Our Previous Samples
NURS 6512 Week 7 Focused Exam Chest Pain Brian Foster ResultsNURS 6512 Week 7 Fo ...
NURS 6512 Week 7 Focused Exam Chest Pain Brian Foster Results
NURS 6512 Week 7 Focused Exam: Chest Pain Brian Foster Results
Experience Overview
Patient: Brian Foster
Digital Clinical Experience Score
99.1%
This score measures your performance on the Student Performance Index in relation to other students in comparable academic programs. Your instructor has chosen to scale your Student Performance Index score so that the average score on the index is 80.0%. This score may not be your final grade if your instructor chooses to include additional components, such as documentation or time spent.
CLICK HERE TO ORDER SHADOW HEALTH ASSESSMENTS
Student Performance Index
67out of
69Proficiency Level:
Proficient- Beginning
- Developing
- Proficient
Subjective Data Collection
30out of
30Objective Data Collection
31out of
33Education and Empathy
6out of
6Time
602 minutes total spent in assignmentInteraction with patient
602 minutes
Transcript
Started: Oct 05, 2020 | Total Time: 602 minAll Lines (349)Interview Questions (133)Statements (42)Exam Actions (174) Hi Mr Foster, My name is , I am going to examine you today.
Hi Mr Foster, My name is , I am going to examine you today.Greet
10/05/20 1:18 PM MDT
 Good morning.
Good morning.  What brought you here today ?
What brought you here today ?Question
10/05/20 1:18 PM MDT
 I have been having some troubling chest pain in my chest now and then for the past month.
I have been having some troubling chest pain in my chest now and then for the past month.  Oh I’m sorry to hear that, it should be very uncomfortable to have that pain for a whole month.
Oh I’m sorry to hear that, it should be very uncomfortable to have that pain for a whole month.Empathize
10/05/20 1:22 PM MDT
 Thanks. I appreciate that.
Thanks. I appreciate that.  ? (No matching questions found.)
? (No matching questions found.)Question
10/05/20 1:22 PM MDT
 What is the onset of your pain ?
What is the onset of your pain ?Question
10/05/20 1:23 PM MDT
 I first noticed it earlier this month. I thought it might just be heartburn and it passed after about a couple of minutes.
I first noticed it earlier this month. I thought it might just be heartburn and it passed after about a couple of minutes.  What is the exact location of the pain ?
What is the exact location of the pain ?Question
10/05/20 1:24 PM MDT
 When the pain happens, I feel it mostly in the middle of my chest, over my heart.
When the pain happens, I feel it mostly in the middle of my chest, over my heart.  When did you chest pain start ?
When did you chest pain start ?Question
10/05/20 1:25 PM MDT
 I first noticed it earlier this month. I thought it might just be heartburn and it passed after a couple of minutes.
I first noticed it earlier this month. I thought it might just be heartburn and it passed after a couple of minutes.  What is the exact location of the pain ?
What is the exact location of the pain ?Question
10/05/20 1:25 PM MDT
 When the pain happens, I feel it mostly in the middle of my chest, over my heart.
When the pain happens, I feel it mostly in the middle of my chest, over my heart.  Sorry to hear that
Sorry to hear thatEmpathize
10/05/20 1:26 PM MDT
 Thanks. I appreciate that.
Thanks. I appreciate that.  Easter pain radiates anywhere ? (Clarified to Is your pain radiating?.)
Easter pain radiates anywhere ? (Clarified to Is your pain radiating?.)Question
10/05/20 1:26 PM MDT
 The pain doesn’t radiate anywhere. It’s mostly just right in the middle of my chest. (Clarified to if the pain is radiating.)
The pain doesn’t radiate anywhere. It’s mostly just right in the middle of my chest. (Clarified to if the pain is radiating.)  If your arm hurts (Clarified to Do you have pain in your arm?.)
If your arm hurts (Clarified to Do you have pain in your arm?.)Question
10/05/20 1:26 PM MDT
 No, when I am having the chest pain, it’s mostly just in middle of my chest. (Clarified to if I have pain in my arm.)
No, when I am having the chest pain, it’s mostly just in middle of my chest. (Clarified to if I have pain in my arm.)  Do you have a pain in your shoulder ?
Do you have a pain in your shoulder ?Question
10/05/20 1:27 PM MDT
 No, the pain hasn’t been in my shoulder.
No, the pain hasn’t been in my shoulder.  Do you have a back pain ?
Do you have a back pain ?Question
10/05/20 1:27 PM MDT
 I haven’t had back pain, no.
I haven’t had back pain, no.  Can you tell me the duration of the pain ? (No matching questions found.)
Can you tell me the duration of the pain ? (No matching questions found.)Question
10/05/20 1:28 PM MDT
 Can you describe the duration of the pain ? (Clarified to Can you tell me what the pain is like?.)
Can you describe the duration of the pain ? (Clarified to Can you tell me what the pain is like?.)Question
10/05/20 1:28 PM MDT
 Well, it mostly feels tight and uncomfortable right in the middle of my chest. (Clarified to if I can tell you what the pain is like.)
Well, it mostly feels tight and uncomfortable right in the middle of my chest. (Clarified to if I can tell you what the pain is like.)  How often pain occurs ? (Clarified to How often do you have pain?.)
How often pain occurs ? (Clarified to How often do you have pain?.)Question
10/05/20 1:29 PM MDT
 Well, it has happened three times the past month. It usually goes away after about a couple of minutes. (Clarified to how often I have pain.)
Well, it has happened three times the past month. It usually goes away after about a couple of minutes. (Clarified to how often I have pain.)  Can you describe your pain from 0 to 10 scale ?
Can you describe your pain from 0 to 10 scale ?Question
10/05/20 1:29 PM MDT
 I’d say maybe a . . . 5? It’s just really uncomfortable . . . like there’s nothing I can do about it. Right now it’s like a zero though.
I’d say maybe a . . . 5? It’s just really uncomfortable . . . like there’s nothing I can do about it. Right now it’s like a zero though.  Sorry to hear that
Sorry to hear thatEmpathize
10/05/20 1:30 PM MDT
 Thanks. I appreciate that.
Thanks. I appreciate that.  Can you describe your pain ?
Can you describe your pain ?Question
10/05/20 1:31 PM MDT
 Well, it mostly feels tight and uncomfortable right in the middle of my chest.
Well, it mostly feels tight and uncomfortable right in the middle of my chest.  ASA pain crashing ? (Clarified to Do you take aspirin?.)
ASA pain crashing ? (Clarified to Do you take aspirin?.)Question
10/05/20 1:31 PM MDT
 I usually just take Tylenol or ibuprofen. (Clarified to if I take aspirin.)
I usually just take Tylenol or ibuprofen. (Clarified to if I take aspirin.)  What is the dosage of Tylenol are you taking ?
What is the dosage of Tylenol are you taking ?Question
10/05/20 2:35 PM MDT
 Just whatever the bottle recommends for an adult.
Just whatever the bottle recommends for an adult.  What is the dosage of ibuprofen you taking ? (Clarified to What is the strength of the ibuprofen you take?.)
What is the dosage of ibuprofen you taking ? (Clarified to What is the strength of the ibuprofen you take?.)Question
10/05/20 2:35 PM MDT
 Just whatever the bottle recommends for an adult. (Clarified to What strength ibuprofen I take.)
Just whatever the bottle recommends for an adult. (Clarified to What strength ibuprofen I take.)  Is it Tylenol helps ?
Is it Tylenol helps ?Question
10/05/20 2:35 PM MDT
 Just a couple when I get a headache, which is not very often.
Just a couple when I get a headache, which is not very often.  How often do you take Tylenol ?
How often do you take Tylenol ?Question
10/05/20 2:36 PM MDT
 I took some today . . . maybe every couple days for mild pain.
I took some today . . . maybe every couple days for mild pain.  What is the reason you’re taking ibuprofen ?
What is the reason you’re taking ibuprofen ?Question
10/05/20 2:36 PM MDT
 Just when I need it for various aches and pains. Probably not more than 3 or 4 times a month.
Just when I need it for various aches and pains. Probably not more than 3 or 4 times a month.  Where else do you have a pain ?
Where else do you have a pain ?Question
10/05/20 2:36 PM MDT
 No, when I am having the chest pain, it’s mostly just in middle of my chest.
No, when I am having the chest pain, it’s mostly just in middle of my chest.  Do you have a pain somewhere else in your body ?
Do you have a pain somewhere else in your body ?Question
10/05/20 2:37 PM MDT
 No, when I am having the chest pain, it’s mostly just in middle of my chest.
No, when I am having the chest pain, it’s mostly just in middle of my chest.  What is the aggravating factors ? (Clarified to Are there any aggravating factors?.)
What is the aggravating factors ? (Clarified to Are there any aggravating factors?.)Question
10/05/20 2:37 PM MDT
 Well, the pain seems to start when I’m doing something physical . . . the first time it happened while I was doing yard work, and the second time . . . I had to take the stairs at work because the elevator broke. Both times it got better if I took a break or sat down to rest. (Clarified to if there are aggravating factors.)
Well, the pain seems to start when I’m doing something physical . . . the first time it happened while I was doing yard work, and the second time . . . I had to take the stairs at work because the elevator broke. Both times it got better if I took a break or sat down to rest. (Clarified to if there are aggravating factors.)  What activity triggers pain ?
What activity triggers pain ?Question
10/05/20 2:39 PM MDT
 If I’m up and moving around I definitely notice it more and it makes me feel like I should sit down and take a deep breath or something.
If I’m up and moving around I definitely notice it more and it makes me feel like I should sit down and take a deep breath or something.  He’s a pain worse when you eat ?
He’s a pain worse when you eat ?Question
10/05/20 2:40 PM MDT
 I don’t think eating has anything to do with it. One episode did happen when my wife and I were out for dinner, but it seemed to happen before we even settled. The episodes don’t seem all that related, to be honest.
I don’t think eating has anything to do with it. One episode did happen when my wife and I were out for dinner, but it seemed to happen before we even settled. The episodes don’t seem all that related, to be honest.  It can be a lot of triggers in your diet which would aggravate and trigger your pain Mr.Foster.
It can be a lot of triggers in your diet which would aggravate and trigger your pain Mr.Foster.Educate
10/05/20 2:43 PM MDT
 Good to know. Thank you.
Good to know. Thank you.  Do you like spicy food ?
Do you like spicy food ?Question
10/05/20 2:43 PM MDT
 Sure, I like spicy food. I don’t eat it very often, though. Maybe once or twice a month.
Sure, I like spicy food. I don’t eat it very often, though. Maybe once or twice a month.  Do you like high-fat food ? (Clarified to Do fatty foods cause the pain?.)
Do you like high-fat food ? (Clarified to Do fatty foods cause the pain?.)Question
10/05/20 2:44 PM MDT
 I don’t think that has anything to do with it, but I guess I don’t know. (Clarified to if fatty foods cause the pain.)
I don’t think that has anything to do with it, but I guess I don’t know. (Clarified to if fatty foods cause the pain.)  What relieves your pain ?
What relieves your pain ?Question
10/05/20 2:44 PM MDT
 I’m not sure. I think lying still seems to help a little.
I’m not sure. I think lying still seems to help a little.  Take anything for chest pain ?
Take anything for chest pain ?Question
10/05/20 2:46 PM MDT
 No, not yet.
No, not yet.  Do you take medication for hypertension ?
Do you take medication for hypertension ?Question
10/05/20 2:46 PM MDT
 I take metoprolol, yes. [AUDIO COMING SOON]
I take metoprolol, yes. [AUDIO COMING SOON]  Is a dosage of Metoprolol ? (Clarified to What dose of Lopressor do you take?.)
Is a dosage of Metoprolol ? (Clarified to What dose of Lopressor do you take?.)Question
10/05/20 2:47 PM MDT
 I think it’s 100 mg, once a day. (Clarified to what dose of Lopressor I take.)
I think it’s 100 mg, once a day. (Clarified to what dose of Lopressor I take.)  Do you take any medication for hyperlipidemia ?
Do you take any medication for hyperlipidemia ?Question
10/05/20 2:47 PM MDT
 I take atorvastatin. [AUDIO COMING SOON]
I take atorvastatin. [AUDIO COMING SOON]  What is the dosage of atorvastatin are you taking ?
What is the dosage of atorvastatin are you taking ?Question
10/05/20 2:48 PM MDT
 I think it’s twenty milligrams a day.
I think it’s twenty milligrams a day.  Do you take over-the-counter medications ?
Do you take over-the-counter medications ?Question
10/05/20 2:48 PM MDT
 Oh, just ibuprofen or Tylenol occasionally for pain.
Oh, just ibuprofen or Tylenol occasionally for pain.  Do you take any supplements ?
Do you take any supplements ?Question
10/05/20 2:48 PM MDT
 I take fish oil, that’s it.
I take fish oil, that’s it.  How frequently you take medication for hyperlipidemia ? (Clarified to Do you take cholesterol medication?.)
How frequently you take medication for hyperlipidemia ? (Clarified to Do you take cholesterol medication?.)Question
10/05/20 2:49 PM MDT
 I take atorvastatin. [AUDIO COMING SOON] (Clarified to if I take cholesterol medication.)
I take atorvastatin. [AUDIO COMING SOON] (Clarified to if I take cholesterol medication.)  How often do you take atorvastatin ?
How often do you take atorvastatin ?Question
10/05/20 2:50 PM MDT
 I take them daily. I’m pretty good about following the doctor’s orders.
I take them daily. I’m pretty good about following the doctor’s orders.  When have you been diagnosed with high blood pressure ?
When have you been diagnosed with high blood pressure ?Question
10/05/20 2:51 PM MDT
 Yes, I supposedly have moderately high blood pressure.
Yes, I supposedly have moderately high blood pressure.  When you started to take metoprolol ?
When you started to take metoprolol ?Question
10/05/20 2:51 PM MDT
 I think it’s been about one year.
I think it’s been about one year.  When have you been diagnosed with hyperlipidemia ? (Clarified to Do you have an anxiety disorder?.)
When have you been diagnosed with hyperlipidemia ? (Clarified to Do you have an anxiety disorder?.)Question
10/05/20 2:51 PM MDT
 I’ve never had any anxiety problems before. [AUDIO COMING SOON] (Clarified to if I have an anxiety disorder.)
I’ve never had any anxiety problems before. [AUDIO COMING SOON] (Clarified to if I have an anxiety disorder.)  When have you been diagnosed with hyperlipidemia ? (Clarified to Are you diagnosed with high blood pressure?.)
When have you been diagnosed with hyperlipidemia ? (Clarified to Are you diagnosed with high blood pressure?.)Question
10/05/20 2:52 PM MDT
 Yes, I supposedly have moderately high blood pressure. (Clarified to if I have been diagnosed with hypertension.)
Yes, I supposedly have moderately high blood pressure. (Clarified to if I have been diagnosed with hypertension.)  I’m sorry to hear that
I’m sorry to hear thatEmpathize
10/05/20 2:52 PM MDT
 Thanks. I appreciate that.
Thanks. I appreciate that.  Do you do exercise ?
Do you do exercise ?Question
10/05/20 2:53 PM MDT
 Well I used to ride my bike a lot but it got stolen a couple years ago. I guess I haven’t had much regular exercise since then. I want to get a new bike if the doctor says it is OK to exercise with this chest pain I’ve been having.
Well I used to ride my bike a lot but it got stolen a couple years ago. I guess I haven’t had much regular exercise since then. I want to get a new bike if the doctor says it is OK to exercise with this chest pain I’ve been having.  I’m sorry to hear that your bike was stolen
I’m sorry to hear that your bike was stolenEmpathize
10/05/20 2:53 PM MDT
 Thanks. I appreciate that.
Thanks. I appreciate that.  When did the exercise last time ?
When did the exercise last time ?Question
10/05/20 2:53 PM MDT
 Well I used to ride my bike a lot but it got stolen a couple years ago. I guess
Well I used to ride my bike a lot but it got stolen a couple years ago. I guess READ MORE >>
NURS 6521 Assignment: Off-Label Drug Use in Pediatrics Sample Paper 1Major depre ...
NURS 6521 Assignment: Off-Label Drug Use in Pediatrics Sample Paper 1
Major depressive disorder is a significant pediatric and adolescent health problem associated with significant morbidity. These patients suffer from impaired social functioning, school difficulties and have an increased risk of physical illness and substance abuse. It is also associated with an increased risk of mortality by suicide. Treatment should therefore be initiated with both psychotherapy and pharmacotherapy.
Choosing of antidepressant is however a challenge for pediatric patients. This is because of the smaller evidence available for antidepressant efficacy compared to adult patients. Selective serotonin reuptake inhibitors (SSRIs) are the first line antidepressants in both pediatric and adult patients with only a few of these antidepressants FDA approved to be used in pediatrics.
The lack of FDA approval for pediatric patients is mostly attributed to the lack of sufficient testing. This means that some antidepressants used in pediatrics are prescribed off—label. Use of off-label drugs is common in pediatrics. Off label drugs use is when drugs are used for treatment of conditions different from the ones they were originally intended for (Gore et al., 2017).
Off-label drug use is recommended in children if they do not receive adequate improvement after using first line drugs (Dwyer & Bloch, 2019). In patients with depressive disorders, improvements can be seen when switching form one SSRI to another e.g., when a switch from Prozac to Zoloft is made (Boyce et al., 2020).
However, certain considerations need to be made when drugs are used off label. These include the child’s body weight and stage of development. This is relevant because these factors can affect how the child will tolerate the drug (Collier et al.,2017). Metabolism is also affected by these factors and consequently the amount of drugs prescribed. Another important consideration is the side effects associated with the drugs. SSRIs, for example, are more likely to cause suicidal ideations in pediatric and adolescent patients than in adults.
NURS 6521 Assignment: Off-Label Drug Use in Pediatrics References
Boyce, P., Hopwood, M., Morris, G., Hamilton, A., Bassett, D., Baune, B. T., Mulder, R., Porter, R., Parker, G., Singh, A. B., Outhred, T., Das, P., & Malhi, G. S. (2020). Switching antidepressants in the treatment of major depression: When, how and what to switch to?. Journal of Affective Disorders, 261, 160–163. https://doi.org/10.1016/j.jad.2019.09.082
Collier, H., Nasim, M., & Gandhi, A. (2017). Prescribing in obese children: how good are paediatricians?. Archives Of Disease In Childhood, 102(1), 61–62. https://doi.org/10.1136/archdischild-2016-310603
Dwyer, J. B., & Bloch, M. H. (2019). Antidepressants for Pediatric Patients. Current Psychiatry, 18(9), 26–42F. https://pubmed.ncbi.nlm.nih.gov/31511767/
Gore, R., Chugh, P. K., Tripathi, C. D., Lhamo, Y., & Gautam, S. (2017). Pediatric Off-Label and Unlicensed Drug Use and Its Implications. Current Clinical Pharmacology, 12(1), 18–25. https://doi.org/10.2174/1574884712666170317161935
NURS 6521 Assignment: Off-Label Drug Use in Pediatrics Sample Paper 2
The use of an approved drugs for unapproved purposes is referred to as off-label use. The U.S. Food and Drug Administration (FDA), an organization in charge of the approval of medication use in the USA, regulates the use and applications of medications. The off-label use of medications is legal and common practice in the United States. This practice is risky in pediatric management because there is limited evidence-based data on the efficacy and safety of certain medications in the pediatric population (Allen et al., 2018). Various research studies have been done by pharmaceutical companies and the department of health to fill the knowledge gap in the past three decades.
Circumstances Under Which Children Should be Prescribed Drugs for Off-Label Use
Off-label prescription happens in the management of pediatrics for various reasons. When a standard, safe, and efficacious therapeutic agent for a particular condition is unavailable, an off-label prescription may be allowed. In pediatrics, this is common with the use of most antibiotic medications. The use of ceftriaxone has been used for most febrile conditions for which its use is not approved by the FDA.
The use of sildenafil for pulmonary hypertension in infants is another example of off-label use of medications (Kelly et al., 2017). In other circumstances off-label prescription in children occurs when the clinical trials in the specific age groups are not available, the standard therapy fails, and when the alternative forms have shown more efficacy and effectiveness than the standard therapy in treating the same condition.
Strategies to Make the off-label Use and Dosage of Drugs Safer
Occasionally, clinicians may carry out off-label prescriptions because the approval process by the FDA takes longer or is quite expensive for a particular medication for which evidence-based trials and studies have shown substantial efficacy. The best strategy to promote medication safety in children can be achieved through improving the process of approval and clinical trials of such medications (Mir & Geer, n.d.).
This mainly applies to chemotherapeutic agents. Various neoplastic conditions common in childhood can also occur in adults. In such cases, the same agents used to manage adults are used in children because there is no approved medication in children (Gore et al., 2017). Pharmacists and physicians should regularly monitor and report adverse reactions in children on off-label prescriptions. Approving the clinical trials of medications in children and neonates makes the overall process of approval faster and efficient.
NURS 6521 Assignment: Off-Label Drug Use in Pediatrics References
Allen, H. C., Garbe, M. C., Lees, J., Aziz, N., Chaaban, H., Miller, J. L., Johnson, P., & DeLeon, S. (2018). Off-label medication use in children, more common than we think: A systematic review of the literature. The Journal of the Oklahoma State Medical Association, 111(8), 776–783. https://www.ncbi.nlm.nih.gov/pubmed/31379392
Gore, R., Chugh, P. K., Tripathi, C. D., Lhamo, Y., & Gautam, S. (2017). Pediatric off-label and unlicensed drug use and its implications. Current Clinical Pharmacology, 12(1), 18–25. https://doi.org/10.2174/1574884712666170317161935
Kelly, L. E., Ohlsson, A., & Shah, P. S. (2017). Sildenafil for pulmonary hypertension in neonates. Cochrane Database of Systematic Reviews, 8, CD005494. https://doi.org/10.1002/14651858.CD005494.pub4
Mir, A. N., & Geer, M. I. (n.d.). Off-label use of medicines in children. International Journal Of Pharmaceutical Sciences And Research. Retrieved February 10, 2021, from https://ijpsr.com/bft-article/off-label-use-of-medicines-in-children/?view=fulltext
READ MORE >>
it can go into your brain and to clog a blood vessel that will be quick or you c ...
it can go into your brain and to clog a blood vessel
that will be quick or you can have
a weak blood vessel wall so that it blows up
like a balloon
READ MORE >>
or is missing. … The response may include an inaccurate and vague explanation ...
30 pts
This criterion is linked to a Learning OutcomeWritten Expression and Formatting – Paragraph Development and Organization: Paragraphs make clear points that support well developed ideas
READ MORE >>
NURS 6521 Week 1 EmmaGarcia Ethical and Legal Aspects of Prescribing Example Sol ...
NURS 6521 Week 1 EmmaGarcia Ethical and Legal Aspects of Prescribing Example Solution
Ethical and Legal Implications of Prescribing Drugs
As an advanced practice nurse prescribing drugs, you are responsible for the safety of your patients each day. The prescriber is responsible for ensuring that any medical intervention they propose will align with the ethical and legal guidelines. The nurse practitioner must be knowledgeable about the most recent rules governing advanced practice nurses with the power to prescribe.
According to Rosenthal and Burchum (2021), writing prescriptions should prioritize patient safety and minimize medication errors through thorough assessment, clear documentation, electronic prescribing systems, and ongoing monitoring. The prescriber should ensure that any intervention taken has to account for the patient’s wishes and those of the family members and the primary caregivers.

Ethical and Legal Implications
- Prescriber:
From the scenario, as an advanced nursing practitioner, prescribing medication makes the nurse face ethical and legal responsibilities. Ethically, the prescriber must prioritize AC’s best interests and respect his autonomy. The prescriber should consider the principle of beneficence by providing appropriate and necessary treatment.
They should also respect AC’s autonomy by ensuring his values and wishes are considered, even without advanced directives (Rosenthal & Burchum, 2021). Legally, the prescriber must follow applicable laws and regulations regarding informed consent, decision-making capacity, and end-of-life care.
- Pharmacist:
The pharmacist has ethical and legal obligations as well. Ethically, the pharmacist should prioritize patient welfare and respect the autonomy of AC. They should ensure that the prescribed medications are appropriate, safe, and effective. The pharmacist may also play a role in counseling the patient’s family about the potential benefits, risks, and alternatives to treatment options. Legally, the pharmacist must adhere to laws and regulations related to medication dispensing, patient privacy, and confidentiality (Rosenthal & Burchum, 2021).
- Patient (AC):
Although unresponsive and unable to communicate, AC has the ethical right to receive appropriate and compassionate care. The ethical principle of autonomy requires that AC’s values and wishes, as expressed by his family, be considered (American Geriatrics Society, 2019). If AC had previously expressed his wishes regarding end-of-life care, those should be respected. The healthcare team must act in his best interests if his wishes are unknown.
- Patient’s Family (wife and daughter):
The wife and daughter have emotional and ethical involvement in AC’s care. Ethically, the wife’s belief that AC would not want to live in his current state should be respected, as it aligns with the principle of autonomy. The daughter’s belief that AC should be kept alive raises questions about the balance between hope and futility. Ethical discussions and family meetings can help address their concerns, consider AC’s values, and reach a consensus regarding his care.
Strategies to Address Disclosure and Non-disclosure
- Open communication and shared decision-making: Engage in open dialogue with the wife, daughter, and other relevant stakeholders. Discuss the prognosis, treatment options, and potential outcomes. Please encourage them to express their concerns, values, and beliefs. By involving them in decision-making, you promote shared decision-making and respect for their autonomy (Rosenthal & Burchum, 2021).
- Respecting patient confidentiality: Maintain patient confidentiality and privacy throughout the discussions. Ensure that sensitive information is only shared with individuals who have a legitimate need to know. Familiarize yourself with the laws specific to your state regarding patient confidentiality and privacy, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States, and adhere to them.
- Exploring legal frameworks: Familiarize yourself with the legal framework in your state regarding disclosure and nondisclosure in healthcare. Laws may vary, but generally, healthcare professionals have a duty to disclose information to patients or their surrogates that is relevant to the patient’s condition and treatment decisions. However, laws also recognize exceptions where disclosure may not be appropriate, such as when it could cause serious harm to the patient or if the patient has explicitly requested nondisclosure (Rosenthal & Burchum, 2021).
- Involving an ethics committee or legal counsel: In complex situations with conflicting views, involving an ethics committee or seeking legal counsel can provide guidance and ensure compliance with legal and ethical obligations. These resources can help navigate the specific laws in your state and provide recommendations on how to address disclosure and nondisclosure appropriately.
Strategies to Guide My Decision Making
- Ethical reflection and consultation: Engaging in ethical reflection allows for a thoughtful examination of the situation, weighing the principles of autonomy, beneficence, and non-maleficence. Consulting with colleagues, an ethics committee, or a supervisor can provide different perspectives and support in decision-making. Discussing the ethical dilemma of disclosing the error with trusted individuals can help ensure a well-considered decision.
- Adherence to professional standards and guidelines: Utilizing professional standards, such as those set forth by nursing organizations, can provide a framework for decision-making. These standards emphasize the importance of patient safety, communication, and accountability. In this scenario, disclosing the error may align with professional standards and guidelines, as it promotes transparency, fosters trust with the patient and family and allows for shared decision-making.
Whether to disclose the error should be carefully considered, considering the potential impact on the patient, their family, and the healthcare team. Justification for disclosing the error may include promoting transparency, maintaining trust, and involving the patient and family in decision-making (Rosenthal & Burchum, 2021). However, it is important to consult legal and institutional policies to ensure compliance with disclosure requirements specific to the jurisdiction.
The Process of Writing Prescriptions
- Patient assessment and diagnosis: Conduct a thorough assessment of the patient, including their medical history, current symptoms, and any allergies or contraindications. Accurate diagnosis is crucial for prescribing the appropriate medication (Shojaei & Salari, 2020).
- Selecting the medication: Choose the most appropriate medicine based on the patient’s diagnosis, considering efficacy, safety, dosage form, and patient-specific factors (e.g., age, comorbidities).
- Determine dosage and frequency: Calculate the correct dosage and frequency of administration based on the patient’s age, weight, renal or hepatic function, and other relevant factors. Double-check calculations and refer to reliable references or prescribing guidelines.
- Write clear and legible prescriptions: Use clear and concise language when writing prescriptions, including the medication name, strength, dosage form, instructions for use, and duration of treatment. Avoid abbreviations or ambiguous terminology to minimize confusion.
- Electronic prescribing systems: Utilize electronic prescribing systems whenever possible, as they can help reduce errors by providing decision support, alerts for potential interactions or allergies, and automated dose calculations.
- Double-check and review: Review the prescription for accuracy and completeness before transmitting or handing it to the patient. Ensure there are no potential drug-drug interactions, duplications, or contraindications (Shojaei & Salari, 2020).
- Communication and patient education: Clearly communicate the prescription instructions to the patient or caregiver, ensuring they understand the medication regimen, potential side effects, and any necessary precautions.
- Ongoing monitoring: Regularly assess the patient’s response to the medication, monitor for adverse effects, and adjust the prescription as needed.
Conclusion
The case scenario presented ethical and legal implications for all stakeholders involved, including the prescriber, pharmacist, patient, and patient’s family. The conflicting perspectives regarding end-of-life care highlighted the importance of open communication, shared decision-making, and respecting patient autonomy. Strategies such as ethical reflection, adherence to professional standards, and consultation with ethics committees or legal counsel can guide decision-making in complex situations.
Additionally, the process of writing prescriptions should prioritize patient safety and minimize medication errors through thorough assessment, clear documentation, electronic prescribing systems, and ongoing monitoring. By considering the ethical and legal aspects while implementing strategies to minimize errors, healthcare professionals can provide compassionate and appropriate care in challenging situations.
NURS 6521 Week 1 EmmaGarcia Ethical and Legal Aspects of Prescribing References
American Geriatrics Society. (2019). Beers Criteria Update Expert Panel. (2019). American Geriatrics Society 2019 updated AGS Beers criteria for potentially inappropriate medication use in older adults. Journal of the American Geriatrics Society Download Journal of the American Geriatrics Society, 67(4), 674–694. https://doi.org/10.1111/jgs.15767
Rosenthal, L. D., & Burchum, J. R. (2021). Lehne’s pharmacotherapeutics for advanced practice nurses and physician assistants (2nd ed.) St. Louis, MO: Elsevier. https://evolve.elsevier.com/cs/product/9780323554954
Shojaei, A., & Salari, P. (2020). COVID-19 and off-label use of drugs: an ethical viewpoint. DARU Journal of Pharmaceutical Sciences, 28, 789-793. https://www.mdpi.com/1383694
Also read:
NURS 6521 Week 2 EmmaGarcia Pharmacotherapy For Cardiovascular Disorders
NURS 6521 Week 3 EmmaGarcia Asthma and Stepwise Management
NURS 6521 Week 4 EmmaGarcia Pharmacotherapy For Gastrointestinal And Hepatobiliary Disorders
NURS 6521 WEEK 1: AT A GLANCE BASIC PHARMACOTHERAPEUTIC CONCEPTS/ETHICAL AND LEGAL ASPECTS OF PRESCRIBING
INTRODUCTION
How do beta-blockers work? What exactly do antibiotics do to the bacteria they target? What effects does an anti-depressant have on blood flow?
Questions like these are related to the underlying pharmacokinetic and pharmacodynamic processes of pharmacotherapeutics. As an advanced practice nurse, understanding these fundamental pharmacotherapeutic concepts is important to ensure that the prescription drugs you recommend for your patients will be safe and effective to treat and/or manage their symptoms. Additionally, as the advanced practice nurse, it is your responsibility to ensure that when prescribing prescription drugs, you adhere to the ethical and legal principles set forth for prescribing drugs as an added layer of protection and safety for the patients you will treat.
This week, you will analyze factors that may influence pharmacokinetic and pharmacodynamics processes of a patient and assess the details of a personalized plan of care that you develop based on influencing factors and patient history. You will also evaluate and analyze ethical and legal implications and practices related to prescribing drugs, including disclosure and nondisclosure, and analyze the process of writing prescriptions to avoid medication errors.
LEARNING OBJECTIVES
Students will:
- Analyze factors that influence pharmacokinetic and pharmacodynamic processes in patients
- Assess patient factors and history to develop personalized plans of care
- Evaluate ethical and legal implications related to prescribing drugs
- Analyze ethical and legal practices of prescribing drugs
- Analyze strategies to address disclosure and nondisclosure
- Justify advanced practice nurse strategies to guide prescription drug decision-making
- Analyze the process of writing prescriptions to avoid medication errors
LEARNING RESOURCES
Required Readings
- Rosenthal, L. D., & Burchum, J. R. (2021). Lehne’s pharmacotherapeutics for advanced practice nurses and physician assistants(2nd ed.) St. Louis, MO: Elsevier.
- Chapter 1, “Prescriptive Authority” (pp. 1–3)
- Chapter 2, “Rational Drug Selection and Prescription Writing” (pp. 4–7)
- Chapter 3, “Promoting Positive Outcomes of Drug Therapy” (pp. 8–12)
- Chapter 4, “Pharmacokinetics, Pharmacodynamics, and Drug Interactions” (pp. 13–33)
- Chapter 5, “Adverse Drug Reactions and Medication Errors” (pp. 34–42)
- Chapter 6, “Individual Variation in Drug Response” (pp. 43–45)
- American Geriatrics Society 2019 Beers Criteria Update Expert Panel. (2019). American Geriatrics Society 2019 updated AGS Beers criteria for potentially inappropriate medication use in older adults. Journal of the American Geriatrics SocietyDownload Journal of the American Geriatrics Society, 67(4), 674–694. doi:10.1111/jgs.15767
American Geriatrics Society 2019 updated AGS Beers criteria for potentially inappropriate medication use in older adults by American Geriatrics Society, in Journal of the American Geriatrics Society, Vol. 67/Issue 4. Copyright 2019 by Blackwell Publishing. Reprinted by permission of Blackwell Publishing via the Copyright Clearance Center.
This article is an update to the Beers Criteria, which includes lists of potentially inappropriate medications to be avoided in older adults as well as newly added criteria that lists select drugs that should be avoided or have their dose adjusted based on the individual’s kidney function and select drug-drug interactions documented to be associated with harms in older adults.
- Drug Enforcement Administration. (2021). CFR – Code of Federal Regulations Title 21. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?CFRPart=1300
This website outlines the code of federal regulations for prescription drugs.
- Drug Enforcement Administration. (n.d.). Mid-level practitioners authorization by state. Retrieved May 13, 2019 from http://www.deadiversion.usdoj.gov/drugreg/practioners/index.html
This website outlines the schedules for controlled substances, including prescriptive authority for each schedule.
- Institute for Safe Medication Practices. (2017). List of error-prone abbreviations, symbols, and dose designations. Retrieved from https://www.ismp.org/recommendations/error-prone-abbreviations-list
This website provides a list of prescription-writing abbreviations that might lead to misinterpretation, as well as suggestions for preventing resulting errors.
- Sabatino, J. A., Pruchnicki, M. C., Sevin, A. M., Barker, E., Green, C. G., & Porter, K. (2017). Improving prescribing practices: A pharmacist?led educational intervention for nurse practitioner students. Journal of the American Association of Nurse Practitioners, 29(5), 248–254. https://doi:10.1002/2327-6924.12446
The authors of this article assess the impact of a pharmacist?led educational intervention on family nurse practitioner (FNP) students’ prescribing skills, perception of preparedness to prescribe, and perception of pharmacist as collaborator.
Required Media
Introduction to Advanced Pharmacology
- Meet Dr. Terry Buttaro, associate professor of practice at Simmons College of Nursing and Health Sciences as she discusses the importance of pharmacology for the advanced practice nurse.
Time Estimate: 8 minutes
- Speed Pharmacology. (2016). Pharmacology – Adrenergic receptors & agonists.(MADE EASY) [Video]. https://www.youtube.com/watch?v=KtmV-yMDYPI&t=372s
Note: This media program is approximately 18 minutes.
- Speed Pharmacology. (2017). Drugs for Hyperlipidemia (Made Easy)Links to an external site.[Video]. https://www.youtube.com/watch?v=Of1Aewx-zRM&t=24s
Note: This media program is approximately 14 minutes.
NURS 6521 Week 1 Discussion
To prepare:
- Review the Resources for this module and consider the principles of pharmacokinetics and pharmacodynamics.
- Reflect on your experiences, observations, and/or clinical practices from the last 5 years and think about how pharmacokinetic and pharmacodynamic factors altered his or her anticipated response to a drug.
- Consider factors that might have influenced the patient’s pharmacokinetic and pharmacodynamic processes, such as genetics (including pharmacogenetics), gender, ethnicity, age, behavior, and/or possible pathophysiological changes due to disease.
- Think about a personalized plan of care based on these influencing factors and patient history in your case study.
BY DAY 3 OF WEEK 1
Post a description of the patient case from your experiences, observations, and/or clinical practice from the last 5 years. Then, describe factors that might have influenced pharmacokinetic and pharmacodynamic processes of the patient you identified. Finally, explain details of the personalized plan of care that you would develop based on influencing factors and patient history in your case. Be specific and provide examples.
Week 1 Discussion Sample
While working at a medical ward in my 4th year of practice, I encountered a 72-year-old male named Mr. Smith. The patient had been in the ward for over a month and presented with hypertension and chronic kidney disease. His blood pressure was through the roof as he had a history of non-compliance with medication regimens and a significant genetic predisposition to drug metabolism variations. The patient has been on antihypertensives but has no detectable elevated blood pressure changes.
Factors That May Have Influenced Mr. Smith’s Pharmacokinetic and Pharmacodynamic Responses
- Genetics and Pharmacogenetics: Mr. Smith may have had changed drug metabolism and clearance rates due to genetic differences in drug-metabolizing enzymes, such as cytochrome P450 enzymes. Higher medication concentrations and a higher likelihood of negative consequences may follow (Rosenthal & Burchum, 2021).
- Age: Given Mr. Smith’s age of 65, changes in drug absorption, distribution, metabolism, and excretion due to aging may take place. For instance, decreased renal function in CKD may impact medication clearance, potentially causing drug buildup and protracted effects.
- Pathophysiological Changes: Mr. Smith’s chronic kidney disease may have changed his pharmacokinetic characteristics, particularly for medications whose main route of elimination are the kidneys. Medication clearance may be lowered, and medication exposure may rise due to impaired renal function (American Geriatrics Society, 2019).
- Non-Compliance: The effectiveness of Mr. Smith’s prescription antihypertensive medicine may have been harmed by his prior history of non-compliance with medication regimens. Drug levels in the body can fluctuate due to inconsistent drug use, which can lessen the intended therapeutic effects.
Individualized Plan of Care:
Mr. Smith could have the individualized plan of care listed below based on the patient’s medical history and contributing factors:
- Pharmacogenetic testing should be carried out to find particular genetic variants that could affect medication metabolism. The likelihood of adverse drug reactions can be decreased by using this information to help with dosage modifications and medication selection.
- Individualized Dosing: Change the antihypertensive drug dosage based on Mr. Smith’s renal function and pharmacokinetic data. Regular medication level monitoring and renal function testing are essential for appropriate dosing.
- Patient Education and Counseling: Stress to Mr. Smith the value of drug compliance. Inform him of the dangers of disobeying instructions and the advantages of constantly following his prescribed drugs (Rosenthal & Burchum, 2021).
- Use a multidisciplinary approach to manage Mr. Smith’s chronic kidney illness and monitor his renal function. The effectiveness of the treatment should be checked frequently, and the prescription schedule should be changed as necessary.
References
American Geriatrics Society (2019). Beers Criteria Update Expert Panel. (2019). American Geriatrics Society 2019 updated AGS Beers criteria for potentially inappropriate medication use in older adults. Journal of the American Geriatrics Society Download Journal of the American Geriatrics Society, 67(4), 674–694. https://doi.org/10.1111/jgs.15767
Rosenthal, L. D., & Burchum, J. R. (2021). Lehne’s pharmacotherapeutics for advanced practice nurses and physician assistants (2nd ed.) St. Louis, MO: Elsevier. https://evolve.elsevier.com/cs/product/9780323554954
NURS 6521 Week 1 Assignment 2 ETHICAL AND LEGAL IMPLICATIONS OF PRESCRIBING DRUGS
What type of drug should you prescribe based on your patient’s diagnosis? How much of the drug should the patient receive? How often should the drug be administered? When should the drug not be prescribed? Are there individual patient factors that could create complications when taking the drug? Should you be prescribing drugs to this patient? How might different state regulations affect the prescribing of this drug to this patient?
These are some of the questions you might consider when selecting a treatment plan for a patient.
As an advanced practice nurse prescribing drugs, you are held accountable for people’s lives every day. Patients and their families will often place trust in you because of your position. With this trust comes power and responsibility, as well as an ethical and legal obligation to “do no harm.” It is important that you are aware of current professional, legal, and ethical standards for advanced practice nurses with prescriptive authority.
Additionally, it is important to ensure that the treatment plans and administration/prescribing of drugs is in accordance with the regulations of the state in which you practice. Understanding how these regulations may affect the prescribing of certain drugs in different states may have a significant impact on your patient’s treatment plan. In this Assignment, you explore ethical and legal implications of scenarios and consider how to appropriately respond.
Please use the following scenario for this assignment:
- AC is a 72-year-old male who is admitted to your ICU after suffering a massive stroke that has left him unresponsive and unable to communicate. He is currently on a ventilator. His wife of 48 years is available along with their one adult daughter. The wife informs you that they don’t have any advanced directives, but she is “pretty sure her husband would not want to live like this.” However, their daughter is adamant her dad would want to be kept alive in case there is any chance to come out of this.
Talk to you all soon!
To Prepare:
- Review the Resources for this module and consider the legal and ethical implications of prescribing prescription drugs, disclosure, and nondisclosure.
- Review the scenario assigned by your Instructor for this Assignment.
- Search specific laws and standards for prescribing prescription drugs and for addressing medication errors for your state or region, and reflect on these as you review the scenario assigned by your Instructor.
- Consider the ethical and legal implications of the scenario for all stakeholders involved, such as the prescriber, pharmacist, patient, and patient’s family.
- Think about two strategies that you, as an advanced practice nurse, would use to guide your ethically and legally responsible decision-making in this scenario, including whether you would disclose any medication errors.
BY DAY 7 OF WEEK 1
Write a 2- to 3-page paper that addresses the following:
- Explain the ethical and legal implications of the scenario you selected on all stakeholders involved, such as the prescriber, pharmacist, patient, and patient’s family.
- Describe strategies to address disclosure and nondisclosure as identified in the scenario you selected. Be sure to reference laws specific to your state.
- Explain two strategies that you, as an advanced practice nurse, would use to guide your decision making in this scenario, including whether you would disclose your error. Be sure to justify your explanation.
- Explain the process of writing prescriptions, including strategies to minimize medication errors.
Reminder: The College of Nursing requires that all papers submitted include a title page, introduction, summary, and references. The College of Nursing Writing Template with Instructions provided at the Walden Writing Center offers an example of those required elements (available at https://academicguides.waldenu.edu/writingcenter/templates/general#s-lg-box-20293632.). All papers submitted must use this formatting.
Rubric – NURS_6521_Week1_Assignment_Rubric
NURS_6521_Week1_Assignment_Rubric
Criteria
Ratings
Pts
This criterion is linked to a Learning OutcomeExplain the ethical and legal implications of the scenario you selected on all stakeholders involved such as the prescriber, pharmacist, patient, and the patient’s family.
25 to >22.25 pts
Excellent
The response accurately and thoroughly explains in detail the ethical and legal implications of the scenario selected on all stakeholders involved. … The response includes accurate, clear, and detailed explanations as to how these implications affect the prescriber, pharmacist, patient, and the patient’s family.
22.25 to >19.75 pts
Good
The response explains the ethical and legal implications of the scenario selected on all stakeholders involved. … The response includes accurate explanations as to how these implications affect the prescriber, pharmacist, patient, and the patient’s family.
19.75 to >17.25 pts
Fair
The response inaccurately or vaguely explains the ethical and legal implications of the scenario selected for all stakeholders involved. … The response includes vague explanations as to how these implications affect the prescriber, pharmacist, patient, and the patient’s family.
17.25 to >0 pts
Poor
The response vaguely and inaccurately explains the ethical and legal implications of the scenario selected for all stakeholders involved, or the response is missing. … The response vaguely and inaccurately explains how these implications affect the prescriber, pharmacist, patient, and the patient’s family, or is missing.
25 pts
This criterion is linked to a Learning OutcomeDescribe strategies to address disclosure and nondisclosure as identified in the scenario selected. Be sure to reference laws specific to your state.
20 to >17.8 pts
Excellent
An accurate, detailed, and clear description of strategies to address disclosure and nondisclosure as identified in the scenario selected is provided. … The response includes specific, detailed, and accurate reference to state laws related to the scenario.
17.8 to >15.8 pts
Good
An accurate description of strategies to address disclosure and nondisclosure as identified in the scenario selected is provided. … The response includes accurate reference to state laws related to the scenario.
15.8 to >13.8 pts
Fair
A vague or inaccurate description of strategies to address disclosure and nondisclosure as identified in the scenario selected is provided. … The response includes inaccurate or vague reference to state laws related to the scenario.
13.8 to >0 pts
Poor
A vague and inaccurate description of strategies to address disclosure and nondisclosure as identified in the scenario selected is provided, or is missing. … The response includes vague and inaccurate reference to state laws related to the scenario, or is missing.
20 pts
This criterion is linked to a Learning OutcomeExplain two strategies that you, as an advanced practice nurse would use to guide your decision making in this scenario, including whether you would disclose your error. Be sure to justify your explanation.
20 to >17.8 pts
Excellent
The response accurately and thoroughly explains in detail at least two strategies that an advanced practice nurse would use to guide decision making in the scenario. … The response accurately and completely explains whether they would disclose the error, including an accurate, detailed, and clear justification for the explanation provided.
17.8 to >15.8 pts
Good
The response accurately explains at least two strategies that an advanced practice nurse would use to guide decision making in the scenario. … The response accurately explains whether they would disclose the error, including an accurate justification for the explanation provided.
15.8 to >13.8 pts
Fair
The response inaccurately or vaguely explains at least two strategies that an advanced practice nurse would use to guide decision making in the scenario, or only explains one strategy. … The response inaccurately or vaguely explains whether they would disclose the error, including a justification that is vague, inaccurate, or misaligned to the explanation provided.
13.8 to >0 pts
Poor
The response inaccurately and vaguely explains only one strategy that an advanced practice nurse would use to guide decision making in the scenario, or is missing. … The response inaccurately and vaguely explains whether they would disclose the error, with no justification provided, or is missing.
20 pts
This criterion is linked to a Learning OutcomeExplain the process of writing prescriptions including strategies to minimize medication errors.
20 to >17.8 pts
Excellent
The response provides an accurate, detailed, and thorough explanation of the process of writing prescriptions, including detailed strategies to minimize medication errors.
17.8 to >15.8 pts
Good
The response provides an accurate explanation of the process of writing prescriptions, including some strategies to minimize medication errors.
15.8 to >13.8 pts
Fair
The response provides an inaccurate or vague explanation of the process of writing prescriptions, including inaccurate or vague strategies to minimize medication errors.
13.8 to >0 pts
Poor
The response provides an inaccurate and vague explanation of the process of writing prescriptions, including inaccurate and vague strategies to minimize medication errors, or is missing.
20 pts
This criterion
READ MORE >>
NURS 6521 Week 11 Sample DiscussionPatient Preferences and Decision MakingDiseas ...
NURS 6521 Week 11 Sample Discussion
Patient Preferences and Decision Making
Diseases and treatments can become compound, thus involving patients in the decision-making process is essential. Patient participation or involvement in the care process entails shared decision-making or allowing patients to share their views concerning distinct treatment procedures. Factors impacting patient involvement include reasons connected to health care experts like clinician-clientele interaction, allocation of adequate time for involvement, and acknowledgment of patient’s knowledge. Other factors are client-related and include patient’s cognitive and physical capacity, values, beliefs, knowledge, and emotional connections. Essentially, patient participation empowers patients, enhances health results and services, and ensures jointly agreeable medical decisions.
My experience involved providing patient J. R. with CRC (colorectal cancer) screening decision aids, to categorize a chosen screening alternative. Involving J. R in the decision-making process when faced with delicate selections in relation to cancer treatment and screening was vital to the conception of patient-based care. The process took place within the setting of SDM (shared decision making), where J. R and a team of care providers formed a partnership to simplify principles and morals, discuss statistics, and convey a jointly agreeable medical decision.
Essentially, collaborative decision-making tends to empower patients to make a knowledgeable, value-based decision concerning a particular course of action of care. Such empowerment enhances the patient’s comprehension of probable risks, benefits, scientific uncertainty, and probabilities. Decision aids also enhance the efficiency and quality of the patient-clinician encounter and enable patients to engage in decision-making (Melnyk & Fineout-Overholt, 2011). Research has proved that decision aids boost familiarity and information, alleviate decisional conflict, facilitate informed value-founded verdicts, and raises participation in the decision-making procedure (The Ottawa Hospital Research Institute, 2019). However, their influence on the decision quality, health outcomes, and satisfaction with the procedure of making decisions is still uncertain.
The decision aid tool employed art graphics and pictures, and videotaped narratives in DVD data format to communicate crucial statistics concerning colorectal cancer and the significance of screening. The graphics and narratives also compared the five suggested screening alternatives utilizing both option-based and attribute-based methodologies, and prompt patient partialities. The implement also integrated the CRC risk assessment tool. Patient J. R. engaged in an interactional computer forum before a planned session with the practitioner.
The decision aids tool allowed J. R. to classify a chosen screening selection founded on the comparative ideals based on distinct test features. The tool also increased J.R.’s understanding and familiarity with CRC screening. Unlike other patients who did not engage in patient participation, J. R.’s fulfillment with the decision-making procedure and screening purposes was augmented. However, in a case where the provider’s and patient’s preferences vary, test ordering and screening intentions are negatively impacted (Schroy, et al, 2014). Fortunately, J. R.’s and the provider’s test ordering and screening intentions were similar, providing patient satisfaction and the best outcomes.
Patient involvement in the decision-making process is a suitable use of the client’s clinic time, saves clinicians time, and amplifies patient familiarity with the numerous screening selections, encompassing their risks and benefits. As a result, the process allowed J. R. to categorize a preferred screening option and augmented his wish to get screened.
Notably, the clinician’s impartial and unbiased participation in the valuation of the usefulness of the tool enabled the clinicians to adapt their consultative method to J. R.’s requirements, enhancing the quality of J. R.’s visit, and increasing his satisfaction with care. Significantly, health providers must measure the educational intervention’s impact to validate the achievement of professional development activities (Opperman et al., 2016). A major aspect to consider is the financial impact measurement, including the benefit-cost ratio and cost analysis. It is essential for providers to proactively validate the educational programs and the value of the decision aids tools.
Most critical care professional institutions authorize SDM (shared decision making) as a fundamental element of patient-based care. According to Kon et al. (2016), providers should integrate the decision-making approach in assessing and managing patient’s needs and preferences. Notably, few ethical validations exist for formulating collaborations and partnerships between patients and practitioners. Practitioners have a legitimate function in the procedure of making decisions due to their proficiency in medicine and understanding of the medically specified interventions.
Allowing patients to participate in the procedure demonstrates respect for individuals, a principal ethical duty of the medical profession. Additionally, patient involvement guarantees that the decisions made are in line with the goals, preferences, and values. Hoffman, Montori, & Del Mar assert that shared decision-making and evidence-based medicine are fundamental to quality care, yet the interdependence between the two methods is not commonly appreciated (2014).
The SDM intends to guarantee treatment options and decisions that are medically suitable and compatible with the client’s goals, ideals, and likings. Occasionally, though, such partnerships fail to produce satisfactory decisions for the patient or the clinical team. When such cases arise, it is obliging to conscript the support and aid of clinical ethics counselors at conflict resolution (Kon et al., 2016). Ethical validations promote the decisions made from such partnerships.
As discussed in this paper, patient participation in healthcare decision-making is significant as it empowers and boosts health and services outcomes for the patient. To promote professional practice, it is essential to integrate patient knowledge and viewpoints, alongside the clinician’s scientific and professional clinical knowledge in the care of patients. Specifically, such approach to patient care seeks to address any existing doubts in the minds of patients, in addition to giving them the opportunity to not only share their views, but also actively make decisions based on their treatment preferences.
References
- Hoffman, T. C., Montori, V. M., & Del Mar, C. (2014). The connection between evidence-based medicine and shared decision making. Journal of the American Medical Association, 312(13), 1295–1296. doi:10.1001/jama.2014.10186
- Kon, A. A., Davidson, J. E., Morrison, W., Danis, M., & White, D. B. (2016). Shared decision making in intensive care units: an American College of Critical Care Medicine and American Thoracic Society policy statement. Critical Care Medicine, 44(1), 188–201. doi:10.1097/CCM.0000000000001396
- Melnyk, B. M., & Fineout-Overholt, E. (Eds.). (2011). Evidence-based practice in nursing & healthcare: A guide to best practice. Lippincott Williams & Wilkins.
- Opperman, C., Liebig, D., Bowling, J., Johnson, C. S., & Harper, M. (2016). Measuring Return on Investment for Professional Development Activities:: Implications for Practice. Journal For Nurses In Professional Development, 32(4), 176-184. doi:10.1097/NND.0000000000000483
- Schroy III, P. C., Mylvaganam, S., & Davidson, P. (2014). Provider perspectives on the utility of a colorectal cancer screening decision aid for facilitating shared decision making. Health Expectations, 17(1), 27-35. doi:10.1111/j.1369-7625.2011.00730.x
- The Ottawa Hospital Research Institute. (2019). Patient decision aids. Retrieved from https://decisionaid.ohri.ca/
READ MORE >>
NURS 6521 Week 2 EmmaGarcia Pharmacotherapy For Cardiovascular Disorders Example ...
NURS 6521 Week 2 EmmaGarcia Pharmacotherapy For Cardiovascular Disorders Example
Pharmacotherapy For Cardiovascular Disorders Sample 1
Pharmacokinetic and Pharmacodynamic Processes
The selected factor, genetics, can significantly influence the pharmacokinetic and pharmacodynamic processes in the patient from the provided case study. Starting with pharmacokinetics, genetic variations can impact drug metabolism, absorption, distribution, and elimination. For instance, in this case, the patient’s genetic variations in the CYP2C9 gene can influence the metabolism of warfarin. Reduced enzymatic activity due to specific genetic variants can lead to slower warfarin metabolism, resulting in higher blood levels of the drug. This can increase the risk of bleeding and necessitate lower initial doses of warfarin. Genetics also influence drug transporters (Rosenthal & Burchum, 2021).

The patient’s genetic variations in the ABCB1 gene, encoding P-glycoprotein, can affect the function of this transporter. Reduced P-glycoprotein activity due to genetic variants can lead to higher concentrations of digoxin, a medication transported by P-gp, in the body. This elevated concentration increases the risk of digoxin toxicity and may require lower initial doses of digoxin in patients with such genetic variations (Wojtyniak et al., 2021).
In terms of pharmacodynamics, genetic variants might affect the targets and receptors of drugs. In this case, the patient’s genetic polymorphisms in the ADRB1 gene, coding for beta-1 adrenergic receptors, may impact the sensitivity of these receptors to metoprolol, a beta-blocker (Rosenthal & Burchum, 2021). Specific genetic variants can alter the response to metoprolol, potentially requiring different doses or alternative medications to achieve the desired heart rate control in atrial fibrillation.
Changes
Changes in the pharmacokinetics and pharmacodynamics processes can profoundly impact the recommended drug therapy for the patient described in the case study. One notable area where these changes can influence treatment is drug metabolism. For instance, the patient is prescribed warfarin, an anticoagulant primarily metabolized by the cytochrome P450 enzyme CYP2C9. However, genetic variations in the CYP2C9 gene can alter warfarin’s metabolism rates (Rosenthal & Burchum, 2021).
Patients with specific genetic variants, such as CYP2C92 or CYP2C93, may exhibit reduced enzymatic activity, leading to slower metabolism of warfarin. As a result, their blood levels of warfarin may increase, putting them at a higher risk of bleeding. In such cases, the recommended drug therapy may involve starting with lower initial doses of warfarin and closely monitoring the patient’s International Normalized Ratio (INR) to ensure appropriate anticoagulation.
Additionally, changes in drug transporters can affect drug absorption and distribution. The patient is taking digoxin, a medication transported by the P-glycoprotein (P-gp) transporter. Genetic variations in the ABCB1 gene, which encodes P-gp, can impact its function. Some individuals may have genetic variants that result in reduced P-gp activity, leading to higher concentrations of digoxin in the body. This increased concentration raises the risk of digoxin toxicity. To address this, the recommended drug therapy for patients with such genetic variations may involve starting with lower initial doses of digoxin and monitoring serum digoxin levels to avoid adverse effects.
Furthermore, genetic variations in drug targets can impact drug response. The patient has atrial fibrillation (A.F.) and is prescribed metoprolol, a beta-blocker, to manage her heart rate. However, genetic polymorphisms in the ADRB1 gene, which codes for beta-1 adrenergic receptors, can affect the sensitivity of these receptors to medications like metoprolol (Hirota et al., 2020). Individuals with specific ADRB1 variants may require different doses or alternative medications to achieve the desired heart rate control in A.F.
Improving the Patient’s Drug Therapy Plan
Based on the provided case study, several recommended improvements can be made to improve the patient’s drug therapy plan. Firstly, conducting a comprehensive medication review would be beneficial considering the patient’s age, the potential for polypharmacy, and the presence of delirium.
This review would assess the appropriateness of each medication, evaluate potential drug interactions, and identify any medications that may contribute to or exacerbate the patient’s delirium (Wojtyniak et al., 2021). Considering the patient’s altered level of consciousness, an alternative oral anticoagulant, such as a direct oral anticoagulant (DOAC), could be considered instead of warfarin. DOACs have a more predictable pharmacokinetic profile, fewer interactions, require less monitoring, and have a lower risk of major bleeding.
Adjusting the dose or considering an alternative medication with a more favorable cardiovascular profile may be necessary to manage the patient’s low blood pressure and heart rate while still effectively controlling her heart rate. Lastly, dosage adjustments for medications undergoing renal elimination, such as digoxin, should be considered due to the patient’s chronic kidney disease (CKD).
Close monitoring of renal function and drug levels can help ensure appropriate dosing to minimize the risk of drug toxicity (Wojtyniak et al., 2021). These recommended improvements aim to enhance safety, effectiveness, and patient outcomes. Conducting a medication review, considering alternative anticoagulants, adjusting cardiovascular medications, and accounting for CKD-related dosage adjustments can optimize the medication regimen to better suit the patient’s needs, minimize adverse effects, and improve overall therapeutic outcomes.
Conclusion
Improving the patient’s drug therapy plan based on the case study involves conducting a medication review, considering alternative anticoagulants, adjusting cardiovascular medications, and accounting for CKD-related dosage adjustments. These recommendations are crucial to enhance safety, effectiveness, and overall patient outcomes. Conducting a comprehensive medication review ensures the appropriateness of each medication and minimizes the risk of adverse effects.
Considering alternative anticoagulants like DOACs can provide a more predictable pharmacokinetic profile and lower bleeding risk. Adjusting cardiovascular medications helps manage the patient’s low blood pressure and heart rate more effectively. Dosage adjustments for drugs undergoing renal elimination account for the patient’s CKD, minimizing the risk of drug toxicity. By implementing these improvements, healthcare providers can optimize the patient’s drug therapy plan, tailor it to her specific needs, and improve her treatment’s overall quality and safety.
NURS 6521 Week 2 EmmaGarcia Pharmacotherapy For Cardiovascular Disorders References
Hirota, T., Fujita, Y., & Ieiri, I. (2020). An updated review of pharmacokinetic drug interactions and pharmacogenetics of statins. Expert Opinion on Drug Metabolism & Toxicology, 16(9), 809-822. https://doi.org/10.1080/17425255.2020.1801634
Rosenthal, L., & Burchum, J. (2021). Lehne’s pharmacotherapeutics for advanced practice nurses and physician assistants (2nd ed.). S.L.: Saunders. https://evolve.elsevier.com/cs/product/9780323554954
Wojtyniak, J. G., Selzer, D., Schwab, M., & Lehr, T. (2021). Physiologically based precision dosing approach for drug?drug?gene interactions: A simvastatin network analysis. Clinical Pharmacology & Therapeutics, 109(1), 201-211. https://doi.org/10.1002/cpt.2111
NURS 6521 Module 2: Cardiovascular and Respiratory Systems
MODULE 2: AT A GLANCE
CARDIOVASCULAR AND RESPIRATORY SYSTEMS
WEEK 2
WEEK 3
WHAT’S HAPPENING THIS MODULE?
Module 2: Cardiovascular and Respiratory Systems is a 2-week module, Weeks 2 and 3 of the course. In this module, you will examine how patient factors may influence pharmacokinetic and pharmacodynamic processes of pharmacotherapeutics used in the treatment of cardiovascular and respiratory disorders. You will also explore and suggest drug therapy plans for asthma and analyze the stepwise approach for asthma treatment and management.
INTRODUCTION
Alterations of the cardiovascular system can cause serious adverse events and may lead to death when not treated in a timely and safe manner. Unfortunately, many patients with cardiovascular disorders are unaware until complications appear. In clinical settings, patients often present with symptoms of several cardiovascular disorders, making it essential for you, as the advanced practice nurse, to be able to recognize these symptoms and recommend appropriate drug treatment options.
This week, you examine the impact of patient factors that may lead to changes in pharmacokinetic and pharmacodynamic processes on patient drug therapy for cardiovascular disorders. You also explore ways to improve drug therapy plans for cardiovascular disorders based on patient factors and overall health needs.
LEARNING OBJECTIVES
Students will:
- Analyze the influence of patient factors on pharmacokinetic and pharmacodynamic processes
- Analyze the impact of changes in pharmacokinetic and pharmacodynamic processes on patient drug therapies
- Evaluate drug therapy plans for cardiovascular disorders
PHARMACOTHERAPY FOR CARDIOVASCULAR DISORDERS
…heart disease remains the No. 1 killer in America; nearly half of all Americans have high blood pressure, high cholesterol, or smoke—some of the leading risk factors for heart disease…
—Murphy et al., 2018
Despite the high mortality rates associated with cardiovascular disorders, improved treatment options do exist that can help address those risk factors that afflict the majority of the population today.
As an advanced practice nurse, it is your responsibility to recommend appropriate treatment options for patients with cardiovascular disorders. To ensure the safety and effectiveness of drug therapy, advanced practice nurses must consider aspects that might influence pharmacokinetic and pharmacodynamic processes such as medical history, other drugs currently prescribed, and individual patient factors.
Reference: Murphy, S. L., Xu, J., Kochanek, K. D., & Arias, E. (2018). Mortality in the United States, 2017. Retrieved from https://www.cdc.gov/nchs/products/databriefs/db328.htm
RESOURCES
Be sure to review the Learning Resources before completing this activity.
Click the weekly resources link to access the resources.
WEEKLY RESOURCES
To Prepare
- Review the Resources for this module and consider the impact of potential pharmacotherapeutics for cardiovascular disorders introduced in the media piece.
- Review the case study assigned by your Instructor for this Assignment.
- Select one the following factors: genetics, gender, ethnicity, age, or behavior factors.
- Reflect on how the factor you selected might influence the patient’s pharmacokinetic and pharmacodynamic processes.
- Consider how changes in the pharmacokinetic and pharmacodynamic processes might impact the patient’s recommended drug therapy.
- Think about how you might improve the patient’s drug therapy plan based on the pharmacokinetic and pharmacodynamic changes. Reflect on whether you would modify the current drug treatment or provide an alternative treatment option for the patient.
BY DAY 7 OF WEEK 2
Write a 2- to 3-page paper that addresses the following:
- Explain how the factor you selected might influence the pharmacokinetic and pharmacodynamic processes in the patient from the case study you were assigned.
- Describe how changes in the processes might impact the patient’s recommended drug therapy. Be specific and provide examples.
- Explain how you might improve the patient’s drug therapy plan and explain why you would make these recommended improvements.
Reminder: The College of Nursing requires that all papers submitted include a title page, introduction, summary, and references. The College of Nursing Writing Template with Instructions provided at the Walden Writing Center offers an example of those required elements (available at https://academicguides.waldenu.edu/writingcenter/templates/general#s-lg-box-20293632Links to an external site.). All papers submitted must use this formatting.
SUBMISSION INFORMATION
Before submitting your final assignment, you can check your draft for authenticity. To check your draft, access the Turnitin Drafts from the Start Here area.
- To submit your completed assignment, save your Assignment as WK2Assgn_LastName_Firstinitial
- Then, click on Start Assignmentnear the top of the page.
- Next, click on Upload Fileand select Submit Assignment for review.
NURS_6521_Week2_Assignment_Rubric
Criteria
Ratings
Pts
This criterion is linked to a Learning OutcomeExplain how the factor you selected might influence the pharmacokinetic and pharmacodynamic processes in the patient from the case study you were assigned.
25 to >22.5 pts
Excellent
The response accurately and completely explains in detail how the factor selected might influence the pharmacokinetic and pharmacodynamic processes in the patient.
22.5 to >19.75 pts
Good
The response provides a basic explanation of how the factor selected might influence the pharmacokinetic and pharmacodynamic processes in the patient.
19.75 to >17.25 pts
Fair
The response inaccurately or vaguely explains how the factor selected might influence the pharmacokinetic and pharmacodynamic processes in the patient.
17.25 to >0 pts
Poor
The response inaccurately and vaguely explains how the factor selected might influence the pharmacokinetic and pharmacodynamic processes in the patient, or is missing.
25 pts
This criterion is linked to a Learning OutcomeDescribe how changes in the processes might impact the patient’s recommended drug therapy. Be specific and provide examples.
30 to >26.7 pts
Excellent
The response accurately and completely describes in detail how changes in the processes might impact the patient’s recommended drug therapy. … Accurate, complete, and aligned examples are provided to support the response.
26.7 to >23.7 pts
Good
The response accurately describes how changes in the processes might impact the patient’s recommended drug therapy. … Accurate examples may be provided to support the response.
23.7 to >20.7 pts
Fair
The response inaccurately or vaguely describes how changes in the processes might impact the patient’s recommended drug therapy. … Inaccurate or vague examples are provided to support the response.
20.7 to >0 pts
Poor
The response inaccurately and vaguely describes how changes in the processes might impact the patient’s recommended drug therapy, or is missing. … Inaccurate and vague examples may be provided to support the response, or is missing.
30 pts
This criterion is linked to a Learning OutcomeExplain how you might improve the patient’s drug therapy plan, and explain why you would make these recommended improvements.
30 to >26.7 pts
Excellent
The response accurately and clearly explains in detail how to improve the patient’s drug therapy plan. … The response includes an accurate and detailed explanation to support the recommended improvements.
26.7 to >23.7 pts
Good
The response accurately explains how to improve the patient’s drug therapy plan. … The response may include an accurate explanation to support the recommended improvements.
23.7 to >20.7 pts
Fair
The response inaccurately or vaguely explains how to improve the patient’s drug therapy plan. … The response may include an inaccurate, vague, or misaligned explanation to support the recommended improvements.
20.7 to >0 pts
Poor
The response inaccurately and vaguely explains how to improve the patient’s drug therapy plan, or is missing. … The response may include an inaccurate and vague explanation to support the recommended improvements, or is missing.
30 pts
This criterion is linked to a Learning OutcomeWritten Expression and Formatting – Paragraph Development and Organization: Paragraphs make clear points that support well developed ideas, flow logically, and demonstrate continuity of ideas. Sentences are carefully focused–neither long and rambling nor short and lacking substance.
5 to >4.45 pts
Excellent
Paragraphs and sentences follow writing standards for flow, continuity, and clarity.
4.45 to >3.95 pts
Good
Paragraphs and sentences follow writing standards for flow, continuity, and clarity 80% of the time.
3.95 to >3.45 pts
Fair
Paragraphs and sentences follow writing standards for flow, continuity, and clarity 60%–79% of the time.
3.45 to >0 pts
Poor
Paragraphs and sentences follow writing standards for flow, continuity, and clarity less than 60% of the time.
5 pts
This criterion is linked to a Learning OutcomeWritten Expression and Formatting – English writing standards: Correct grammar, mechanics, and proper punctuation
5 to >4.45 pts
Excellent
Uses correct grammar, spelling, and punctuation with no errors
4.45 to >3.95 pts
Good
Contains a few (1–2) grammar, spelling, and punctuation errors
3.95 to >3.45 pts
Fair
Contains several (3–4) grammar, spelling, and punctuation errors
3.45 to >0 pts
Poor
Contains many (? 5) grammar, spelling, and punctuation errors that interfere with the reader’s understanding
5 pts
This criterion is linked to a Learning OutcomeWritten Expression and Formatting – The paper follows correct APA format for title page, headings, font, spacing, margins, indentations, page numbers, running head, parenthetical/in-text citations, and reference list.
5 to >4.45 pts
Excellent
Uses correct APA format with no errors
4.45 to >3.95 pts
Good
Contains a few (1–2) APA format errors
3.95 to >3.45 pts
Fair
Contains several (3–4) APA format errors
3.45 to >0 pts
Poor
Contains many (? 5) APA format errors
5 pts
Total Points: 100
LEARNING RESOURCES
Required Readings
- Rosenthal, L. D., & Burchum, J. R. (2021). Lehne’s pharmacotherapeutics for advanced practice nurses and physician assistants(2nd ed.) St. Louis, MO: Elsevier.
- Chapter 33, “Review of Hemodynamics” (pp. 285–289)
- Chapter 37, “Diuretics” (pp. 290–296)
- Chapter 38, “Drugs Acting on the Renin-Angiotensin-Aldosterone System” (pp. 297–307)
- Chapter 39, “Calcium Channel Blockers” (pp. 308–312)
- Chapter 40, “Vasodilators” (pp. 313–317)
- Chapter 41, “Drugs for Hypertension” (pp. 316–324)
- Chapter 42, “Drugs for Heart Failure” (pp. 325–336)
- Chapter 43, “Antidysrhythmic Drugs” (pp. 337–348)
- Chapter 44, “Prophylaxis of Atherosclerotic Cardiovascular Disease: Drugs That Help Normalize Cholesterol and Triglyceride Levels” (pp. 349–363)
- Chapter 45, “Drugs for Angina Pectoris” (pp. 364–371)
- Chapter 46, “Anticoagulant and Antiplatelet Drugs” (pp. 372–388)
Required Media
Cardiovascular Disorders
- Meet Dr. Norbert Myslinski as he discusses ACE inhibitors, angiotensin inhibitors, beta-blockers, calcium channel blockers, and diuretics as different categories of hypertension drugs. What potential drugs might be best recommended for patients suffering from hypertension? (8m)
- Walden University. (n.d.). Instructor feedbackLinks to an external site.. https://cdn-media.waldenu.edu/2dett4d/Walden/WWOW/1001/pulse_check/instructor_feedback/index.html#/
[Music] One of the missions
of this course is to straddle the basic sciences
and the clinical sciences. Many years ago,
Sir William Osler said, “One cannot become
a competent clinician “without the full knowledge
of human physiology “and pathology. “Without it,
one flounders along “in an aimless fashion,
never able to gain “an accurate conception
of disease, “practicing a sort
of popgun pharmacy, “hitting now the malady
and again the patient, he himself
not knowing which.” This week,
Dr. Norbert Myslinski examines how categories of drugs
working through different mechanisms can provide
a synergistic effect creating more treatment options. So often in hospitals
and the doctors’ offices and also in medical schools
and nursing schools and dental schools,
there is this dichotomy between the two. I mean, you first learn
the basic sciences, then you forget about those
and you go to the clinics, I think you learn
the real stuff, but we want to do
with this course is to produce a bridge between the two. And make the understanding
of the clinical portions more relevant by knowing
the basic science– knowing the basic science
that we have. Another way in which groups
are important is synergism. In pharmacology,
we have a concept where the effect
of two different drugs is greater than the sum
of the individual drugs and which is very important
when you combine different drugs and especially when you have
groups of drugs or categories that work via
different mechanisms of action. You may have a same end result
of different categories of drugs, but they work
via different mechanisms. And if you do that,
you’re more likely to get a synergistic effect
than if they all worked via the same mechanism. Some drugs work
via same mechanism no matter what
their effects are, okay? For instance, aspirin. Aspirin has many effects,
all right? Aspirin is an analgesic
that alleviates pain. Aspirin is anti-inflammatory,
alleviates inflammation. Aspirin is an anticoagulant
for the blood. Aspirin also is antipyretic. It decreases
body temperature, okay? But how does it do it? It has many effects. By the way, all drugs
have multiple effects. No drug only has one effect. All drugs have
more than one effect. But how does aspirin do
all these different effects? Via the same mechanism. And that’s
through the inhibition of a certain compound
in the body called prostaglandins. So inhibition of the synthesis
of prostaglandins produces all of them. Okay? There are many different types
of prostaglandins and therefore we have
different effects in there, Okay? So if we have
two different drugs, they work via the inhibition
of prostaglandins. Say, aspirin and Tylenol, right? They’re not going to have
a synergistic effect. They’ll have an additive effect,
right? But if you have, for instance,
a narcotic like morphine, okay? And then you also have Tylenol,
you can have a synergistic effect
with those two. Although with Tylenol
and aspirin, there is a ceiling. You can take
two or three tablets and that’s the maximum
pain relief you’re going to get. No matter if you take five
or 10 after that, you may have gastric distress,
but it’s more of an effect, it’s a ceiling. With morphine though
there is no ceiling. You just keep going,
going, going, you get more
and more pain relief, you know, until your respiration
shuts down and you die. So if we look at hypertension,
that silent killer. That’s one disorder
that we have a wealth of groups and categories of drugs working
via many different mechanisms. So we can have
a very nice synergistic effect. We can tailor-make
their pharmacotherapy, you know, so they can control
their blood pressure with the least amount
of side effects and they can function
in society. For example, you have
your ACE inhibitors, you have
your angiotensin inhibitors, you have your beta-blockers,
you have your calcium-channel blockers,
you have your diuretics, all of them can
reduce blood pressure, all of them work
via different mechanisms. There are two types
of blood vessels that go up, which is the carotids
and the vertebrals and then they go into
a little area here and distributed throughout
the brain and one of the most
common causes of disability that we have is stroke. Now, stroke is when you have
a deprivation of oxygen going to a part of the brain. And that’s usually
due to one of three things. Either there is a buildup
of a clot in that blood vessel, a primary site,
so the blood stops going to that area
or you have a clot that breaks off
from a different part of your body, more likely
from the left side of heart because you may have
atherosclerosis, build up of fatty tissues
and clots there and if one breaks off,
it can go into your brain and to clog a blood vessel,
that will be quick or you can have
a weak blood vessel wall so that it blows up
like a balloon, a balloon is aneurysm
and eventually it bursts and when it bursts
then you have a stroke in that part
of the area of brain. Now, the symptoms of a stroke
on many patients that nurses treat
for chronic time periods, the symptoms of a stroke
can be quite varied. You know, as many functions
that are functions of the brain depending upon
where the stroke is, depending upon
where the stroke is, okay? For instance, if it happens here
at the back of the brain, you’ll have a lot
of visual symptoms because this is where
the brain processes visual information,
occipital lobes. If you have one over here
in the temporal lobes, that process is hearing, okay? So you’d have
hearing problems, okay? If you have a stroke
that affects this part over here,
this is somatosensory cortex, you may have a problem
with the feeling, touch, and pressure
in different parts of your body. Over here is the motor cortex
and that has to do with movement. So you may have problems
with movement of your body. Okay, so it all depends upon
where that injury is and it’s very interesting
because when there is a stroke, the main part dies and then
the other parts around it shut down and unless
treatment is given quickly and drugs can be given that can
dissolve a clot real quickly, okay, the part
that sort of are not dead yet, but they are affected
around there if not treated quickly
then that part may also die. And so when you first
have a stroke your symptoms involve
not only the dead part, but also the part back here
sort of shut down, all right? If you’re treated quickly,
if you have the signs of a stroke you have
what we call a brain attack then you get right there
to the emergency center, you can dissolve the clot,
and then you can have reversal of some of the symptoms. Like dysfunction of all
these ones around, the dysfunctional ones can come
back and we can have reversal of the symptoms, but if you
don’t get the treatment, these will eventually die too
and the others– those symptoms will stay around
for a very long time. And so it all depends upon
where the dysfunction is and that determines
what kind of symptoms we have. Captioning performed by
Aegis Communications
Also Read: NURS 6521 Week 1 EmmaGarcia Ethical and Legal Aspects of Prescribing
READ MORE >>
NURS 6521 Week 3 EmmaGarcia Asthma and Stepwise Management Sample Solution Inclu ...
NURS 6521 Week 3 EmmaGarcia Asthma and Stepwise Management Sample Solution Included
Asthma and Stepwise Management Sample Presentation Notes
Slide 1 – Introduction
Welcome to this staff education session on Asthma Management.
This presentation aims to provide valuable insights into understanding and effectively managing asthma in patients.
Healthcare professionals can enhance patient outcomes and the standard of care by improving their knowledge and expertise in managing asthma.
This presentation will explore key concepts, treatment options, and stepwise approaches that empower healthcare providers to deliver optimal care for patients with asthma.
Slide 2 – Long-Term Control Treatment Options for Asthma
In asthma management, various medications play vital roles in achieving long-term control of the disease. Inhaled corticosteroids (ICS) are the cornerstone of long-term control as they effectively reduce airway inflammation, a key component of asthma. These medications help prevent and manage asthma symptoms by reducing inflammation and improving overall lung function. Long-acting beta-agonists (LABAs) are often used in combination with ICS. They work by relaxing the airway muscles, resulting in bronchodilation and improved airflow (Rosenthal & Burchum, 2021). LABAs provide sustained relief and help control symptoms for an extended period.
Leukotriene modifiers are another class of medications used in asthma management. They block the chemicals responsible for inflammation and constriction of the airways, helping to prevent asthma symptoms. Immunomodulators are medications that modify the immune response to prevent asthma symptoms. They target specific components of the immune system involved in the inflammatory process, thereby reducing the frequency and severity of asthma attacks.
Mast cell stabilizers are used to prevent the release of asthma-triggering chemicals from mast cells (Rosenthal & Burchum, 2021). By stabilizing these cells, mast cell stabilizers help reduce airway inflammation and prevent the onset of asthma symptoms. For severe asthma cases, monoclonal antibodies are utilized. These medications target specific immune molecules involved in the inflammatory cascade of asthma. Monoclonal antibodies help control severe asthma symptoms and reduce the frequency of exacerbations, offering a targeted approach to treatment (Rosenthal & Burchum, 2021).
Slide 3 – Quick Relief Treatment Options for Asthma
Short-acting beta-agonists (SABAs) are crucial in asthma management as they provide quick relief during acute symptoms by rapidly relaxing the airway muscles and promoting bronchodilation. They are commonly used as rescue medications to alleviate sudden asthma attacks. Anticholinergics, often used in combination with SABAs, help relax the airway muscles further and improve bronchodilation (Rosenthal & Burchum, 2021). By blocking the action of acetylcholine, these medications reduce airway constriction and improve airflow.
Systemic corticosteroids play a vital role in controlling severe asthma exacerbations. These medications, typically prescribed for short periods, effectively reduce airway inflammation, improve lung function, and help manage acute episodes of asthma. Beta-agonist tablets are reserved for specific cases where immediate relief is required. They provide rapid bronchodilation and are typically used when other forms of medication or inhalers are not accessible or do not offer sufficient relief. Rescue inhalers, containing short-acting bronchodilators, offer a portable and convenient option for immediate symptom relief (Rosenthal & Burchum, 2021). They are designed to be used on the go and provide quick relief by delivering medication directly to the airways.
A personalized asthma action plan is an essential tool that empowers patients to manage their symptoms and treatment effectively. It provides clear instructions on medication usage, trigger avoidance, and steps to take during worsening symptoms or exacerbations (Rosenthal & Burchum, 2021). The asthma action plan helps patients recognize early warning signs, take appropriate actions, and maintain control over their condition.
Slide 4 – Stepwise Approach to Asthma Treatment and Management
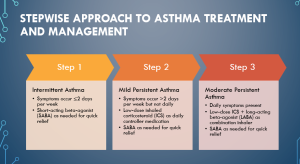
The stepwise approach to asthma treatment and management provides a structured framework for healthcare providers to tailor treatment based on the severity and frequency of symptoms experienced by patients.
Step 1 – Intermittent Asthma: At this stage, symptoms occur infrequently, with episodes happening two or fewer days per week. The recommended treatment is using a short-acting beta-agonist (SABA) as needed for quick relief. SABAs work by relaxing the airway muscles, providing immediate bronchodilation during asthma attacks. Since symptoms are sporadic, no daily controller medication is necessary at this stage (Rosenthal & Burchum, 2021).
Step 2 – Mild Persistent Asthma: In this stage, symptoms occur more frequently, happening more than two days per week, but not daily. The mainstay of treatment is a low-dose inhaled corticosteroid (ICS) as a daily controller medication. ICS reduces airway inflammation, helping to prevent symptoms and maintain asthma control. SABA is still used as needed for quick relief during exacerbations or when symptoms arise (Rosenthal & Burchum, 2021).
Step 3 – Moderate Persistent Asthma: At this stage, patients experience daily symptoms. Treatment involves a combination inhaler containing a low-dose ICS and a long-acting beta-agonist (LABA) for daily controller medication. The LABA provides additional bronchodilation and helps improve symptom control. SABA is still used as needed for quick relief during acute episodes.
Slide 5 – Asthma Treatment and Management Cont’
Step 4 – Severe Persistent Asthma: At this stage, patients experience symptoms throughout the day. The recommended treatment involves using a high-dose inhaled corticosteroid (ICS) in combination with a long-acting beta-agonist (LABA) as a daily controller medication. The combination inhaler provides potent anti-inflammatory effects and sustained bronchodilation to manage symptoms. In some cases, additional controllers like leukotriene modifiers or theophylline may be considered to further improve asthma control. SABA is still used as needed for quick relief during acute episodes (Papi et al., 2020).
Step 5 – Severe Persistent Asthma (Uncontrolled): In this stage, patients have daily symptoms and frequent exacerbations despite the use of high-dose ICS and LABA. Treatment involves a combination of high-dose ICS, LABA, and oral corticosteroids. Oral corticosteroids help to further control inflammation and manage severe symptoms. In addition, healthcare providers may consider additional therapies, such as monoclonal antibodies, which specifically target immune molecules involved in the inflammatory process of asthma. These medications are reserved for uncontrolled severe cases with standard therapies(Papi et al., 2020).
It is important to note that steps 4 and 5 of the asthma treatment plan are typically managed by asthma specialists or pulmonologists due to the complexity and severity of the condition. Regular monitoring, close follow-up, and ongoing adjustments to the treatment plan are necessary to achieve optimal asthma control and minimize the risk of complications.
Slide 6 – Stepwise Management in Asthma: Gaining and Maintaining Control
A tailored treatment approach based on individual needs, severity, and control level is essential in asthma management. Asthma is a heterogeneous condition, and patients may present with varying symptoms and levels of disease severity. By considering these factors, healthcare providers can customize treatment plans to address the specific needs of each patient (Bleecker et al., 2020). The gradual treatment intensification strategy plays a crucial role in asthma management.
Starting with the lowest effective dose of medications and then gradually increasing the treatment intensity helps minimize the risk of overtreatment and reduces the potential for side effects. This approach allows healthcare providers to find the optimal balance between symptom control and medication safety. Regular monitoring and assessment of symptoms, lung function, and exacerbation frequency are vital components of effective asthma management (Bleecker et al., 2020). By closely monitoring patients, healthcare providers can track their progress, identify any deterioration in control, and make necessary adjustments to the treatment plan. This proactive approach ensures timely interventions and reduces the risk of exacerbations.
Proactive prevention of exacerbations is another vital aspect of stepwise management. Treatment adjustments are made at each step to prevent and minimize the occurrence of asthma exacerbations. As patients progress through treatment, healthcare providers may modify medication dosages, add or remove specific medications, and consider additional therapies to achieve better control and prevent exacerbations. Patient empowerment and education are essential for successful asthma management. Educating patients about asthma, its triggers, and the importance of adhering to treatment plans empowers them to take an active role in their own care.
Patients can learn to recognize early warning signs of worsening asthma and promptly seek medical assistance. Empowered patients are more likely to adhere to prescribed medications, follow action plans, and engage in self-management strategies (Bleecker et al., 2020). The ultimate goal of stepwise management in asthma is achieving long-term disease control, reducing symptoms, and improving the overall quality of life for patients. With effective treatment adjustments, regular monitoring, patient education, and proactive prevention of exacerbations, healthcare providers can optimize asthma control and minimize the impact of the disease on patients’ daily lives.
References
Bleecker, E. R., Menzies-Gow, A. N., Price, D. B., Bourdin, A., Sweet, S., Martin, A. L., & Tran, T. N. (2020). Systematic literature review of systemic corticosteroid use for asthma management. American Journal of Respiratory and Critical Care Medicine, 201(3), 276-293. https://doi.org/10.1164/rccm.201904-0903SO
Papi, A., Blasi, F., Canonica, G. W., Morandi, L., Richeldi, L., & Rossi, A. (2020). Treatment strategies for asthma: Reshaping the concept of asthma management. Allergy, Asthma & Clinical Immunology, 16, 1-11. https://doi.org/10.1186/s13223-020-00472-8
Rosenthal, L. D., & Burchum, J. R. (2021). Lehne’s pharmacotherapeutics for advanced practice nurses and physician assistants (2nd ed.) St. Louis, MO: Elsevier.
NURS 6521 Week 3 EmmaGarcia Asthma and Stepwise Management Instructions
INTRODUCTION
Asthma and chronic obstructive pulmonary disease (COPD) are significant public health burdens. Currently, more than 25 million people in the United States have asthma (HealthyPeople.gov, 2019). As an advanced practice nurse, you will likely encounter patients who will present with respiratory disorders, including asthma or COPD. Understanding specific treatment protocols as well as the types of pharmacotherapeutics used to treat respiratory disorders is important to ensure the effective and safe delivery of advanced nursing practice.
This week, you will evaluate drug therapy plans for patients who present with asthma and analyze the stepwise approach to asthma treatment and management from a patient in your professional practice.
Reference: HealthyPeople.gov. (2019). Respiratory diseases. Retrieved from https://www.healthypeople.gov/2020/topics-objectives/topic/respiratory-diseasesLinks to an external site.
LEARNING OBJECTIVES
Students will:
- Evaluate drug therapy plans for asthma
- Assess the impact of asthma treatments on patients
- Analyze the stepwise approach to asthma treatment and management
ASTHMA AND STEPWISE MANAGEMENT
Asthma is a respiratory disorder that affects children and adults. Advanced practice nurses often provide treatment to patients with these disorders. Sometimes patients require immediate treatment, making it essential that you recognize and distinguish minor asthma symptoms from serious, life-threatening ones. Since symptoms and attacks are often induced by a trigger, advanced practice nurses must also help patients identify their triggers and recommend appropriate management options. Like many other disorders, there are various approaches to treating and managing care for asthmatic patients depending on individual patient factors.
One method that supports the clinical decision making of drug therapy plans for asthmatic patients is the stepwise approach, which you explore in this Assignment.
RESOURCES
Be sure to review the Learning Resources before completing this activity.
Click the weekly resources link to access the resources.
WEEKLY RESOURCES
To Prepare:
- Reflect on drugs used to treat asthmatic patients, including long-term control and quick relief treatment options for patients. Think about the impact these drugs might have on patients, including adults and children.
- Consider how you might apply the stepwise approach to address the health needs of a patient in your practice.
- Reflect on how stepwise management assists health care providers and patients in gaining and maintaining control of the disease.
BY DAY 7 OF WEEK 3
Create a 5- to 6-slide PowerPoint presentation that can be used in a staff development meeting on presenting different approaches for implementing the stepwise approach for asthma treatment. Be sure to address the following:
- Describe long-term control and quick relief treatment options for the asthma patient from your practice as well as the impact these drugs might have on your patient.
- Explain the stepwise approach to asthma treatment and management for your patient.
- Explain how stepwise management assists health care providers and patients in gaining and maintaining control of the disease. Be specific.
SUBMISSION INFORMATION
Before submitting your final assignment, you can check your draft for authenticity. To check your draft, access the Turnitin Drafts from the Start Here area.
- To submit your completed assignment, save your Assignment as WK3Assgn_LastName_Firstinitial
- Then, click on Start Assignment near the top of the page.
- Next, click on Upload File and select Submit Assignment for review.
LEARNING RESOURCES
Required Readings
- Rosenthal, L. D., & Burchum, J. R. (2021). Lehne’s pharmacotherapeutics for advanced practice nurses and physician assistants(2nd ed.) St. Louis, MO: Elsevier.
- Chapter 62, “Drugs for Asthma and Chronic Obstructive Pulmonary Disease” (pp. 557–579)
- Chapter 63, “Drugs for Allergic Rhinitis, Cough, and Colds” (pp. 580–588)
- Document:APA Presentation TemplateDownload APA Presentation Template
Required Media
- Speed Pharmacology. (2020). Drugs for asthma and COPD (Made Easy)Links to an external site.[Video]. https://www.youtube.com/watch?v=-DVZ9pl0rGY
Note: This media program is approximately 14 minutes.
- Speed Pharmacology. (2017). Antihistamines (Made Easy)Links to an external site.[Video]. https://www.youtube.com/watch?v=D5PHANcdA_E&t=25s
Note: This media program is approximately 10 minutes.
Optional Resources
- National Heart Lung and Blood Institute. (2007). Expert panel report 3 (EPR3): Guidelines for the diagnosis and management of asthmaLinks to an external site.. Retrieved from http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm
This web resource presents guidelines for diagnosing and managing asthma and outlines treatment recommendations for specific age groups.
NURS_6521_Week3_Assignment_Rubric
Criteria
Ratings
Pts
This criterion is linked to a Learning Outcome Describe the long-term control and quick relief treatment options for the asthma patient from your practice, as well as the impact these drugs might have on your patient.
30 to >26.7 pts
Excellent
The presentation clearly and accurately describes in detail the long-term control and quick relief treatment options for the asthma patient from their practice. … The presentation clearly and accurately describes in detail the impact these drugs might have on their patient.
26.7 to >23.7 pts
Good
The presentation accurately describes the long-term control and quick relief options for the asthma patient from their practice. … The presentation accurately describes the impact these drugs might have on their patient.
23.7 to >20.7 pts
Fair
The presentation inaccurately or vaguely describes the long-term control and quick relief options for the asthma patient from their practice. … The presentation inaccurately or vaguely describes the impact these drugs might have on their patient.
20.7 to >0 pts
Poor
The presentation inaccurately and vaguely describes the long-term and quick relief options for the asthma patient from their practice, or is missing. … The presentation inaccurately and vaguely describes the impact these drugs might have on their patient, or is missing.
30 pts
This criterion is linked to a Learning OutcomeExplain the stepwise approach to asthma treatment and management for your patient.
30 to >26.7 pts
Excellent
The presentation clearly and accurately explains in detail the stepwise approach to asthma treatment and management for their patient.
26.7 to >23.7 pts
Good
The presentation accurately explains the stepwise approach to asthma treatment and management for their patient.
23.7 to >20.7 pts
Fair
The presentation inaccurately or vaguely explains the stepwise approach to asthma treatment and management for their patient.
20.7 to >0 pts
Poor
The presentation inaccurately and vaguely explains the stepwise approach to asthma treatment and management for their patient.
30 pts
This criterion is linked to a Learning OutcomeExplain how stepwise management assists health care providers and patients in gaining and maintaining control of the disease. Be specific.
30 to >26.7 pts
Excellent
The presentation clearly and accurately explains in detail how stepwise management assists health care providers and patients in gaining and maintaining control of the disease. … The presentation provides accurate and detailed examples to support the explanation provided.
26.7 to >23.7 pts
Good
The presentation accurately explains how stepwise management assists health care providers and patients in gaining and maintaining control of the disease. … The presentation provides accurate examples to support the explanation provided.
23.7 to >20.7 pts
Fair
The presentation inaccurately or vaguely explains how stepwise management assists health care providers and patients in gaining and maintaining control of the disease. … The presentation provides inaccurate or vague examples to support the explanation provided.
20.7 to >0 pts
Poor
The presentation inaccurately and vaguely explains how stepwise management assists health care providers and patients in gaining and maintaining control of the disease, or is missing. … The presentation provides inaccurate and vague examples to support the explanation provided, or is missing.
30 pts
This criterion is linked to a Learning OutcomeWritten Expression and Formatting – Paragraph Development and Organization: Paragraphs make clear points that support well developed ideas, flow logically, and demonstrate continuity of ideas. Sentences are carefully focused–neither long and rambling nor short and lacking substance.
5 to >4.45 pts
Excellent
Paragraphs and sentences follow writing standards for flow, continuity, and clarity.
4.45 to >3.95 pts
Good
Paragraphs and sentences follow writing standards for flow, continuity, and clarity 80% of the time.
3.95 to >3.45 pts
Fair
Paragraphs and sentences follow writing standards for flow, continuity, and clarity 60%–79% of the time.
3.45 to >0 pts
Poor
Paragraphs and sentences follow writing standards for flow, continuity, and clarity less than 60% of the time.
5 pts
This criterion is linked to a Learning OutcomeWritten Expression and Formatting – English writing standards: Correct grammar, mechanics, and proper punctuation
5 to >4.45 pts
Excellent
Uses correct grammar, spelling, and punctuation with no errors
4.45 to >3.95 pts
Good
Contains a few (1–2) grammar, spelling, and punctuation errors
3.95 to >3.45 pts
Fair
Contains several (3–4) grammar, spelling, and punctuation errors
3.45 to >0 pts
Poor
Contains many (? 5) grammar, spelling, and punctuation errors that interfere with the reader’s understanding
5 pts
Total Points: 100
PreviousNext
NURS 6521 Module 3: Gastrointestinal and Hepatobiliary Systems
Week 4: Gastrointestinal and Hepatobiliary Disorders
INTRODUCTION
As an advanced practice nurse, you will likely encounter patients who will present with symptoms affecting the gastrointestinal (GI) tract. Of special note, is the consideration that most symptoms concerning the GI tract are non-specific and therefore, diagnosing diagnoses of the GI tract require thoughtful and careful investigation. Similarly, hepatobiliary disorders may also mirror many of the signs and symptoms that patients present when suffering from GI disorders.
How might you tease out the specific signs and symptoms between these potential disorders and body systems? What drug therapy plans will best address these disorders for your patients?
This week, you examine GI and hepatobiliary disorders. You will review a patient case study and consider those factors in recommending and prescribing a drug therapy plan for your patient.
LEARNING OBJECTIVES
Students will:
- Evaluate diagnoses for patients with gastrointestinal and hepatobiliary disorders
- Justify drug therapy plans based on patient history and diagnosis
PHARMACOTHERAPY FOR GASTROINTESTINAL AND HEPATOBILIARY DISORDERS
Gastrointestinal (GI) and hepatobiliary disorders affect the structure and function of the GI tract. Many of these disorders often have similar symptoms, such as abdominal pain, cramping, constipation, nausea, bloating, and fatigue. Since multiple disorders can be tied to the same symptoms, it is important for advanced practice nurses to carefully evaluate patients and prescribe a treatment that targets the cause rather than the symptom.
Once the underlying cause is identified, an appropriate drug therapy plan can be recommended based on medical history and individual patient factors. In this Assignment, you examine a case study of a patient who presents with symptoms of a possible GI/hepatobiliary disorder, and you design an appropriate drug therapy plan.
RESOURCES
Be sure to review the Learning Resources before completing this activity.
Click the weekly resources link to access the resources.
WEEKLY RESOURCES
To Prepare:
- Review the case study assigned by your Instructor for this Assignment
- Reflect on the patient’s symptoms, medical history, and drugs currently prescribed.
- Think about a possible diagnosis for the patient. Consider whether the patient has a disorder related to the gastrointestinal and hepatobiliary system or whether the symptoms are the result of a disorder from another system or other factors, such as pregnancy, drugs, or a psychological disorder.
- Consider an appropriate drug therapy plan based on the patient’s history, diagnosis, and drugs currently prescribed.
BY DAY 7 OF WEEK 4
Write a 1-page paper that addresses the following:
- Explain your diagnosis for the patient, including your rationale for the diagnosis.
- Describe an appropriate drug therapy plan based on the patient’s history, diagnosis, and drugs currently prescribed.
- Justify why you would recommend this drug therapy plan for this patient. Be specific and provide examples.
Reminder: The College of Nursing requires that all papers submitted include a title page, introduction, summary, and references. The Sample Paper provided at the Walden Writing Center offers an example of those required elements (available at http://writingcenter.waldenu.edu/57.htmLinks to an external site.). All papers submitted must use this formatting.
LEARNING RESOURCES
Required Readings
- Rosenthal, L. D., & Burchum, J. R. (2021). Lehne’s pharmacotherapeutics for advanced practice nurses and physician assistants(2nd ed.) St. Louis, MO: Elsevier.
- Chapter 64, “Drugs for Peptic Ulcer Disease” (pp. 589–597)
- Chapter 65, “Laxatives” (pp. 598–604)
- Chapter 66, “Other Gastrointestinal Drugs” (pp. 605–616)
- Chapter 80, “Antiviral Agents I: Drugs for Non-HIV Viral Infections” (pp. 723–743)
- Chalasani, N., Younossi, Z., Lavine, J. E., Charlton, M., Cusi, K., Rinella, M., . . . Sanya, A. J. (2018). The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology, 67(1), 328–357. Retrieved from https://aasldpubs.onlinelibrary.wiley.com/doi/pdf/10.1002/hep.29367
This article details the diagnosis and management of nonalcoholic fatty liver disease. Review this article to gain an understanding of the underlying pathophysiology as well as the suggested pharmacotherapeutics that might be recommended to treat this disorder.
Week 4 Case Study
Nathan SW
Hi everyone-
I hope everyone had a good week! This week we will be looking at GI disorders. We have a paper that will be due.
Please use the following case for your assignment:
DC is a 46-year-old female who presents with a 24-hour history of RUQ pain. She states the pain started about 1 hour after a large dinner she had with her family. She has had nausea and on instance of vomiting before presentation.
PMH:Vitals:HTNTemp: 98.8oFType II DMWt: 202 lbsGoutHt: 5’8”DVT – Caused by oral BCPsBP: 136/82 HR: 82 bpmCurrent Medications:Notable Labs:Lisinopril 10 mg dailyWBC: 13,000/mm3HCTZ 25 mg dailyTotal bilirubin: 0.8 mg/dLAllopurinol 100 mg dailyDirect bilirubin: 0.6 mg/dLMultivitamin dailyAlk Phos: 100 U/L AST: 45 U/L ALT: 30 U/LAllergies:
- Latex
- Codeine
- Amoxicillin
PE:
- Eyes: EOMI
- HENT: Normal
- GI:bNondistended, minimal tenderness
- Skin:bWarm and dry
- Neuro: Alert and Oriented
- Psych:bAppropriate mood
NURS_6521_Week4_Assignment_Rubric
Criteria
Ratings
Pts
This criterion is linked to a Learning OutcomeExplain your diagnosis for the patient, including your rationale for the diagnosis.
25 to >22.25 pts
Excellent
The response accurately and clearly explains in detail the diagnosis for the patient, including an accurate and thorough rationale for the diagnosis that supports clinical judgment.
22.25 to >19.75 pts
Good
The response provides a basic explanation of 1-2 diagnoses for the patient, including an accurate rationale for the diagnosis that may support clinical judgment.
19.75 to >17.25 pts
Fair
The response inaccurately or vaguely explains the diagnosis for the patient, including an inaccurate or vague rationale for the diagnosis that may or may not support clinical judgment.
17.25 to >0 pts
Poor
The response inaccurately and vaguely explains the diagnosis for the patient, including an inaccurate and vague rationale for the diagnosis that does not support clinical judgment, or is missing.
25 pts
This criterion is linked to a Learning OutcomeDescribe an appropriate drug therapy plan based on the patient’s history, diagnosis, and drugs currently prescribed.
30 to >26.7 pts
Excellent
The response accurately and completely describes in detail an appropriate drug therapy plan based on the patient’s history, diagnosis, and drugs currently prescribed.
26.7 to >23.7 pts
Good
The response describes a basic explanation of the appropriate drug therapy plan based on the patient’s history, diagnosis, and drugs currently prescribed.
23.7 to >20.7 pts
Fair
The response inaccurately or vaguely describes an appropriate drug therapy plan based on the patient’s history, diagnosis, and drugs currently prescribed.
20.7 to >0 pts
Poor
The response inaccurately and vaguely describes an appropriate drug therapy plan based on the patient’s history, diagnosis, and drugs currently prescribed.
30 pts
This criterion is linked to a Learning OutcomeJustify why you would recommend this drug therapy plan for this patient. Be specific and provide examples.
30 to >26.7 pts
Excellent
The response provides an accurate, clear, and detailed justification for the recommended drug therapy plan for this patient. … The response includes specific, accurate, and detailed examples that fully support the justification provided.
26.7 to >23.7 pts
Good
The response provides a basic justification for the recommended drug therapy plan for this patient. … The response includes only 1-2 examples that fully support the justification provided.
23.7 to >20.7 pts
Fair
The response provides an inaccurate or vague justification for the recommended drug therapy plan for this patient. … The response may include examples, which may inaccurately or vaguely support the justification provided.
20.7 to >0 pts
Poor
The response provides an inaccurate and vague justification for the recommended drug therapy plan for this patient, or is missing. … The response does not include examples that support the justification provided, or is missing.
30 pts
This criterion is linked to a Learning OutcomeWritten Expression and Formatting – Paragraph Development and Organization: Paragraphs make clear points that support well developed ideas, flow logically, and demonstrate continuity of ideas. Sentences are carefully focused–neither long and rambling nor short and lacking substance.
5 to >4.45 pts
Excellent
Paragraphs and sentences follow writing standards for flow, continuity, and clarity.
4.45 to >3.95 pts
Good
Paragraphs and sentences follow writing standards for flo
READ MORE >>
NURS 6521 Week 4 EmmaGarcia Pharmacotherapy For Gastrointestinal And Hepatobilia ...
NURS 6521 Week 4 EmmaGarcia Pharmacotherapy For Gastrointestinal And Hepatobiliary Disorders Example
Week 4 Case Study
Nathan SW
Hi everyone-
I hope everyone had a good week! This week we will be looking at GI disorders. We have a paper that will be due.
Please use the following case for your assignment:
DC is a 46-year-old female who presents with a 24-hour history of RUQ pain. She states the pain started about 1 hour after a large dinner she had with her family. She has had nausea and on instance of vomiting before presentation.
PMH:Vitals:HTNTemp: 98.8oFType II DMWt: 202 lbsGoutHt: 5’8”DVT – Caused by oral BCPsBP: 136/82HR: 82 bpmCurrent Medications:Notable Labs:Lisinopril 10 mg dailyWBC: 13,000/mm3HCTZ 25 mg dailyTotal bilirubin: 0.8 mg/dLAllopurinol 100 mg dailyDirect bilirubin: 0.6 mg/dLMultivitamin dailyAlk Phos: 100 U/LAST: 45 U/LALT: 30 U/LAllergies:
- Latex
- Codeine
- Amoxicillin
PE:
- Eyes: EOMI
- HENT: Normal
- GI:bNondistended, minimal tenderness
- Skin:bWarm and dry
- Neuro: Alert and Oriented
- Psych:bAppropriate mood
Pharmacotherapy for Gastrointestinal and Hepatobiliary Disorders
Based on the provided case study, the patient, DC, appears to be presenting with acute cholecystitis. The sudden onset of the right upper quadrant (RUQ) pain occurring approximately one hour after a large dinner is indicative of gallbladder inflammation. The gallbladder is located in the RUQ, and cholecystitis often manifests as sharp or colicky pain in this region (Rosenthal & Burchum, 2021). Additionally, DC reports experiencing nausea and vomiting, which are common symptoms associated with cholecystitis, particularly when biliary colic occurs due to gallstone obstruction.
DC possesses several risk factors that further support the diagnosis of acute cholecystitis. Being a 46-year-old female, she is more prone to gallbladder-related issues. Her weight of 202 lbs and height of 5’8? indicate obesity, which is associated with an increased risk of gallstone formation. Furthermore, her medical history reveals a diagnosis of hypertension, type II diabetes mellitus (DM), and a previous deep vein thrombosis (DVT) caused by oral contraceptive pills (BCPs). While the latter is unrelated to the current symptoms, hypertension and type II DM can contribute to the overall clinical picture.
Considering the diagnosis of acute cholecystitis, an appropriate drug therapy plan for DC would involve pain management, administration of antibiotics, and symptom relief. Pain can be managed using nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen. However, due to DC’s comorbidities of hypertension and type II DM, acetaminophen may be a safer choice, as it does not significantly affect blood pressure or glucose levels. Conversely, NSAIDs can potentially interfere with antihypertensive medications and have adverse effects on blood pressure.
The next aspect of the drug therapy plan involves antibiotic treatment. Acute cholecystitis involves inflammation and infection of the gallbladder (Gallaher & Charles, 2022). Therefore, an appropriate antibiotic regimen should be prescribed. A combination of a third-generation cephalosporin, such as ceftriaxone, and metronidazole would be suitable. This combination provides broad-spectrum coverage against gram-negative organisms commonly found in biliary infections and anaerobic bacteria. Additionally, symptom relief for DC’s nausea and vomiting can be achieved through the use of antiemetics. Ondansetron, a well-tolerated antiemetic, can be considered to alleviate these symptoms and improve the patient’s overall comfort.
References
Gallaher, J. R., & Charles, A. (2022). Acute cholecystitis: A review. JAMA, 327(10), 965-975. https://doi.org/10.1001/jama.2022.2350
Rosenthal, L. D., & Burchum, J. R. (2021). Lehne’s pharmacotherapeutics for advanced practice nurses and physician assistants (2nd ed.) St. Louis, MO: Elsevier.
Case Study: Gastroenteritis
HL is a patient who presents with nausea, vomiting, and diarrhea with a history of drug abuse and possible Hepatitis C. This paper aims to highlight the differential diagnosis based on the patient’s presenting complaint, describe the recommended drug therapy, and justify its use for this patient.
Differential Diagnoses
The primary diagnosis is gastroenteritis. Differential diagnoses include food poisoning and bowel obstruction. Gastroenteritis is a viral, bacterial, or parasitic infection of the intestines that presents with the above presentation in addition to abdominal pain and is highly contagious (Maslennikov et al., 2021). The main causative agents are viruses, including noroviruses and rotavirus, transmitted through ingestion or coming into contact with contaminated food and water. Using prednisone, which suppresses the immune system, means an increased predisposition to infections. In addition to the patient’s presenting complaint, this means that gastroenteritis is the primary diagnosis.
Drug Therapy Plan
Gastroenteritis is often self-limiting, and the patient is encouraged to stay hydrated and rest. In this patient, I would recommend antiemetic drugs such as ondansetron (Riddle, 2018). In addition, I would recommend loperamide or bismuth subsalicylate. After finding out the reason for the use of prednisone, I would slowly taper off the drug and eventually discontinue it. The patient can continue using both Synthroid and nifedipine.
Justification For Drug Therapy
Antiemetics are critical in minimizing vomiting and consequent fluid loss. Ondansetron is my preferred drug of choice due to its limited sedative properties compared to other antiemetics, such as promethazine (Rosenthal & Burchum, 2021). Antidiarrheals such as loperamide and bismuth subsalicylate help address diarrhea, significantly contributing to fluid loss. Tapering off the prednisone and eventually discontinuing it is crucial in this patient. Corticosteroids such as prednisone, when used over long durations of time, significantly impact the liver. These drugs often increase the risk of developing or worsening nonalcoholic fatty liver disease. This is particularly risky in this patient with possible hepatitis C. Nifedipine and Synthroid have minimal to no impact on the liver and can be continued.
Conclusion
The patient’s presenting complaints paint a picture of gastroenteritis. Despite the condition being mostly self-limiting, prescribing antiemetics and antidiarrheals is important to minimize fluid loss. Discontinuing drugs such as prednisone, which have a significant impact on the liver in such a patient, is essential to minimize the risk of nonalcoholic fatty liver disease.
NURS 6521 Week 4 EmmaGarcia Pharmacotherapy For Gastrointestinal And Hepatobiliary Disorders References
Maslennikov, R., Poluektova, E., Ivashkin, V., & Svistunov, A. (2021). Diarrhea in adults with coronavirus disease-beyond incidence and mortality: a systematic review and meta-analysis. Infectious Diseases (London, England), 53(5), 348–360. https://doi.org/10.1080/23744235.2021.1885733
Riddle M. S. (2018). Current management of acute diarrheal infections in adults. Polish Archives Of Internal Medicine, 128(11), 685–692. https://doi.org/10.20452/pamw.4363
Rosenthal, L. D., & Burchum, J. R. (2021). Lehne’s pharmacotherapeutics for advanced practice nurses and physician assistants (2nd ed.). St. Louis, MO: Elsevier.
Also Read: NURS 6521 Week 3 EmmaGarcia Asthma and Stepwise Management
READ MORE >>
