. In another case, a New York nurse was terminated for posting an insensitive emergency department photo on her Instagram account.
Health care providers today must develop their skills in mitigating risks to their patients and themselves related to patient information. At the same time, they need to be able distinguish between effective and ineffective uses of social media in health care.
This assessment will require you to develop a staff update for the interprofessional team to encourage team members to protect the privacy, confidentiality, and security of patient information.
Preparation
To successfully prepare to complete this assessment, complete the following:
- Review the infographics on protecting PHI provided in the resources for this assessment, or find other infographics to review. These infographics serve as examples of how to succinctly summarize evidence-based information.
- Analyze these infographics and distill them into five or six principles of what makes them effective. As you design your interprofessional staff update, apply these principles. Note: In a staff update, you will not have all the images and graphics that an infographic might contain. Instead, focus your analysis on what makes the messaging effective.
- Select from any of the following options, or a combination of options, the focus of your interprofessional staff update:
- Social media best practices.
- What not to do: social media.
- Social media risks to patient information.
- Steps to take if a breach occurs.
- Conduct independent research on the topic you have selected in addition to reviewing the suggested resources for this assessment. This information will serve as the source(s) of the information contained in your interprofessional staff update. Consult the BSN Program Library Research Guide for help in identifying scholarly and/or authoritative sources.
Instructions
In this assessment, assume you are a nurse in an acute care, community, school, nursing home, or other health care setting. Before your shift begins, you scroll through Facebook and notice that a coworker has posted a photo of herself and a patient on Facebook. The post states, “I am so happy Jane is feeling better. She is just the best patient I’ve ever had, and I am excited that she is on the road to recovery.”
You have recently completed your annual continuing education requirements at work and realize this is a breach of your organization’s social media policy. Your organization requires employees to immediately report such breaches to the privacy officer to ensure the post is removed immediately and that the nurse responsible receives appropriate corrective action.
You follow appropriate organizational protocols and report the breach to the privacy officer. The privacy officer takes swift action to remove the post. Due to the severity of the breach, the organization terminates the nurse.
Based on this incident’s severity, your organization has established a task force with two main goals:
- Educate staff on HIPAA and appropriate social media use in health care.
- Prevent confidentiality, security, and privacy breaches.
The task force has been charged with creating a series of interprofessional staff updates on the following topics:
- Social media best practices.
- What not to do: Social media.
- Social media risks to patient information.
- Steps to take if a breach occurs.
You are asked to select one or more of the topics and create the content for a staff update containing a maximum of two content pages. This assessment is not a traditional essay. It is a staff educational update about PHI. Consider creating a flyer, pamphlet, or one PowerPoint slide (not an entire presentation). Remember it should not be more than two pages (excluding a title and a reference page).
The task force has asked team members assigned to the topics to include the following content in their updates in addition to content on their selected topics:
- What is protected health information (PHI)?
- Be sure to include essential HIPAA information.
- What are privacy, security, and confidentiality?
- Define and provide examples of privacy, security, and confidentiality concerns related to the use of technology in health care.
- Explain the importance of interdisciplinary collaboration to safeguard sensitive electronic health information.
- What evidence relating to social media usage and PHI do interprofessional team members need to be aware of? For example:
- How many nurses have been terminated for inappropriate social media use in the United States?
- What types of sanctions have health care organizations imposed on interdisciplinary team members who have violated social media policies?
- What have been the financial penalties assessed against health care organizations for inappropriate social media use?
- What evidence-based strategies have health care organizations employed to prevent or reduce confidentiality, privacy, and security breaches, particularly related to social media usage?
Notes
- Your staff update is limited to two double-spaced content pages. Be selective about the content you choose to include in your update so you can meet the page length requirement. Include need-to-know information. Omit nice-to-know information.
- Many times people do not read staff updates, do not read them carefully, or do not read them to the end. Ensure your staff update piques staff members’ interest, highlights key points, and is easy to read. Avoid overcrowding the update with too much content.
- Also, supply a separate reference page that includes two or three peer-reviewed and one or two non-peer-reviewed resources (for a total of 3–5 resources) to support the staff update content.
Additional Requirements
- Written communication: Ensure the staff update is free from errors that detract from the overall message.
- Submission length: Maximum of two double-spaced content pages.
- Font and font size: Use Times New Roman, 12-point.
- Citations and references: Provide a separate reference page that includes 2–3 current, peer-reviewed and 1–2 current, non-peer-reviewed in-text citations and references (total of 3–5 resources) that support the staff update’s content. Current means no older than 5 years.
- APA format: Be sure your citations and references adhere to APA format. Consult the Evidence and APA page for an APA refresher.
Competencies Measured
By successfully completing this assessment, you will demonstrate your proficiency in the following course competencies and scoring guide criteria:
- Competency 1: Describe nurses’ and the interdisciplinary team’s role in informatics with a focus on electronic health information and patient care technology to support decision making.
- Describe the security, privacy, and confidentially laws related to protecting sensitive electronic health information that govern the interdisciplinary team.
- Explain the importance of interdisciplinary collaboration to safeguard sensitive electronic health information.
- Competency 2: Implement evidence-based strategies to effectively manage protected health information.
- Identify evidence-based approaches to mitigate risks to patients and health care staff related to sensitive electronic health information.
- Develop a professional, effective staff update that educates interprofessional team members about protecting the security, privacy, and confidentiality of patient data, particularly as it pertains to social media usage.
- Competency 5: Apply professional, scholarly communication to facilitate use of health information and patient care technologies.
- Follow APA style and formatting guidelines for citations and references.
- Create a clear, concise, well-organized, and professional staff update that is generally free from errors in grammar, punctuation, and spelling.
NURS-FPX4040 Assessment 2 Protected Health Information PHI: Privacy, Security, and Confidentiality Best Practices Example 3
Protected health information PHI is the personal information collected by healthcare professionals for the aim of patient identification. Protected health information includes demographic information, the medical history of a patient, their tests and laboratory results, the patient’s health conditions, and the patient’s insurance information.
The HIPAA requires healthcare institutions to maintain safeguards that ensure confidentiality, privacy, integrity, and unavailability of protected health information to unauthorized persons. The act also lays out guidelines for running health apps that potentially use, store, or transmit protected health information. HIPAA does not necessarily cover data collected by these apps. However, the healthcare institution applying the app is required to have a HIPAA compliance officer evaluating the app before implementation to ensure that it safeguards patients’ privacy, security, and confidentiality (HIPAA journal, 2022).
Privacy, security, and confidentiality
Protection of the patient’s privacy and treating their information with confidentiality protects them from security issues that would develop when unauthorized persons access their information. Patient privacy is the protection of the information that the institution collects about the individual. It is the right one to determine for themselves when and how personal information can be accessed or shared.
Confidentiality is the protection of sharing information with unauth
READ MORE >>
