Our Previous Samples
NRNP 6645 Week 6 Supportive and Interpersonal PsychotherapyNRNP 6645 Week 6 Supp ...
NRNP 6645 Week 6 Supportive and Interpersonal Psychotherapy
NRNP 6645 Week 6 Supportive and Interpersonal Psychotherapy
Amelia, a 16-year-old high school sophomore, presents with symptoms of weight loss and a very obvious concern for her weight. She has made several references to being “fat” and “pudgy” when, in fact, she is noticeably underweight. Her mother reports that Amelia is quite regimented in her eating and that she insists on preparing her own meals, as her mother “puts too many fattening things in the food” that she cooks.
After discovering that during the past 3 months Amelia has lost 15 pounds and is well under body weight for someone of similar age/sex/developmental trajectory, the psychiatric-mental health nurse practitioner diagnosed Amelia with anorexia nervosa.
Evidence-based research shows that clients like Amelia may respond well to supportive psychotherapy and interpersonal psychotherapy. So which approach might you select? Are both equally effective for all clients? In practice, you will find that many clients may be candidates for both of these therapeutic approaches, but factors such as a client’s psychodynamics and your own skill set as a therapist may impact their effectiveness.
This week, you continue exploring therapeutic approaches and their appropriateness for clients, focusing on supportive psychotherapy and interpersonal psychotherapy.
NRNP 6645 Week 6 Supportive and Interpersonal Psychotherapy Learning Objectives
Students will:
- Assess knowledge of concepts, principles, and theories related to psychotherapy with individuals, families, and groups
NRNP 6645 Week 6 Supportive and Interpersonal Psychotherapy Learning Resources
- Required Readings (click to expand/reduce)
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.)
Nichols, M., & Davis, S. D. (2020). The essentials of family therapy (7th ed.). Pearson.
- Chapter 5, “Strategic Family Therapy”
- Chapter 11, “Solution-Focused Therapy”
- Chapter 12, “Narrative Therapy”
Wheeler, K. (Ed.). (2020). Psychotherapy for the advanced practice psychiatric nurse: A how-to guide for evidence-based practice (3rd ed.). Springer Publishing.
- Chapter 3, “Assessment and Diagnosis” (pp. 123–134 only)
- Chapter 5, “Supportive and Psychodynamic Psychotherapy”
- Review the sections on supportive psychotherapy only.
- Chapter 10, “Interpersonal Psychotherapy”
- Chapter 21, “Psychotherapeutic Approaches with Children and Adolescents” (p. 781 only)
U.S. Department of Health & Human Services. (n.d.). HIPAA privacy rule and sharing information related to mental health. http://www.hhs.gov/hipaa/for-professionals/special-topics/mental-health/
Credit: U.S. Department of Health and Human Services/Office for Civil Rights. (n.d.). HIPAA Privacy Rule and Sharing Information Related to Mental Health. HHS.gov. https://www.hhs.gov/sites/default/files/hipaa-privacy-rule-and-sharing-info-related-to-mental-health.pdf
- NRNP 6645 Week 6 Supportive and Interpersonal Psychotherapy Required Media (click to expand/reduce)
IPT Institute. (2015, April 16). IPT Institute lecture demonstration Scott Stuart [Video]. YouTube. https://www.youtube.com/watch?v=TmQYhLiDRE0
MindbyMind. (2016, December 8). Elements of supportive psychotherapy for high impact clinic visits – Episode 2 [Video]. YouTube. https://www.youtube.com/watch?v=i8kj5blYiJk&t=4s
NRNP 6645 Week 6 Supportive and Interpersonal Psychotherapy Optional Resource
Sommers-Flanagan, J., & Sommers-Flanagan, R. (2013). Counseling and psychotherapy theories in context and practice [Video]. https://waldenu.kanopy.com/video/counseling-and-psychotherapy-theories-contex
- Existential Therapy (starts at 58 minutes)
Exam : Midterm Exam – NRNP 6645 Week 6 Supportive and Interpersonal Psychotherapy
This exam is a test of your knowledge in preparation for your certification exam. No outside resources—including books, notes, websites, or any other type of resource—are to be used to complete this exam. Prior to starting the exam, you should review all of your materials. You are expected to comply with Walden University’s Code of Conduct.
This exam will cover the following topics, which relate to psychotherapy with individuals, families, and groups:
- Biological basis of psychotherapy treatments
- Influences of culture, religion, and socioeconomics on personal perspectives of psychotherapy treatments
- Legal and ethical considerations among individual, family, and group modalities of therapy
- Family assessment
- Group therapy techniques
- Psychodynamic psychotherapy
- Cognitive-behavior psychotherapy
- Supportive and interpersonal psychotherapy
By Day 7
Complete the Midterm Exam. There is a 2-hour and 30-min time limit to complete this 100-question exam. You may only attempt the exam once.
Submission and Grading Information
Grading Criteria
To access your Exam:
Week 6 Midterm Exam
WEEK 7 ASSIGNMENT – COMPARING HUMANISTIC-EXISTENTIAL PSYCHOTHERAPY WITH OTHER APPROACHES
Understanding the strengths of each type of therapy and which type of therapy is most appropriate for each patient is an essential skill of the psychiatric-mental health nurse practitioner. In this Assignment, you will compare humanistic-existential therapy to another psychotherapeutic approach. You will identify the strengths and challenges of each approach and describe expected potential outcomes.
To prepare:
- Review the humanistic-existential psychotherapy videos in this week’s Learning Resources.
- Reflect on humanistic-existential psychotherapeutic approaches.
- Then, select another psychotherapeutic approach to compare with humanistic-existential psychotherapy. The approach you choose may be one you previously explored in the course or one you are familiar with and especially interested in.
In a 2- to 3-page paper, address the following:
- Briefly describe humanistic-existential psychotherapy and the second approach you selected.
- Explain at least three differences between these therapies. Include how these differences might impact your practice as a PMHNP.
- Focusing on one video you viewed, explain why humanistic-existential psychotherapy was utilized with the patient in the video and why it was the treatment of choice. Describe the expected potential outcome if the second approach had been used with the patient.
- Support your response with specific examples from this week’s media and at least three peer-reviewed, evidence-based sources. Explain why each of your supporting sources is considered scholarly. Attach the PDFs of your sources.
Comparing Humanistic-Existential Therapy with Other Approaches Example
Psychosocial interventions are vital therapeutic options for a variety of psychiatric illnesses that may be employed alone or in conjunction with pharmacologic agents. Humanistic-existential psychotherapy is a sort of psychosocial intervention that helps patients gain transcendental abilities over their situations. Humanistic-existential therapy promotes comprehension of the human experience rather than symptoms and aims to increase client self-awareness and self-understanding (Schneider, 2019). The goal of this paper is to present an overview of humanistic-existential therapy, followed by a discussion of its differences from cognitive behavioral therapy (CBT), which is also a widespread psychotherapy intervention used in the treatment of mood, anxiety, and psychotic diseases. Furthermore, with reference to a video of a therapy session in progress, the discussion explains why humanistic-existential therapy was chosen as the treatment of choice.
Overview of Humanistic-Existential Psychotherapy and Cognitive Behavioral Therapy
Humanistic-existential therapy is based on a compassionate relationship with patients and focuses on the client’s individual experiences rather than the symptoms. The treatment emphasizes unconditional positive regard as a humanistic value, while freedom and responsibility are stressed as existential virtues (Schneider, 2019). The central constructs of humanistic therapy, of which person-centered therapy is a paragon, include self-actualizing tendency (be all that you can be), self and ideal self, conditions of worth, and relational transparency, in which genuineness, empathy, acceptance, and caring form the therapeutic approach (Grande, 2016).
The therapist focuses on the client and provides a comfortable setting for positive growth while conducting treatment. In addition, the therapist encourages the client to be open and honest while expressing himself/herself. The therapy session is based on the client’s set objectives. Thus, the name patient-centered therapy, and it also fosters the client’s independence in terms of decision-making (Grande, 2016). The core constructs of existential therapy are phenomenology, ultimate concerns, and defenses.
Phenomenology refers to the client’s direct or immediate experiences. In contrast, the ultimate concerns are the thoughts that trigger anxiety, such as death, isolation, meaninglessness, and the desperate need to acquire freedom, which creates anxiety and the necessity to act. Defenses are acts that a person does to avoid anxiety. As a result, the treatment embraces worry as a positive force that aids in the achievement of objectives.
CBT is a form of psychotherapy that stresses the significance of thoughts and perception in shaping thoughts and behaviors. People suffering from psychosis, mood, or anxiety disorders may have unpleasant thoughts and perceptions that are harmful to them or others in their immediate surroundings. As a result, CBT employs a problem-solving approach to educate individuals on how to modify their thinking and control their emotions in stressful circumstances (Chand et al., 2022). CBT is extremely educational and employs assignments, homework, and experimenting with new ways of behaving and responding to identities to transform inaccurate or unrealistic ways of thinking, which in turn influences emotions and actions.
The Differences Between Humanistic-Existential Therapy and CBT
The first distinction is that although humanistic-existential treatment emphasizes the relevance of the client’s self-awareness and self-understanding, CBT is based on behavioral traditions. Patient-centered therapy, a type of humanistic-existential therapy, for example, creates an environment in which the therapist forms a therapeutic alliance with the patient, encourages freedom of choice and the potential for meaningful change, and allows therapy to proceed based on the patient’s expectations and goals (Heidenreich et al., 2021). When dealing with individuals suffering from drug addiction problems, for example, promoting their independence and self-awareness may be the first step toward avoiding substance usage.
Conversely, CBT focuses on tactics for changing a person’s negative beliefs, which ultimately influence their actions and behaviors. The second distinction is the length of treatment. Humanistic-existential therapy may be utilized for short-term treatment of drug misuse problems, but if a lifetime journey and development are necessary, the therapy may be everlasting. On the other hand, CBT requires a short course of 5-20 sessions lasting 30-60 minutes and taking place once a week or every two weeks (Heidenreich et al., 2021).
The third distinction is that, whereas a therapist’s role in humanistic-existential therapy is to create a positive environment in which a client can develop self-awareness and understanding, a therapist’s role in CBT includes developing client-oriented activities to help shape the client’s thoughts and behaviors (Heidenreich et al., 2021). Understanding the contrasts between the two psychotherapeutic treatments allows a psychiatric mental health nurse practitioner to justify therapy selection when treating a variety of mental health disorders.
Why Humanistic-Existential Therapy was the Treatment of Choice in the Video
Joe is a fictitious name given to the patient being discussed. James Bugental is in a session with a female interviewee, perhaps Joe’s mother. According to the extract, Joe feels “not being alive” and is constricted in his existence. He started treatment two years ago, and his mother believes he needs further help with his illness, which is not indicated in the video excerpt. Humanistic-existential therapy was selected as the treatment of choice to help the patient comprehend his problem better. The treatment would allow the patient to gain self-awareness and self-understanding, rescuing him from a hazy state of mind that he characterizes as “not being alive” and feeling constrained. If CBT had been available, the patient may have formed a positive attitude about his life, which could have led to actions and behaviors that made him feel better.
Conclusion
Humanistic-existential therapy shows promise in the treatment of individuals who have a poor understanding of their ailments and situations. The therapy aims to increase patients’ self-awareness and self-understanding, which will eventually improve their recovery. As a result, humanistic-existential therapists concentrate on making the setting pleasant for patients, promoting their independence, and tailoring the therapy to the patient’s needs and preferences. CBT, in addition to humanistic-existential therapy, is widely utilized in the treatment of mood and anxiety disorders. While the remedies are founded on distinct ideas, when utilized effectively and rationally, they both promote patient recovery from mental health disorders.
References
Chand, S. P., Kuckel, D. P., & Huecker, M. R. (2022). Cognitive Behavior Therapy. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK470241/
Grande, T. (2016, January 9). Theories of counseling – Existential Therapy. https://youtu.be/YvAvc2aWup0
Heidenreich, T., Noyon, A., Worrell, M., & Menzies, R. (2021). Existential approaches and cognitive behavior therapy: Challenges and potential. International Journal of Cognitive Therapy, 14(1), 209–234. https://doi.org/10.1007/s41811-020-00096-1
Schneider, K. J. (2019). Existential-humanistic and existential-integrative therapy: Philosophy and theory. In The Wiley World Handbook of Existential Therapy (pp. 247–256). John Wiley & Sons, Ltd. https://doi.org/10.1002/9781119167198.ch14
Also Read: NRNP 6645 Week 4 Exploring Psychodynamic Theories
READ MORE >>
NRNP 6645 Week 8 Assignment Psychotherapy for Clients With Addictive DisordersNR ...
NRNP 6645 Week 8 Assignment Psychotherapy for Clients With Addictive Disorders
NRNP 6645 Week 8 Assignment Psychotherapy for Clients With Addictive Disorders
A long-standing debate has roiled over whether addicts have a choice over their behaviors. The disease creates distortions in thinking, feelings, and perceptions, which drive people to behave in ways that are not understandable to others around them. Simply put, addiction is not a choice. Addictive behaviors are a manifestation of the disease, not a cause.
—Dr. Raju Hajela, former president of the Canadian Society of Addiction Medicine
A common misconception is that addiction is a choice, and addicts are often labeled as individuals who lack morals, willpower, or responsibility. However, addiction is a clinical disorder that must be treated with the support of a health care professional. Although many people who are exposed to potentially addictive substances and behaviors continue life unaltered by their experiences, some people are fueled by these experiences and spiral out of control.
In your role as the psychiatric-mental health nurse practitioner, you must be prepared to not only work with these individuals who struggle with addiction but also help them and their families overcome the social stigmas associated with addictive behavior.
This week, you will assess a research article on psychotherapy for clients with addictive disorders. You also examine therapies for treating these clients and consider potential outcomes. Finally, you will discuss how therapy treatment will translate into your clinical practice.
NRNP 6645 Week 8 Assignment Psychotherapy for Clients With Addictive Disorders
Learning Objectives
Students will:
- Analyze literature on interventions and therapeutic approaches used for treating clients with addictive disorders
- Evaluate the application of current literature on addiction treatment to clinical practice
NRNP 6645 Week 8 Assignment Psychotherapy for Clients With Addictive Disorders Learning Resources
- Required Readings (click to expand/reduce)
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.)
- For reference as needed
Wheeler, K. (Ed.). (2020). Psychotherapy for the advanced practice psychiatric nurse: A how-to guide for evidence-based practice (3rd ed.). Springer Publishing.
- Chapter 9, “Motivational Interviewing”
- Chapter 19, “Psychotherapeutic Approaches for Addictions and Related Disorders”
- Required Media (click to expand/reduce)
AllCEUs Counseling Education. (2017, November 4). 187 models of treatment for addiction | Addiction counselor training series [Video]. YouTube. https://www.youtube.com/watch?v=eQkA0mIWx8A
Assignment: NRNP 6645 Week 8 Assignment Psychotherapy for Clients With Addictive Disorders
Addictive disorders can be particularly challenging for clients. Not only do these disorders typically interfere with a client’s ability to function in daily life, but they also often manifest as negative and sometimes criminal behaviors. Sometimes clients with addictive disorders also suffer from other mental health issues, creating even greater struggles for them to overcome.
In your role, you have the opportunity to help clients address their addictions and improve outcomes for both the clients and their families.
To prepare for NRNP 6645 Week 8 Assignment Psychotherapy for Clients With Addictive Disorders:
- Review this week’s Learning Resources and consider the insights they provide about diagnosing and treating addictive disorders. As you watch the 187 Models of Treatment for Addiction video, consider what treatment model you may use the most with clients presenting with addiction.
- Search the Walden Library databases and choose a research article that discusses a therapeutic approach for treating clients, families, or groups with addictive disorders.
NRNP 6645 Week 8 Assignment Psychotherapy for Clients With Addictive Disorders The Assignment
In a 5- to 10-slide PowerPoint presentation, address the following. Your title and references slides do not count toward the 5- to 10-slide limit.
- Provide an overview of the article you selected.
- What population (individual, group, or family) is under consideration?
- What was the specific intervention that was used? Is this a new intervention or one that was already studied?
- What were the author’s claims?
- Explain the findings/outcomes of the study in the article. Include whether this will translate into practice with your own clients. If so, how? If not, why?
- Explain whether the limitations of the study might impact your ability to use the findings/outcomes presented in the article.
- Use the Notes function of PowerPoint to craft presenter notes to expand upon the content of your slides.
- Support your response with at least three other peer-reviewed, evidence-based sources. Explain why each of your supporting sources is considered scholarly. Provide references to your sources on your last slide. Be sure to include the article you used as the basis for this Assignment.
By Day 7
Submit your Assignment. Also, attach and submit PDFs of the sources you used.
Submission and Grading Information
To submit your completed Assignment for review and grading, do the following:
- Please save your Assignment using the naming convention “WK8Assgn+last name+first initial.(extension)” as the name.
- Click the Week 8 Assignment Rubric to review the Grading Criteria for the Assignment.
- Click the Week 8 Assignment link. You will also be able to “View Rubric” for grading criteria from this area.
- Next, from the Attach File area, click on the Browse My Computer button. Find the document you saved as “WK8Assgn+last name+first initial.(extension)” and click Open.
- If applicable: From the Plagiarism Tools area, click the checkbox for I agree to submit my paper(s) to the Global Reference Database.
- Click on the Submit button to complete your submission.
Grading Criteria
To access your rubric:
Week 8 Assignment Rubric
Check Your Assignment Draft for Authenticity
To check your Assignment draft for authenticity:
Submit your Week 8 Assignment draft and review the originality report.
Submit Your Assignment by Day 7
To participate in this Assignment:
Week 8 Assignment
Psychotherapy for Clients with Addictive Disorders Example Approach
Addictive Disorders manifest via deficits in regulating emotions, self-esteem, relationships, and self-care, leading to the inability to abandon detrimental substances or behaviors. Often, causal factors for addictive disorders include biological, psychosocial, cultural, and social factors. According to Khantzian (2020), environmental influences such as traumatic abuse, peer pressure, safety, and parenting may increase individual susceptibility to addiction. With much emphasis regarding addictive disorders resting on substance abuse and gambling, various psychoanalytical psychotherapy is one of the most profound interventions for treating and preventing addiction.
Psychoanalytical Psychotherapy and Addiction Treatment
Psychoanalytical/psychodynamic psychotherapy assumes that essential psychological factors lead to addictive behaviors and activities (Khantzian, 2020). In a retrospective study by Mooney et al. (2019), the researchers evaluate the applicability of psychoanalytical psychotherapy in treating and preventing gambling addiction. Therefore, the research targets patients struggling with compulsive addiction seeking treatment at the National Problem Gambling Clinic (NPGC) in London. According to Mooney et al. (2019), psychodynamic therapy is crucial in exposing unconscious patterns by enabling patients to reflect, clarify, and confront interpersonal conflicts, wishes, and defenses that strengthen addiction.
The research revealed that psychodynamic psychotherapy successfully treated patients’ addiction problems by imparting a sense of intrinsic awareness while reducing depression and anxiety. However, researchers acknowledged that various limitations hampered the study’s precision and validity of the conclusion. For instance, investigators identified a lack of scholarly literature, data disparities, and research model as the major drawbacks for the study. Therefore, it is essential to evaluate scholarly evidence to justify the applicability of psychodynamic psychotherapy in addressing addiction.
Additional Scholarly Evidence
Although insufficient scholarly evidence compromises the determination to render psychodynamic psychotherapy effective in treating addiction, some studies support this approach. Verma & Vijayakrishnan (2018) argue that this therapeutic approach helps patients better understand themselves, their unconscious desires, motivations, and conflicts. On the other hand, Whitman & Olesker (2021) contend that psychoanalytic approaches play a significant role in treating opiate, alcohol, and marijuana dependence patients. Finally, Khantzian (2020) supports the topic by arguing that psychodynamic psychotherapy enables change agents to identify, target, modify and eliminate causal factors for addiction. Undoubtedly, these sources are scholarly because they are peer-reviewed, organized, and published in reputable databases to provide additional insights into the topic.
References
Khantzian, E. (2020). Psychodynamic psychotherapy for the treatment of substance use disorders. Textbook Of Addiction Treatment, 383-389. https://doi.org/10.1007/978-3-030-36391-8_26
Mooney, A., Roberts, A., Bayston, A., & Bowden?Jones, H. (2019). The piloting of a brief relational psychodynamic protocol (psychodynamic addiction model) for problem gambling and other compulsive addictions: A retrospective analysis. Counselling And Psychotherapy Research, 19(4), 484-496. https://doi.org/10.1002/capr.12251
Verma, M., & Vijayakrishnan, A. (2018). Psychoanalytic psychotherapy in addictive disorders. Indian journal of psychiatry, 60(Suppl 4), S485–S489. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_16_18
Whitman, L., & Olesker, W. (2021). Introduction – Addiction: A ubiquitous problem. The Psychoanalytic Study of The Child, 74(1), 227-233. https://doi.org/10.1080/00797308.2020.1859302
NRNP 6645 Week 8 Assignment Psychotherapy for Clients With Addictive Disorders Rubric Detail
Select Grid View or List View to change the rubric’s layout
Excellent90%–100%
Good80%–89%
Fair70%–79%
Poor0%–69%
Develop a 5- to 10-slide PowerPoint presentation on your selected research article discussing a therapeutic approach for treating clients, families, or groups with addictive disorders. •Provide an overview of the article you selected, including: What population (individual, group, or family) is under consideration? What was the specific intervention that was used? Is this a new intervention or one that was already used? What were the author’s claims? 18 (18%) – 20 (20%)The presentation thoroughly and accurately defines the considered population.
The specific intervention used is fully and accurately described. The description clearly indicates whether the intervention is new or whether it was already studied.
The response includes a thorough and accurate description of the author’s claims.
16 (16%) – 17 (17%)The presentation defines the considered population.
The specific intervention used is described. The description indicates whether the intervention is new or whether it was already studied.
The response includes a description of the author’s claims.
14 (14%) – 15 (15%)There is an incomplete definition of the considered population.
The specific intervention used is partially or inaccurately described.
The response includes a partial or inaccurate description of the author’s claims.
0 (0%) – 13 (13%)There is an incomplete definition of the considered population, or it is missing.
The specific intervention used is partially or inaccurately described, or is missing.
The response includes a partial or inaccurate description of the author’s claims, or is missing.
o Explain the findings/outcomes of the study in the article. Include whether this will translate into practice with your clients. If so, how? If not, why? 23 (23%) – 25 (25%)The presentation includes a thorough and accurate review of the findings of the selected article.
The response fully addresses whether or not the outcomes will translate into practice with clients.
20 (20%) – 22 (22%)The presentation includes a review of the findings of the selected article.
The response addresses whether or not the outcomes will translate into practice with clients.
18 (18%) – 19 (19%)The presentation includes a somewhat inaccurate or incomplete review of the findings of the selected article.
The response partially or inaccurately addresses whether or not the outcomes will translate into practice with clients.
0 (0%) – 17 (17%)The presentation includes an inaccurate and incomplete review of the findings of the selected article, or is missing.
The response partially or inaccurately addresses whether or not the outcomes will translate into practice with clients, or is missing.
• Explain whether the limitations of the study might impact your ability to use the findings/outcomes presented in the article. 23 (23%) – 25 (25%)The presentation includes a thorough and accurate explanation of the whether the limitations of the study might impact your ability to use the findings presented in the article. 20 (20%) – 22 (22%)The presentation includes an explanation of the whether the limitations of the study might impact your ability to use the findings presented in the article. 18 (18%) – 19 (19%)The presentation includes a somewhat inaccurate or incomplete explanation of the whether the limitations of the study might impact your ability to use the findings presented in the article. 0 (0%) – 17 (17%)The presentation includes an inaccurate or incomplete explanation of the whether the limitations of the study might impact your ability to use the findings presented in the article, or is missing.•Use the Notes function of PowerPoint to craft presenter notes to expand upon the content of your slides. 9 (9%) – 10 (10%)The Notes function of the presentation is appropriately used to comprehensively expand upon the presentation slides. 8 (8%) – 8 (8%)The Notes function of the presentation is adequately used to expand upon the presentation slides. 7 (7%) – 7 (7%)The Notes function of the presentation is utilized but notes are vague or contain small inaccuracies. 0 (0%) – 6 (6%)The Notes function of the presentation partially or inaccurately expands upon the presentation slides, or is not included.• Support your response with at least three peer-reviewed, evidence-based sources. Explain why each of your supporting sources is scholarly. References are included on your last slide. PDFs of sources are included with submission. 9 (9%) – 10 (10%)The presentation is strongly supported with at least three peer-reviewed, evidence-based, scholarly sources. References are included on the last slide. PDFs of sources are included with submission. 8 (8%) – 8 (8%)The presentation is supported with at least three peer-reviewed, evidence-based, scholarly sources. References are included on the last slide. PDFs of sources are included with submission. 7 (7%) – 7 (7%)The presentation is supported with two or three peer-reviewed, evidence-based, scholarly sources. Accurate references may not be included on the last slide. PDFs of sources may be missing. 0 (0%) – 6 (6%)The presentation is supported with resources peer-reviewed, evidence-based, scholarly sources, or the sources are missing.Written Expression and Formatting – Style and Organization: Slides are clear and not overly crowded. Sentences in presenter notes are carefully focused—neither long and rambling nor short and lacking substance. 5 (5%) – 5 (5%)Slides are clear, concise, and visually appealing. Sentences in presenter notes follow writing standards for flow, continuity, and clarity. 4 (4%) – 4 (4%)Slides are clear and concise. Sentences follow writing standards for flow, continuity, and clarity 80% of the time. 3.5 (3.5%) – 3.5 (3.5%)Slides may be somewhat unorganized or crowded. Sentences follow writing standards for flow, continuity, and clarity 60%–79% of the time. 0 (0%) – 3 (3%)Slides are unorganized and/or crowded. Sentences follow writing standards for flow, continuity, and clarity < 60% of the time.Written Expression and Formatting – English writing standards: Correct grammar, mechanics, and proper punctuation 5 (5%) – 5 (5%)Uses correct grammar, spelling, and punctuation with no errors. 4 (4%) – 4 (4%)Contains 1 or 2 grammar, spelling, and punctuation errors. 3.5 (3.5%) – 3.5 (3.5%)Contains 3 or 4 grammar, spelling, and punctuation errors. 0 (0%) – 3 (3%)Contains many (? 5) grammar, spelling, and punctuation errors that interfere with the reader’s understanding.Total Points: 100Also Read: NRNP 6645 Week 6 Supportive and Interpersonal Psychotherapy
READ MORE >>
NRNP 6650 Psychotherapy With Groups and FamiliesWeek 1: Legal and Ethical Consid ...
NRNP 6650 Psychotherapy With Groups and Families
Week 1: Legal and Ethical Considerations for Group and Family Therapy
Members of a cohesive group feel warmth and comfort in the group and a sense of belongingness; they value the group and feel in turn that they are valued, accepted, and supported by other members.
—Irvin D. Yalom, The Theory and Practice of Group Psychotherapy
Laureate Education (Producer). (2017). Introduction to psychotherapy with groups and families [Video file]. Baltimore, MD: Author.
Note: The approximate length of this media piece is 2 minutes.
Accessible player
Group and family therapy offers a unique sense of community and support that may not be achieved through other therapeutic approaches. As you help clients effect change within themselves, they are able to in turn help others within the group change. Although many clients thrive in this environment, it is important to recognize that group and family therapy is not appropriate for everyone. Like any other therapeutic approach, group and family therapy has limitations that must be considered.
This week, as you begin exploring group and family therapy, you examine legal and ethical considerations of this therapeutic approach.
NRNP 6650 Psychotherapy With Groups and Families Learning Resources
Required Readings
American Nurses Association. (2014). Psychiatric-mental health nursing: Scope and standards of practice (2nd ed.). Washington, DC: Author.
- Standard 5A “Coordination of Care” (page 54)
Note: Throughout the program you will be reading excerpts from the ANA’s Scope & Standards of Practice for Psychiatric-Mental Health Nursing. It is essential to your success on the ANCC board certification exam for Psychiatric/Mental Health Nurse Practitioners that you know the scope of practice of the advanced practice psychiatric/mental health nurse. You should also be able to differentiate between the generalist RN role in psychiatric/mental health nursing and the advanced practice nurse role.
Breeskin, J. (2011). Procedures and guidelines for group therapy. The Group Psychologist, 21(1). Retrieved from http://www.apadivisions.org/division-49/publications/newsletter/group-psychologist/2011/04/group-procedures.aspx
Khawaja, I. S., Pollock, K., & Westermeyer, J. J. (2011). The diminishing role of psychiatry in group psychotherapy: A commentary and recommendations for change. Innovations in Clinical Neuroscience, 8(11), 20-23.
Koukourikos, K., & Pasmatzi, E. (2014). Group therapy in psychotic inpatients. Health Science Journal, 8(3), 400-408.
Lego, S. (1998). The application of Peplau’s theory to group psychotherapy. Journal of Psychiatric and Mental Health Nursing, 5(3), 193-196. doi:10.1046/j.1365-2850.1998.00129.x
McClanahan, K. K. (2014). Can confidentiality be maintained in group therapy? Retrieved from http://nationalpsychologist.com/2014/07/can-confidentiality-be-maintained-in-group-therapy/102566.html
Nichols, M., & Davis, S. D. (2020). The essentials of family therapy (7th ed.). Boston, MA: Pearson.
- Chapter 1, “Introduction Becoming a Family Therapist” (pp. 1–5)
- Chapter 1, “The Evolution of Family Therapy” (pp. 6-22)
U.S. Department of Health & Human Services. (2014). HIPAA privacy rule and sharing information related to mental health. Retrieved from http://www.hhs.gov/sites/default/files/ocr/privacy/hipaa/understanding/special/mhguidancepdf.pdf
Wheeler, K. (Ed.). (2014). Psychotherapy for the advanced practice psychiatric nurse: A how-to guide for evidence-based practice. New York, NY: Springer.
- Chapter 11, “Group Therapy” (pp. 407–428)
Document: Midterm Exam Study Guide (Word document)
Document: Final Exam Study Guide (Word document)
Required Media
Laureate Education (Producer). (2015). Microskills: Family counseling techniques 1 [Video file]. Baltimore, MD: Author.
Note: The approximate length of this media piece is 32 minutes.
Accessible player
Laureate Education (Producer). (2015). Microskills: Family counseling techniques 2 [Video file]. Baltimore, MD: Author.
Note: The approximate length of this media piece is 32 minutes.
Accessible player
Laureate Education (Producer). (2015). Microskills: Family counseling techniques 3 [Video file]. Baltimore, MD: Author.
Note: The approximate length of this media piece is 24 minutes.
Accessible player
Sommers, G., Feldman, S., & Knowlton, K. (Producers). (2008a). Legal and ethical issues for mental health professionals, volume 1: Confidentiality, privilege, reporting, and duty to warn [Video file]. Mill Valley, CA: Psychotherapy.net. [Kanopy]
Note: You will access this media from the Walden Library databases. The approximate length of this media piece is 140 minutes.
Optional Resources
Sommers, G., Feldman, S., & Knowlton, K. (Producers). (2008). Legal and ethical issues for mental health professionals, volume 2: Dual relationships, boundaries, standards of care and termination [Video file]. Mill Valley, CA: Psychotherapy.net.
Note: You will access this media from the Walden Library databases. The approximate length of this media piece is 191 minutes.
Discussion: Legal and Ethical Considerations for Group and Family Therapy
Considering the Health Insurance Portability and Accountability Act (HIPPA), the idea of discussing confidential information with a patient in front of an audience is probably quite foreign to you. However, in group and family therapy, this is precisely what the psychiatric mental health nurse practitioner does. In your role, learning how to provide this type of therapy within the limits of confidentiality is essential. For this Discussion, consider how limited confidentiality and other legal and ethical considerations might impact therapeutic approaches for clients in group and family therapy.
Learning Objectives
Students will:
- Compare legal and ethical considerations for group and family therapy to legal and ethical considerations for individual therapy
- Analyze the impact of legal and ethical considerations on therapeutic approaches for clients in group and family therapy
- Recommend strategies to address legal and ethical considerations for group and family therapy
To prepare:
- Review this week’s Learning Resources and consider the insights they provide on group and family therapy.
- View the media, Legal and Ethical Issues for Mental Health Professions, Volume I, and reflect on legal and ethical considerations for group and family therapy and individual therapy.
Note: For this Discussion, you are required to complete your initial post before you will be able to view and respond to your colleagues’ postings. Begin by clicking on the Post to Discussion Question link and then select Create Thread to complete your initial post. Remember, once you click submit, you cannot delete or edit your own posts, and you cannot post anonymously. Please check your post carefully before clicking Submit!
By Day 3
Post an explanation of how legal and ethical considerations for group and family therapy differ from those for individual therapy. Then, explain how these differences might impact your therapeutic approaches for clients in group and family therapy. Support your rationale with evidence-based literature.
By Day 6
Respond to at least two of your colleagues by suggesting strategies to address the legal and ethical considerations your colleagues discussed. Support your responses with evidence-based literature.
Practicum – Upcoming Deadline
In the Nurse Practitioner programs of study (FNP, AGACNP, AGPCNP, and PMHNP) you are required to take several practicum courses. If you plan on taking a practicum course within the next two terms, you will need to submit your application via Meditrek .
For information on the practicum application process and deadlines, please visit the Field Experience: College of Nursing: Application Process – Graduate web page.
Please take the time to review the Appropriate Preceptors and Field Sites for your courses.
Please take the time to review the practicum manuals, FAQs, Webinars and any required forms on the Field Experience: College of Nursing: Student Resources and Manuals web page.
- Field Experience: College of Nursing Quick Answers
- Field Experience: MSN Nurse Practitioner Practicum Manual
- Student Practicum Resources: NP Student Orientation
NRNP 6650 Psychotherapy With Groups and Families Week 2: Family Assessment and Phases of Family Therapy
A family’s patterns of behavior influences [sic] the individual and therefore may need to be a part of the treatment plan. In marriage and family therapy, the unit of treatment isn’t just the person – even if only a single person is interviewed – it is the set of relationships in which the person is imbedded.
—American Association of Marriage and Family Therapy, “About Marriage and Family Therapists”
When issues arise within a family unit, the family often presents with one member identified as the “problem.” However, you will frequently find that the issue is not necessarily the “problem client,” but rather dysfunctional family patterns and relationships. To better understand such patterns and relationships and develop a family treatment plan, it is essential that the practitioner appropriately assess all family members. This requires you to have a strong foundation in family assessment and therapy.
This week, as you explore family assessment and therapy, you assess client families presenting for psychotherapy.
Learning Resources
Required Readings
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
L’Abate, L. (2015). Highlights from 60 years of practice, research, and teaching in family therapy. American Journal of Family Therapy, 43(2), 180-196. doi:10.1080/01926187.2014.1002367
Mojta, C., Falconier, M. K., & Huebner, A. J. (2014). Fostering self-awareness in novice therapists using internal family systems therapy. American Journal of Family Therapy, 42(1), 67–78. doi:10.1080/01926187.2013.772870
Nichols, M., & Davis, S. D. (2020). The essentials of family therapy (7th ed.). Boston, MA: Pearson.
- Chapter 2, “Basic Techniques of Family Therapy” (pp. 23-39)
- Chapter 3, “The Fundamental Concepts of Family Therapy” (pp. 40-55)
Nichols, M., & Tafuri, S. (2013). Techniques of structural family assessment: A qualitative analysis of how experts promote a systemic perspective. Family Process, 52(2), 207-215. doi:10.1111/famp.12025
Papero, D. V. (2014). Assisting the two-person system: An approach based on the Bowen theory. Australian & New Zealand Journal of Family Therapy, 35(4), 386-397. doi:10.1002/anzf.1079
Wheeler, K. (Ed.). (2014). Psychotherapy for the advanced practice psychiatric nurse: A how-to guide for evidence-based practice. New York, NY: Springer.
- Chapter 12, “Family Therapy” (pp. 429–468)
Document: Group Therapy Progress Note
Required Media
Laureate Education (Producer). (2013a). Hernandez family> Sessions 1—6 [Video file]. Author: Baltimore, MD.
Note: The approximate length of this media piece is 52 minutes.
Psychotherapy.net. (2006c). Tools and techniques for family therapy [Video file].
The approximate length of this media piece is 52 minutes.
Assignment : Hernandez Family Assessment
Assessment is as essential to family therapy as it is to individual therapy. Although families often present with one person identified as the “problem,” the assessment process will help you better understand family roles and determine whether the identified problem client is in fact the root of the family’s issues. As you examine the Hernandez Family: Sessions 1-6 videos in this week’s Learning Resources, consider how you might assess and treat the client family.
Learning Objectives
Students will:
- Assess client families presenting for psychotherapy
To prepare:
- Review this week’s Learning Resources and reflect on the insights they provide on family assessment.
- View the Hernandez Family: Sessions 1-6 videos, and consider how you might assess the family in the case study.
Note: For guidance on writing a comprehensive client assessment, refer to pages 137–142 of Wheeler (2014) in this week’s Learning Resources.
The Assignment
Address in a comprehensive client assessment of the Hernandez family the following:
- Demographic information
- Presenting problem
- History or present illness
- Past psychiatric history
- Medical history
- Substance use history
- Developmental history
- Family psychiatric history
- Psychosocial history
- History of abuse and/or trauma
- Review of systems
- Physical assessment
- Mental status exam
- Differential diagnosis
- Case formulation
- Treatment plan
Note: Any item you are unable to address from the video should be marked “needs to be added to” as you would in an actual comprehensive client assessment
Also Read: COUN 5279 Unit 4 Assignment Job Loss Case Study
READ MORE >>
NRNP 6665 PMHNP Care Across the Lifespan INRNP/PRAC 6665 & 6675 Comprehensiv ...
NRNP 6665 PMHNP Care Across the Lifespan I
NRNP/PRAC 6665 & 6675 Comprehensive Focused SOAP Psychiatric Evaluation Template
Name: P.P DOB: 1/07/1995 Age: 25 yrs Gender: female
Subjective:
CC (chief complaint): mood cycles between periods of low energy for about 4 to 5 times in a year, and mostly being high for more than a week in a row.
HPI: the patient came for a mental health assessment, and seeking review of her medications after being treated for previous psychiatric symptoms and being started on medications. She has a history of being treated using medications such as Zoloft, Risperidone, Seroquel (quetiapine), and Clonazepam, then stopping due to side effects. She reports getting episodes of low energy, no motivation, disinterest in activities 4 to 5 times a year. During these low periods, she often skips work, and eats too much, and prefers to sleep mostly up to 12 to 16 hours a day. She reports having periods that she is high for over a week, whereby she sometimes has auditory hallucinations. Excessive talking, insomnia for days, increased goal-orientedness, and heightened sexual behavior. The conversation also revealed she has grandiosity and a heightened sense of importance whereby she envisions everything about her future being with celebrity stars.
Past Psychiatric History: history of several admissions or psychiatric symptoms, she has had no suicidal or homicidal ideation since 2017.
Family Psychiatric History: her mother suffered from a psychiatric illness which she thinks was either bipolar and she tried committing suicide once. Her father went to prison for drugs and thinks her brother probably also has been diagnosed with a psychiatric problem before.
Legal History: she has been arrested once for public disturbance, but thinks this was made up because she cannot remember that scene
Substance Current Use: she smokes one packet of cigarettes daily, and has no recent history of other prescription drugs or substance abuse.
Medical History: he has hypothyroidism and polycystic ovarian syndrome (PCOS)
- Current Medications: takes thyroxines for hypothyroidism and oral contraceptive pills for PCOS
- Allergies:no known food or drug allergies.
- Reproductive Hx: heterosexual female but has a heightened sexual life at different times which places her at high risk.
Review of systems (ROS):
- GENERAL: no fever, night sweats, or vomiting, but amidst to have gained weight when taking some psychotropic medications
- HEENT: no changes in visual acuity, no diplopia, eye discharge, or photophobia. She has no ear pain, tinnitus, or discharge. No history of nose bleeding, recurrent upper airway infections, she has no denture or teeth problems, and reports of good oral hygiene.
- SKIN: normal hair texture and pigmentation, no nodules, ulcers, or lesions.
- CARDIOVASCULAR: she has no paroxysmal nocturnal dyspnea, intermittent claudication, palpitations or chest pain.
- RESPIRATORY: no exertion or difficulty in breathing, hemoptysis, or coughing.
- GASTROINTESTINAL: she has a good appetite, no changes in bowel habits, no nausea, vomiting, heartburn, dysphagia, yellowness of eyes, or abdominal pain.
- GENITOURINARY: no urinary urgency, incontinence, hematuria, frequency, hesitancy, dysuria, color changes, or decreased urine output.
- NEUROLOGICAL: No changes in memory, convulsions, syncope, lightheadedness, abnormal sensations, or dizziness.
- MUSCULOSKELETAL: no changes in gait or mobility, no joint aches, swelling, fractures, or history of arthritis or gout.
- HEMATOLOGIC: no bloody or dark stool, no easy bruising, or nosebleeding.
- LYMPHATICS: no peripheral edema, or swellings
- ENDOCRINOLOGIC: she has no polyuria, polydipsia, or constant polyphagia. She, however, reports slowness and a history of current treatment for hypothyroidism.
Objective:
Physical Exam
General: He was well-groomed, seemed overweight, and normal gait.
Vital signs: BP 123/78; pulse 81 regularly regular, temperature 37.5 ear; RR 21; weight: 142lbs; height 5’2; BMI 26 (overweight).
The rest of the systemic examination was normal.
Diagnostic results: awaiting results of her lipid profile.
Assessment:
Mental Status Examination:
Appearance: looked like a young adult, and as she walked in she responded to my greetings and sat with normal posture. She was well dressed, despite having the smell of cigarettes she did not look intoxicated. she had no obvious bruises or body scars on exposed areas.
Level of consciousness and Orientation: she was alert and well orientated to time and place, and person.
Behavior: she was charming, had good rapport and attitude despite getting irritable on few occasions, and being too critical of personal questions. However, she was cooperative on kind assurance, with no abnormal movement or compulsions, and didn’t resist being examined.
Concentration and attention: she maintained normal eye contact, and was attentive throughout the assessment.
Speech: her speech was not pressured, with normal volume and tone, with a short latency of speech. She responded to questions adequately, despite admitting to having a history of excessive talking. Mood: currently has a normal mood she often feels high “keep my moods high, high, high”, but also sometimes gets depressed “I feel like I’m not worth anything”
Affect: neutral Appropriate to content and congruent with the mood.
Thought Process: she expressed herself in a logical and meaningful manner. She had no circumstantiality, tangentiality, or flight of ideas, she had no neologisms or thought blocking.
Thought content: she has ideas of grandeur, and pseudo-delusional conviction of importance, but no poverty of thought, and no suicidal and homicidal ideation. She has no phobias or irrational fears, no obsessions or compulsions.
Perceptual Disturbances: she has auditory hallucinations, no illusions, and no episodes of depersonalization or derealization.
Cognition: her Immediate, short-term, and long-term memory were intact. She had good attention, judgment, abstraction, and level 6 insight.
Diagnostic Impression: Bipolar 1 Disorder.
The patient was otherwise normal on this visit since the mental status examination only tells about the mental status at that moment, but can change at any time. The presenting complaints and information gathered on a further inquiry made me arrive at a primary diagnosis of bipolar 1 disorder. According to Ganti et al., (2018), Bipolar I disorder is diagnosed when one meets the criteria for a full manic episode with or without episodes of major depression, thus also called manic-depression. Often patients have interspersed euthymia, major depressive episodes, or hypomanic episodes between manic episodes (Perrotta, 2019), of which she presented in a euthymic state on this visit. She is mostly in the manic phase due to undertreatment (López-Muñoz et al., 2018), since the euphoria, heightened energy, and goal-orientedness make her skip her medications.
Differential diagnoses:
Schizoaffective disorder: patients with this disorder, often meet criteria for either a major depressive or manic episode during which psychotic symptoms such as hallucinations and delusions consistent with schizophrenia are also met. Additionally, mood symptoms present for a majority of the psychotic illnesses since some may have atypical features such as flat or blunted affect, anhedonia, apathy, and lack of interest in socialization (Ganti et al., 2018). As such patients often cycle between having a diagnosis between psychotic and mood disorders, thus are given the second generation. antipsychotics such as risperidone to target both psychotic and mood symptoms.
Organic mood disorder due to hypothyroidism: psychiatric symptoms may also be a manifestation of organic disorders such as endocrine or metabolic disorders. Additionally, patients with bipolar also have a high prevalence of psychiatric and medical comorbidities (Grande et al., 2016), such as thyroid disorders or diabetes. She admits to having comorbid hypothyroidism, which could explain the episodes of depression due to undertreatment since she has a history of skipping other medications.
Seasonal affective disorder: This condition is often described as a subtype of recurrent depressive or bipolar disorder. Often patients have recurrent dysregulated mood and affective episodes of regular onset and remission of similar times annually (Pjrek et al., 2016). This condition has been shown to have a high degree of persistence and only about 20 percent of patients get to complete remission after five to eleven years (Nussbaumer-Streit et al., 2018). This is less probable because she described manic symptoms that lasted more than a week (Ganti et al., 2018), thus meeting the criteria for a manic episode.
Case Formulation: this case involves P.P, who is a 25-year-old female with comorbid hypothyroidism and PCOS. Despite having major depressive episodes, where she has anhedonia, hypersomnia, depressed mood, feelings of worthlessness, slowness, loss of energy, and excessive eating, she also experiences manic episodes consisting of grandiosity, inflated self-esteem, increased goal-orientedness, decreased need for sleep, and talkativeness, and excessive involvement in sexual indiscretions despite its negative consequences.
Treatment Plan: most psychiatric conditions require both pharmacotherapy and psychotherapy to have good outcomes. Bipolar patients benefit from mood stabilizers such as lithium, which has been shown to reduce mania and suicide risk, or carbamazepine, especially if the symptoms are rapidly cycling. Most patients have a faster response when mood stabilizers are combined with atypical antipsychotics such as risperidone and quetiapine. Antidepressants are discouraged as monotherapy due to concerns of activating mania or hypomania. I would start her on carbamazepine, at an Initial dose of 200 mg PO q12hr, since it is easier to monitor and make adjustments unlike lithium (Arcangelo et al., 2017). Additionally, I would recommend her to start on Supportive individual therapy, then later enlist her into group therapy to help prolong remission once the acute manic episode has been controlled. I would encourage her to start thinking of quitting smoking and weight reduction since they negatively affect her health.
Reflection notes:
This patient presented minimal challenges since she had good insight into her psychiatric problem. Otherwise, I think I would have explored more on how the symptom cycle between mania and depression and the periods of these symptoms. Additionally asking more about psychotic symptoms such as illusion and delusions would help make a clearer diagnosis with specifiers. If this patient becomes difficult to follow up I would consider referring her to a psychiatrist, and an addiction and wellness counselor
References
- Arcangelo, V. P., Peterson, A. M., Wilbur, V., & Reinhold, J. (2017). Pharmacotherapeutics for Advanced Practice (Vol. 4). Philadelphia: Wolters Kluwer.
- Ganti, L. K. (2018). First aid for the psychiatry clerkship. McGraw Hill Professional.
- Grande, I., Berk, M., Birmaher, B., & Vieta, E. (2016). Bipolar disorder. The Lancet, 387(10027), 1561-1572. https://doi.org/10.1016/s0140-6736(15)00241-x
- López-Muñoz, F., Shen, W. W., D’ocon, P., Romero, A., & Álamo, C. (2018). A history of the pharmacological treatment of bipolar disorder. International Journal of Molecular Sciences, 19(7), 2143. https://dx.doi.org/10.3390%2Fijms19072143
- Nussbaumer-Streit, B., Pjrek, E., Kien, C., Gartlehner, G., Bartova, L., Friedrich, M. E., Kasper, S. & Winkler, D. (2018). Implementing prevention of seasonal affective disorder from patients’ and physicians’ perspectives–a qualitative study. BMC Psychiatry, 18(1), 1-10. https://doi.org/10.1186/s12888-018-1951-0
- Perrotta, G. (2019). Bipolar disorder: definition, differential diagnosis, clinical contexts, and therapeutic approaches. Journal of Neuroscience and Neurological Surgery, 5(1), 1-6. DOI: 10.31579/2578-8868/097
- Pjrek, E., Baldinger-Melich, P., Spies, M., Papageorgiou, K., Kasper, S., & Winkler, D. (2016). Epidemiology and socioeconomic impact of seasonal affective disorder in Austria. European Psychiatry, 32, 28-33. https://doi.org/10.1016/j.eurpsy.2015.11.001
READ MORE >>
NRNP 6675 Week 3 Assignment 2 Study PlanNRNP 6675 Week 3 Assignment 2 Study Plan ...
NRNP 6675 Week 3 Assignment 2 Study Plan
NRNP 6675 Week 3 Assignment 2 Study Plan
Study Plan Example
My first study goal this term is to understand key concepts in psychotherapy by learning more about possible side-effects of antipsychotics and the effects of chronic drug administration. I will achieve this by reviewing the two topics at least three times per week and dedicate at least one distraction-free thirty minutes daily to handling five questions related to the topic for the entire month.
Implementing fundamental life goals and learning goals augments learners’ self-governing motivation to learn and enjoy learning (Froiland, 2021). My second goal encompasses attaining a thorough and profound understanding of the various types of psychotherapy and learning how to practice these different approaches on patients. I intend to study the five approaches to psychotherapy within five weeks, rereading one method weekly.
My third goal is to improve how I tackle and answer test questions. I particularly want to learn how to break the question into smaller parts. This will boost my understanding of the questions in smaller parts rather than a whole question. I will use psychopharmacology review questions from flashcards and online sites such as Quizlet, rich in questions and content instrumental in my practice.
According to Sharmin and Chow (2020), scholars who use technology and mobile devices daily frequently lack the time and motivation to make and use flashcards efficiently. I intend to minimize using my phone to google answers and instead use flashcards. I will review at least one question and practice how to answer it daily until the certification exam.
To attain the three goals, I will create a detailed plan of action, eliminate bad habits such as poor time management, and instill self-discipline. I will ensure that I follow my timetable and utilize the assigned time effectively to accomplish each set goal. I also intend to join a study group to promote creativity and build sturdier communication skills. According to Gouvea (2019), sharing notions and concepts in a group can be risky, creating feelings of embarrassment or conflict.
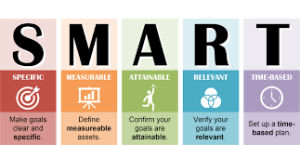
As a shy person, I intend to improve my communication skills and boost my confidence by joining the study group. This will also enhance my understanding of the key concepts in psychotherapy types of psychotherapy and improve how I tackle test questions. Having set SMARTER (specific, measurable, achievable, relevant, time-bound) goals, focusing on areas that require growth, I will excel in the certification exam.
References
Froiland, J. M. (2021). The intrinsic learning goals of elementary school students, in their own words. Journal of Humanistic Psychology, 61(4), 629-649. https://doi.org/10.1177%2F0022167818763923
Gouvea J. S. (2019). Learning in a Group, as a Group, and between Groups. CBE Life Sciences Education, 18(2), fe4. https://doi.org/10.1187/cbe.19-03-0067
Sharmin, N., & Chow, A. K. (2020). Augmented Reality Application to Develop a Learning Tool for Students: Transforming Cellphones into Flashcards. Healthcare Informatics Research, 26(3), 238–242. https://doi.org/10.4258/hir.2020.26.3.238
The Assignment
Revise your study plan summarizing your current strengths and opportunities for improvement.
Develop 3-4 new SMART goals for this quarter and the tasks you need to complete to accomplish each goal. Include a timetable for accomplishing them and a description of how you will measure your progress.
Describe resources you would use to accomplish your goals and tasks, such as ways to participate in a study group or review course, mnemonics and other mental strategies, and print or online resources you could use to study.
Can you imagine an athlete deciding to run a marathon without training for the event? Most ambitious people who have set this goal will follow a specific training plan that will allow them to feel confident and prepared on the big day. Similarly, if you want to feel confident and prepared for your certification exam, you should create and follow a plan that will thoroughly prepare you for success.
In this Assignment, you will review the study plan that you developed in NRNP 6665, and revise your plan as necessary, which will serve as the road map for you to follow to attain your certification.
To Prepare
Reflect on the study plan you created in NRNP 6665. Did you accomplish your SMART goals? What areas of focus still present opportunities for growth?
Personal Reflection and Study Plan Sample
Nursing education is meant to prepare healthcare professionals for excellent clinical practice. Psychiatric Mental Health Nurse Practitioners (PMHNPs) are among the health care professionals that must go through education to acquire the advanced necessary skills required to handle patients with mental health issues. Such advanced nursing education ensures that PMHNPs have future professional effectiveness.
At the end of this master’s degree level education program, PMHNPs must learn how to diagnose and treat psychiatric conditions. Tests are one of the ways to ensure that PMHNPs possess these competencies. Tests assess both practical and cognitive skills which are acquired through education.
Tests are offered by the American Nurses Credentialing Centre (ANCC). Continuous learning is one of the ways one can ensure they pass the certification exam. Continuous learning ensures that one is constantly improving on their weaknesses. It also gives one the chance to evaluate their weaknesses and find ways to improve on them.
A personal development plan can ensure one improves on their knowledge deficiencies. It can do this by ensuring that one gets out of their comfort zone. The purpose of this reflection paper is to look at some of my strengths and weaknesses as I prepare for the certification exam and also to provide a development plan which includes a study plan and some of the goals I intend to achieve before the certification exam.
Strengths and weaknesses.
The test revealed that there are areas that I need to work on and areas which I have mastered. One of my strengths is my ability to comprehensively take a psychiatric history and evaluate patients. This has been made possible by my understanding of the various psychopathologic processes of different psychiatric conditions.
This allows me to ask the right questions that might lead me towards an accurate diagnosis and to create a proper plan of management. I did fairly well in questions relating to psychotherapy because of the vast amount of knowledge I acquired from the psychotherapy class. I also did a number of practice questions on psychotherapy.
However, my weaknesses include psychopharmacology which entails having to memorize how psychoactive drugs exert their effects on behavior by altering neuronal communication in the brain, the use of specific classes of medications in treating mental disorders, as well as therapeutic use of psychotropic medication.
Going into the test I had some fears that I was weak in psychopharmacology and the test proved me right. This is mostly due to the fact that psychopharmacology has a lot of content and my opinion is that most of the content requires cramming in addition to basic understanding of pharmacokinetics and pharmacodynamics. I have difficulties with cramming. It is this weakness that will help me come up with my SMART goals.
SMART goals.
Goal 1: Increase my Knowledge base in psychopharmacology
Task: to ensure that I increase my knowledge in psychopharmacology, I will study for at least two hours daily, six days of the week until I sit for my certification exam. This will ensure that my learning is always continuous. I can use a psychopharmacology review book to help me accomplish this goal. I will make notes to enhance my understanding when reading.
I will also join a study group that will help me go over the various concepts in psychopharmacology. Study groups are useful for information sharing (Rahman et al., 2019). A study group might help me to simplify some of the concepts and to consolidate information into memory much easily.
Goal 2: Familiarize myself with test questions.
Task: to help my self to be more familiar to exam questions related to psychopharmacology, I will use a series of practice exam questions. This will help me to identify my weaknesses in psychopharmacology and to help me improve on them. The practice exams will also help me to keep track of how prepared I am for the final certification exam.
I will ensure that I do at least 20 questions on a daily basis from Monday to Friday. I will also subscribe to various psychopharmacology review websites to ensure that I do not run out of questions to practice with Testing is superior to re-studying concepts when trying to promote long-term retention of information (Yang et al., 2019).
Goal 3: improve my memory of psychopharmacotherapy concepts.
Task: to ensure this, I will make a list of psychiatric conditions and the most commonly prescribed major classes of psychotropic medications. I will also use flashcards that summarize the most important information in psychopharmacology. Flashcards optimize the learning of factual knowledge and improves memory performance (Sharmin & Chow, 2020).
I will make sure that I go through these flashcards every day before I go to sleep. I will also do practice questions on the various psychopharmacology concepts to help me ensure that I consolidate information into my long-term memory.
Resources and study plan.
To ensure that I accomplish the highlighted goals, several resources will be needed. Some of these resources include psychopharmacology review textbooks, online study resources, psychopharmacology review questions, flashcards, stationery including pens, notebooks, coloured markers, and well written lecture notes.
Learning aids like Quizlet can also be a useful resource. Group-based discussions help with interactive learning (Gouvea, 2019). All senses should be involved when learning to help with better retention of information. Additionally, I need to work on my test taking strategies. I the order to be smart about my pacing I will better distribute my test practice time, since it has been repeatedly proven to be more effective than cramming, so I won’t run out of time on my certification exam.
DAY 1DAY 2DAY 3DAY 4DAY 5DAY 6Study : 3 hrs.
Spaced repetition: 1 hr.
Study: 2 hrs.
Study Group: 1hr
Practice Questions: 1 hr.
Study: 2 hrs.
Study Group: 1hr
Practice Questions: 1
Study: 2 hrs.
Study Group: 1hr
Practice Questions: 1
Study: 2 hrs.
Study Group: 1hr
Practice Questions: 1
Study: 2 hrs.
Study Group: 1hr
Practice Questions: 1 hr.
TOTAL : 4 HRSTOTAL : 4 HRSTOTAL : 4 HRSTOTAL : 4 HRSTOTAL : 4 HRSTOTAL : 4 HRSReferences
Gouvea J. S. (2019). Learning in a Group, as a Group, and between Groups. CBE life sciences education, 18(2), fe4. https://doi.org/10.1187/cbe.19-03-0067
Rahman, K., Wahid, A., Afandi, I., Bali, M. M. E. I., & Hakim, L. (2019). Effectiveness of Teams Teaching-Hybrid Learning (TTHL) in Higher Education. In WESTECH 2018: Proceedings of 1st Workshop on Environmental Science, Society, and Technology, WESTECH 2018, December 8th, 2018, Medan, Indonesia (p. 263). European Alliance for Innovation. http://dx.doi.org/10.4108/eai.8-12-2018.2284036
Sharmin, N., & Chow, A. K. (2020). Augmented Reality Application to Develop a Learning Tool for Students: Transforming Cellphones into Flashcards. Healthcare informatics research, 26(3), 238–242. https://doi.org/10.4258/hir.2020.26.3.238
Yang, B. W., Razo, J., & Persky, A. M. (2019). Using Testing as a Learning Tool. American journal of pharmaceutical education, 83(9), 7324. https://doi.org/10.5688/ajpe7324
READ MORE >>
NRS 415 The Role of the Professional Nurse EssayNRS-415: Nursing Leadership and ...
NRS 415 The Role of the Professional Nurse Essay
NRS-415: Nursing Leadership and Interprofessional Collaboration Course introduces the student to the Core Competencies for Professional Nursing Education, the role of the professional nurse, and the importance of effective nursing leadership. Standards of practice, differentiated nursing practice, professional accountability, interprofessional collaboration, and quality improvement are emphasized with importance placed on the application of leadership styles and management skills.
The Nurses’ Role in Promoting Quality Healthcare
In a high-performing healthcare organization, the role of the staff nurse is integral to promoting and maintaining quality patient care. Fawaz et al. (2020) stated that staff nurses are the frontline caregivers who directly interact with patients and their families, making them crucial players in ensuring a positive healthcare experience. Their responsibilities encompass delivering direct patient care and contributing to the overall quality improvement initiatives within the organization.
The healthcare organization I am familiar with is known for its collaborative and patient-centered culture. It strongly emphasizes interdisciplinary teamwork, open communication, and continuous learning. The organization values innovation and encourages staff at all levels to contribute ideas for process improvements and better patient outcomes.
The CEO of this organization exhibits a transformational leadership style. They inspire and motivate the staff by articulating a clear vision for the organization’s future and fostering a sense of shared purpose. The CEO encourages creativity and empowers employees to take ownership of their roles. On the other hand, the Chief Nursing Officer (CNO) practices a supportive leadership style, focusing on creating a nurturing and respectful environment for nursing staff to excel.
The senior leadership recognizes the significance of patient safety and quality improvement. They understand that some changes necessitate financial investments and are willing to allocate resources to support initiatives to enhance patient safety and care delivery. The leadership team collaborates with various departments to ensure that necessary funds are allocated for projects that can lead to measurable improvements in patient outcomes.
Strategic threads carefully interweave in the pursuit of excellence within a healthcare organization to create a tapestry of enhanced patient care and operational effectiveness. Interdisciplinary collaboration forms a cornerstone where nurses work seamlessly with colleagues across departments, leveraging diverse expertise to enhance patient outcomes (Pomare et al., 2020). This collaborative synergy bolsters problem-solving capabilities and fosters an environment where fresh ideas flourish, leading to innovative approaches that uplift the quality of care.
Embedded within this fabric of collaboration is a commitment to data-driven decision-making. According to Pomare et al. (2020), nurses are equipped with insights that show options for development by utilizing the power of technology and analytics. This approach transforms raw data into actionable intelligence, enabling informed clinical judgments and process enhancements.
Moreover, the organization’s investment in continuous professional development for nursing staff enriches this strategic landscape. Through ongoing education, training workshops, and skill refinement, nurses remain equipped with the latest tools and knowledge, ensuring their ability to provide cutting-edge, evidence-based care to patients. This commitment to professional growth enhances individual competencies and fuels a collective culture of advancement and innovation.
References
Fawaz, M., Anshasi, H., & Samaha, A. (2020). Nurses at the front line of COVID-19: Roles, responsibilities, risks, and rights. The American Journal of Tropical Medicine and Hygiene, 103(4), 1341. https://doi.org/10.4269%2Fajtmh.20-0650
Pomare, C., Long, J. C., Churruca, K., Ellis, L. A., & Braithwaite, J. (2020). Interprofessional collaboration in hospitals: A critical, broad-based review of the literature. Journal of Interprofessional Care, 34(4), 509-519. https://doi.org/10.1080/13561820.2019.1702515
READ MORE >>
NRS 420 Health History Assessment PaperNRS-420: Health Assessment imparts the s ...
NRS 420 Health History Assessment Paper
NRS-420: Health Assessment imparts the student with critical knowledge on the methods of health history taking, physical examination skills, and documentation of findings. Students integrate assessment skills and clinical judgment/reasoning in identifying actual or potential health problems and needs across the life span. Health promotion strategies are incorporated to provide for the unique needs of the individual, ensuring person-centered care. The course emphasizes the importance of providing compassionate care dealing with diversity, equity, and inclusion. Students design plans of care based on evidence-based research and practice.
Building a Health History Example Paper
When conducting an interview with a 22-year-old LGBTQIA female Hispanic immigrant living in a middle-class suburb, it is essential to employ communication techniques tailored to her unique experiences and background. These communication techniques are not mere formalities but integral to ensuring that the patient feels understood, respected, and valued. In a healthcare setting, where vulnerability often accompanies patients, the way a practitioner communicates can significantly impact the effectiveness of care and the patient’s willingness to engage in the treatment process.
The first cornerstone of effective communication is empathetic listening (Ball et al., 2023). This goes beyond merely hearing the words the patient says, it involves understanding the emotions and experiences behind those words. For a young LGBTQIA woman who is also an immigrant, there may be layers of complexity in her experiences that necessitate a particularly sensitive and non-judgmental approach. She may have faced challenges related to her sexual orientation, gender identity, cultural adaptation, and possibly discrimination or social exclusion. Understanding these layers through empathetic listening helps build trust and a therapeutic relationship (Sullivan, 2019).
Cultural competence plays a critical role in this interaction. It involves an understanding and respect for the patient’s Hispanic heritage. Each culture has its own set of health beliefs, practices, and values, which can significantly influence a patient’s approach to healthcare (Ball et al., 2023). By acknowledging and respecting these cultural nuances, a healthcare provider can create a more welcoming and comfortable environment for the patient. This might involve understanding specific health beliefs prevalent in the Hispanic community or being aware of the cultural norms that might influence her health behaviors.
Inclusive language is particularly important considering the patient’s LGBTQIA identity (Bingham & Heavey, 2023). This involves using language that respects and affirms her gender identity and sexual orientation. Inclusivity in language is not just about political correctness; it is about creating a safe space where the patient feels seen and respected as her whole self. This includes avoiding assumptions about her relationships, preferences, or experiences based on her sexual orientation or gender identity.
Given her status as an immigrant, there might be language barriers or differences in understanding healthcare terminologies. Therefore, communication should be in clear, simple language. Using visual aids or translation services might be necessary to ensure that she fully understands the information being shared. This clarity in communication is not just about overcoming language barriers; it is about ensuring that the patient is fully informed and can actively participate in her healthcare decisions (Sullivan, 2019).
Targeted Questions:
- Health history and present concerns: “Can you share any health concerns you are currently experiencing or any significant past medical history?”
- Support system: What kind of support system do you have? This can include friends, family, or community groups.
- Experience as an immigrant: How has your experience been as an immigrant in this community? Are there any specific challenges or positive experiences you would like to share?
- LGBTQIA-specific concerns: As a member of the LGBTQIA community, have you faced any challenges related to this aspect of your identity, either personally or in accessing healthcare?
- Cultural and personal values: How do your cultural background and personal values influence your approach to health and healthcare?
Conclusion
The interview with a 22-year-old LGBTQIA female Hispanic immigrant in a middle-class suburb requires a communication approach that is empathetic, culturally sensitive, inclusive, clear, and encouraging open dialogue. By employing these techniques, a healthcare provider can ensure that the patient feels respected, understood, and comfortable sharing her experiences and concerns. This approach not only enhances the quality of the healthcare provided but also strengthens the patient-provider relationship, which is fundamental to effective healthcare delivery.
References
Ball, J. W., Dains, J. E., Flynn, J. A., Solomon, B. S., & Stewart, R. W. (2023). Seidel’s guide to physical examination: An interprofessional approach (10th ed.). Elsevier Mosby.
Bingham, K. W., & Heavey, E. (2023). Creating a friendly healthcare environment for LGBTQIA+ patients. Nursing, 53(1), 34–38. https://doi.org/10.1097/01.NURSE.0000903984.79871.c3
Sullivan, D. D. (2019). Guide to clinical documentation (3rd ed.). F. A. Davis.
Example Reflection Paper on Taking a Health History
While building the patient’s health history, I used both principles from science and art concepts of care. The process was similar to a job interview apart from the purpose of the information derived from answering the questions. This interview aimed to assess the risks and social determinants of health to establish an accurate and reliable health history. Therefore, hard questions or questions deemed as sensitive or personal were necessary.
Experiences
Developing the script for the interview required both critical and reflective thinking to incorporate goal-oriented questions while simultaneously considering the outcomes of the questions for the patient. The inclusion of the ‘hard’ questions was the critical step. Translating the evidence from clinical literature to suggest personal and direct closed questions was the first step towards developing.
Teenage pregnancy impacts both the teenager and parents, guardians, or the custodian economically and socially. To the teenager, the health burden of adolescent pregnancy increases due to the imbalance between the physiological demands and available physical and physiological body supply in that age group. Therefore, holistic care should take into account these factors.
In developing a health history, I targeted the questions toward establishing additional risks that could worsen these imbalances in biophysical and physiological imbalances in demand and supply. I also focused the interview on establishing a ground for planning for prenatal and postnatal care interventions and evaluation. Including the emotional outcomes of the health problem for the patients was guided by the idea that during the teenage period, physiological and social outcomes can cause body image and mood outcomes. Therefore, I believe that I maximized opportunities to plan holistic care through this history-taking.
Asking the Questions
Asking the questions would require setting the patient in the right mind and mood. Difficulties with had questions are related to the patient and clinician’s perceived impacts on the self-image. Fear of breaking the trust between the clinician and the patient also complicates asking hard questions. The clinician will target hornet answers and build a reliable health risks profile.
The patient can withhold honest responses to the questions due to a lack of trust that the clinical will maintain confidentiality or may judge them (Nasirian et al., 2018). Therefore, reassurance and active listening are some of the strategies that would improve the outcomes of the actual interview. The positioning with the patient, the body language, facial expressions, the tone of the questions, and the tone of the clinician’s responses are critical in establishing authentic and truthful responses from the patient (Ball et al., 2018).
The presence of a guardian in the interview suggests they would help corroborate the health history but may also limit the patient’s confidence in responding to sensitive questions. Therefore, the environment in terms of noise levels, lighting, and presence of third parties are key concepts I may consider when redoing the interview differently (Flugelman, 2021).
In sum, the development of the interview is artistic and scientific. Merging scientific and interpersonal interaction principles to achieve a reliable health history was the critical underpinning of the interview script development. Environmental considerations would be vital in influencing the authenticity and reliability of patient responses and establishing a therapeutic relationship to achieve different outcomes.
References
Ball, J. W., Dains, J. E., Flynn, J. A., Solomon, B. S., & Stewart, R. W. (2018). Seidel’s guide to physical examination: An interprofessional approach (9th ed.). Mosby.
Flugelman, M. Y. (2021). History-taking revisited: Simple techniques to foster patient collaboration, improve data attainment, and establish trust with the patient. GMS Journal for Medical Education, 38(6), Doc109. https://doi.org/10.3205/zma001505
Nasirian, M., Hosseini Hooshyar, S., Haghdoost, A. A., & Karamouzian, M. (2018). How and where do we ask sensitive questions: Self-reporting of STI-associated symptoms among the Iranian general population. International Journal of Health Policy and Management, 7(8), 738–745. https://doi.org/10.15171/ijhpm.2018.18
NRS 420 Health History Assessment for Tina Jones Example Transcript
Coming Soon
READ MORE >>
NRS 425 Health Promotion and Functional Health PatternIn this NRS-425 Health Pro ...
NRS 425 Health Promotion and Functional Health Pattern
In this NRS-425 Health Promotion and Population Health Course, the primary focus is on the community as the patient, taking into account varying cultures, spiritual values, geographic norms, and economic conditions. The critical aspects examined in this course encompass social determinants of health, including social, legal, and political variables impacting individual, community, and population health across the life span. Students use epidemiological data, functional health pattern assessments, and nursing theories to plan and intervene in areas of health promotion and disease prevention across the life span.
Example Functional Health Patterns Community Assessment Presentation Notes
Presentation Objectives
Hello everyone, and welcome to today’s presentation. The presentation will focus on assessing Columbus’ community health patterns. Columbus is one of the largest cities in Georgia. It is the third-largest city based on population density. It is a consolidated city-county located on the west-central border of Georgia. We will discuss the community in detail and its boundaries. An extensive community physical assessment will be addressed, including values, beliefs, health and health perception, nutrition, and environment. The social determinants of health for the community will also be explored. Finally, an interview with a community representative and the opportunities for health promotion in the community will be discussed.
Community Description (Geography and Geopolitical Factors)
The community of interest in this assessment is Columbus City in Georgia. It is the second-largest city in Georgia, with a large metropolitan area. The city is located on the west-central border of Georgia, directly along the Chattahoochee River. Additionally, the city’s metropolitan area is joined with the other cities in Alabama, such as Opelika and Auburn. Columbus was merged in 1970 as the official county seat for Muscogee County.
Community Boundaries (People, Ethnic, Financial, and Educational Levels)
Columbus is one of Georgia’s most densely populated cities, with approximately 979 people per square mile. According to the United States Census Bureau (2021), Columbus’s estimated population as of July 2021 was 205,617. More than 50 % of the residents are females. The city is diverse and houses people from different races. The races include white, Hispanic, Asian, black, American Indian and Native Hawaiian.
The majority of the people are white. The census report also included that the estimated household income in the city was $47,008. Additionally, the cost of living in Columbus is $86.8 per day, which is lower than the US average of $100 per day, thus being one of the most affordable cities in Georgia. The population is also educated, with almost 100% attaining a high school education. 61.6% of the population have a post-high school education, meaning bachelor’s, associate and college degrees.
Values and Belief Patterns
Columbus is a city that houses a community that highly regards community values such as peace, unity, and freedom. The family unit is also cherished, with approximately 47% of the adult residents being married. There are different religious beliefs in Columbus. Christianity is the leading religion, with approximately 59% of the residents being Christians from different denominations. However, about 37.9% of the residents are not ascribed to any religion. Community members participate in community programs and regularly meet and interact in community social institutions such as community libraries, schools, and religious centers.
Culture, Health Patterns and Health Management
The culture of a community significantly affects health patterns and health management. Cultural importance in Columbus is felt to a great extent since cultural days and events are observed. The city has various cultural centers where culture is expressed in terms of art. Ballet and Broadway are other cultural icons in the city. Cultural heritage and communism and cultural heritage are also valued. The health of the community and its members is regarded highly. Additionally, from the community reviews, the community views itself as a healthy community. There are adequate health management institutions since 10% of the common industries are healthcare-related.
Nutrition/ Metabolic
Despite the scarcity of data and statistics concerning Columbus City, the county and state statistics show relatively good nutrition. Healthy foods are available and affordable for people of all social classes. However, there is much junk and fast food served in local canteens and food trucks. Most of these fast foods are unhealthy. Safe water is available for consumption for all households and businesses. The statistics for obesity and diabetes are, however, still high. Approximately 12% of children and 30% of adults are obese. More so, the Centers for Disease Control and Prevention reported that approximately 12% of the total population in the city has diabetes.
Activities/Physical Exercise
For adults, children, and youths from inside and outside the city, the recreational centers include parks, community centers, play fields, and swimming pools. The availability, accessibility, and affordability of these centers encourage community members to engage in physical activity and exercise. There are also fitness programs. More than half of the households in Columbus have access to a computer, internet, and television, where the average television watching hours is approximately three hours. Road accidents are a significant form of injury in the city since road transport is the primary mode of transport (Ciy-data.com, n.d.). Therefore, fractures and brain and spinal injuries are common.
Self-perception and Self-concept
Getting the community’s self-perception and self-concept is essential in understanding community identity (Cater & Bruene, 2019). Various sources of pride exist that enhance the self-perception and self-concept of residents in Columbus. These factors include a low cost of living, which enables the residents of different social classes to afford and access most of the services in the city. The tourist attraction sites and parks act as areas of social interaction and meetings, thus enhancing unity and social cohesion. Most city residents are, on average, young, mostly between 18 and 65 years old. Different websites feature the city’s vital information, data, and statistics.
Stress and Coping with Stress
Stress is a significant factor influencing mental health and wellness in the community. The stress levels in Columbus are significantly high. There are various significant causes of stress in the city. Some of the most common causes of Stress include the unemployment rate, which is slightly below the state average, and crime rates.
For instance, sex offenders living in the city as of January 2023 were recorded at 738, with a ratio of offender: population at 252:1. The issue causes vulnerable populations to live in fear, including the victims living in Stress Locality. However, various attempts exist to cope with Stress, including the availability of counseling centers and therapists in the city. Columbus is also one of the cities with many male therapists in the state (City-Data.com, n.d.).
Sexuality and Reproductive Health
Like other communities in Georgia and the US, the community mainly conforms to individualism. Thus, low social interactions exist. Numerous sexual and reproductive health programs exist, facilitated by non-governmental organizations, faith-based organizations, and community organizations. These programs are population-specific, mainly offering services to vulnerable populations. The programs teach domestic violence, teen pregnancy, HIV, safe childcare, and motherhood. However, abortion and miscarriages are not well recorded, thus unavailability of a definite record. Maternal and childcare health services are free, promoting safe maternal and child care.
Environmental Health Concerns
There are various environmental health concerns in the city. Columbus is one of the cities that have recently recorded the highest fecal coliform contamination in the county (City-data.com, n.d.). The city also has sewers that flow into the Chattahoochee River. These two environmental health concerns can pose a considerable health risk in the community through cholera outbreaks. There are also noisy neighborhoods present, which is an environmental health concern.
The air quality in the city does not meet the annual WHO requirements, thus posing a health risk to the community. Air pollutants may cause health risks, including respiratory diseases. Households were observed to have clean and well-maintained toilets and bathrooms. General hygiene is maintained by having hand-washing points throughout the city.
Social Interactions and Common Goals in the Community
Social interaction is a very vital aspect of the community. Social interactions promote unity and cohesion and enhance community participation in various community initiatives. The rate of social interaction in Columbus is generally low, mainly due to the individualism in the community. However, community members interact once in a while in community social institutions such as the Chattahoochee Library, schools, recreation facilities, and religious institutions.
Additionally, Columbus is a metropolitan area; thus, various government institutions exist where people can interact. Some of the common goals in the community are increasing social cohesion and unity, reducing the crime rate challenge, and enhancing collective participation in health initiatives.
Barriers and Challenges in the Community
There are various barriers and challenges in Columbus City. Some of these challenges are interdependent. One of the significant challenges is high unemployment rates, especially among youths aged 25. The high population majorly causes the unemployment challenge. Unemployment rates in this community are slightly above the state rates. Unemployment is a major cause of crimes, which is also a significant challenge. Other challenges include drug abuse, traffic road accidents, and environmental barriers such as sewer overflows.
Social Determinants of Health
According to Peretz et al. (2020), social determinants of health in a community impact community members’ decisions on health, their lifestyle, and their general conduct. SDO is the conditions in which individuals in a community are born, brought up, and age. The assessment’s identified social determinants of health included economic stability, education access, and quality. The cost of living is relatively low compared to the state’s average. As a metropolitan city, there is high production and cash flow. The education levels are high, with 61.6% percent of the total population attaining post-high school education and above 80% having attained high school education.
The other social determinants of health identified in the community include healthcare access and quality, neighborhood and built environment, and social and community concepts. Healthcare facilities are available across the city regarding healthcare access and quality. These facilities are well endowed with care providers from different specializations. There is a high crime rate and security issues, mainly due to poverty and unemployment. The average commuting time is 19 minutes, showing good transport infrastructure (City-Data.com, n.d.). Additionally, despite exhibiting an individualistic society, the community has a certain degree of social cohesion and interaction.
Community Assessment Summary
Conducting the community assessment was essential and needed to understand the community in detail. Some of the community needs identified in the assessment include addressing environmental health concerns impacting its health, such as sewer overflows. Among the barriers to community health are drug abuse and crime rates. Understanding various concepts of the community, including their stress levels, coping with Stress, and self-perception, helped me understand the community’s view of health and their challenges. Additionally, the assessment confirmed the existing data and statistics through observation and actual community engagement.
Interview Summary/Responses
Healthcare providers play a significant role in providing healthcare information. The interview with Mr. Smith, a director of nursing in a long-term care facility, was crucial in understanding health promotion. Mr. Smith has worked as a nurse for the last 21 years and has been at the facility for 13 years. His ambition is to transform nursing care towards patients with chronic illnesses, primarily geriatric patients, by offering decent care and enhancing patient satisfaction.
Mr. Smith participates in health promotion programs in the community through partnerships with the government, healthcare providers, and other organizations. He believes that health promotion is one of the best and most cost-effective approaches to care since it refocuses health from curative to preventive health. He maintains that nurses play a significant role in health promotion.
According to Mr. Smith, the community’s health is slightly above average. He mentioned that the score is due to the community’s various health risks and the different environmental health concerns evident in the community. He cited the lack of insurance as one of the primary barriers to healthcare, especially for vulnerable populations and populations facing health disparities.
He also identified community health issues, including obesity, diabetes, and drug abuse. As a care provider, he aims to enhance decent care and patient satisfaction for all community members while advocating for health focus to shift to preventive health. Additionally, he desires to see the community free of drug abuse and embracing a healthy lifestyle.
Opportunities for Health Promotion
The health assessment and the community representative interview identified different health promotion opportunities. The health promotion opportunities were identified from the environmental health concerns, community challenges, and barriers. One of the most profound community health issues is drug and substance abuse. Research shows that drug abuse is manageable through community education, sensitization, and the use of available community resources (Volkow et al., 2019).
Similarly, this challenge offers a perfect health promotion activity that healthcare providers can focus on going forward. Additionally, the community lacks enough drug abuse programs and rehabilitation centers. Thus, the issue is a ready opportunity for health promotion. Other opportunities for health promotion include diabetes prevention and management, following high numbers of diabetes patients in the city, and mental health and wellness following stress levels and community stressors present.
Conclusion
The best health promotion opportunity is diabetes prevention and management. The problem can be controlled at the community level due to the available social institutions and groups where health promotion can be carried out. These include healthcare facilities, organizations, churches, and schools. Health promotion interventions potentially reduce the health concerns and challenges in the community, thus improving the overall health in Muscogee-Georgia.
Thank you.
References
Carter, M. J., & Bruene, S. (2019). Examining the relationship between self-perceptions of person, role, and social identity change and self-concept clarity. Imagination, Cognition and Personality, 38(4), 425-451. https://doi.org/10.1177/0276236618792267
Center for Disease Control and Prevention (CDC), (2022). Deaths and Mortality. National Center for Health Statistics. https://www.cdc.gov/nchs/fastats/deaths.htm
City-Data.com. (n.d.). Columbus, Georgia. http://www.city-data.com/city/Columbus-Georgia.html
Peretz, P. J., Islam, N., & Matiz, L. A. (2020). Community health workers and Covid-19—addressing social determinants of health in times of crisis and beyond. New England Journal of Medicine, 383(19), e108. https://doi.org/10.1056/NEJMp2022641
United States Census Bureau. (2021). City and Town Population Totals 2020-2021. Retrieved from https://www.census.gov/data/tables/time-series/demo/popest/2020s-total-cities-and-towns.html
Volkow, N. D., Jones, E. B., Einstein, E. B., & Wargo, E. M. (2019). Prevention and treatment of opioid misuse and addiction: a review. JAMA psychiatry, 76(2), 208-216. https://doi.org/10.1001/jamapsychiatry.2018.3126
READ MORE >>
compared to 93.3% of non-Hispanics. A Bachelor’s degree or higher is held by ...
A Bachelor’s degree or higher is held by 17.6% of Hispanics and 36.9% of non-Hispanics (US Census Bureau
READ MORE >>
NRS 429 VARK Analysis Paper SampleIntroductionIn 1992, Fleming and Mills came up ...
NRS 429 VARK Analysis Paper Sample
Introduction
In 1992, Fleming and Mills came up with a theory of teaching named VARK – Visual, Aural, Read/Write, and Kinesthetic theory that adequately captured the needs and the experiences of students and teachers. In nursing, VARK is a critical learning tool that helps students effectively translate theory learning into practice (Mozaffari et al., 2020). This style of learning caters to the needs of different learners by making what has been learned in the classroom a reality.
As the name suggests, VARK uses visual learning, the depiction of information using pictures, diagrams, and any pictorial representations. Similarly, VARK uses aural learning, which is the learning through hearing and speaking. Concerning reading and writing, which happen the most important models of learning, the model encourages extensive student immersion. Lastly, VARK also uses kinesthetic learning, the use of practice and experiences, whether real or simulated to achieve the desired learning goals.

The VARK Questionnaire
Learners have their preferred learning styles which is often determined by numerous factors such as one’s physical and mental status, the level of preparedness for learning, and personal likes and dislikes. According to Chiang (2017), the identification of the appropriate learning styles impacts how teachers impart knowledge to students and the overall student outcome. The VARK questionnaire is a learning tool that aids learning by suggesting to learners the best strategies they should use. For example, individuals with a strong affinity for visual presence will often go for learning modes that contain a lot of spacing, charts, diagrams, plans, maps, and graphs. Other learners simply prefer listening to their teachers, while others prefer the reading and writing modality of teaching.
My Preferred Learning Style.
Having answered all the VARK questionnaire questions in the link provided, I chose to learn styles that resonated well with me. The chosen styles are reading and writing, and visual styles of learning. The fact that I prefer two models of learning makes me multimodal rather than unimodal. Concerning visual learning mode, this mode of learning resonates with me because being a medical student, much of what I learn in theory must be translated into practice. Turning theory into images such as pictures, graphs, and charts is critical for me as a learner.
Concerning reading and writing, I prefer this approach of learning because it empowers me to deeply comprehend what I am taught by being able to write down notes and read them later. Through reading, I can analyze, evaluate, and dissect the teacher’s notes. Similarly, reading gives me the ability to conduct further research on a subject by doing further reading or analysis of the literature. For me, this modal of learning makes it easier to remember and memorize lessons easily. When I write down notes, I can easily recall what I have written much easier than what I have heard.
A Review of other Learning Styles
Visual Learning
This is a type of learning characterized by the use of images, colors, drawings, maps, charts, graphs, and any other form of pictorial representation. A visual learner has numerous characteristics that endear him/her to visual learning. Some of the characteristics that define visual learners include being observant, has a liking for colors, enjoys going through maps, charts, pictures, and graphs. These types of learners need to physically see/examine a teacher’s body language and facial expressions to understand better what is being taught.
Kinesthetic Learning
This is a type of learning where students learn through physical activities rather than watching demonstrations or listening to teachers lecturing. In Kinesthetic learning, a teacher can use a variety of physical activities to enhance learning. Some of the most important strategies of kinesthetic learning include role plays, body mapping, drawing, webbing, mind mapping, and story mapping (Hernandez et al., 2020). Other common techniques under kinesthetic learning are using certain computer technologies that allow a learner’s body to move while learning. Physical activities such as drama, sports, and dance can be used to bring out the best learning results for learners who prefer this type of learning model.
Aural Learning Style
This is a learning style characterized by learners acquiring information/knowledge through hearing what they are taught and giving back answers by speaking. Thus, hearing and listening form the core pillars of aural learning. For example, a teacher passes information to learners through lectures and an auditory learner learns what he/she’s taught through hearing and listening (Amaniyan et al., 2020). Such learners depend on remembering what they heard from their teachers but also have the opportunity to speak, answering questions or asking questions. Excellent examples of auditory learning include humming, reading out loudly, or talking to oneself.
How Individual Learning Styles Affect the Degree to which A Learner Can Understand or Perform Educational Activities
Learning styles have a direct impact on learning outcomes. However, each student has their preferred model of learning that resonates well with their personalities, ability, the level of intelligence, perception, and attitudes towards learning. Each learner experiences the learning process differently even if the learning environment is the same. This factor means that even in the same learning environment, students do not experience the same quality or level of learning. In a learning environment where a teacher prefers the reading and writing teaching model, students with high affinity to this learning style have an advantage over those who prefer other models (Leasa & Corebima, 2020). The same is true for other learning styles. It is incumbent on a teacher to develop a combination of teaching styles that appeal to all learners.
Importance of understanding the learning styles of individuals.
While it is difficult to meet the need of every learner, teachers must identify the learning styles preferred by each student. This act helps the teacher to create a teaching plan that caters to the need of all learners. This way, all students experience the same quality and level of teaching. Another critical reason for teachers to understand the learning styles of individuals is because preferred learning styles have a significant influence on student’s behavior. Noteworthy is that learning is not just about academic performance but also a means of molding learner’s behavior to turn them into responsible human beings. Behavior is a critical factor in learning and must be incorporated for better outcomes.
Conclusion
VARK is a critical learning tool that helps teachers to identify learner’s preferred learning styles. While some students do well with aural learning style, other students may prefer visual, reading/writing, or kinesthetic learning style. It is the duty of teachers to identify their learners preferred ‘learnings styles and create an effective teaching plan that addresses the need of every student. Even in the same learning environment, students do not experience the same quality or level of learning which means that some may lag. For this reason, it is incumbent on teachers to ensure that all learners get the best through inclusivity.
NRS 429 VARK Analysis Paper References
Amaniyan, S., Pouyesh, V., Bashiri, Y., Snelgrove, S., & Vaismoradi, M. (2020). Comparison of the Conceptual Map and Traditional Lecture Methods on Students’ Learning Based on the VARK Learning Style Model: A Randomized Controlled Trial. SAGE Open Nursing, 6, 2377960820940550. https://doi.org/10.1177/2377960820940550
Chiang, Y. C., Chen, C. H., Liao, Y. C., & Liao, C. W. (2016). A Study on Investigating Learning Styles and Skills Learning Motivations for Mechanical Department Students in Vocational High Schools. International Journal of Information and Education Technology, 6(11), 851. DOI:10.7763/ijiet.2016.v6.804
Hernandez, J. E., Vasan, N., Huff, S., & Melovitz-Vasan, C. (2020). Learning Styles/Preferences Among Medical Students: Kinesthetic Learner’s Multimodal Approach to Learning Anatomy. Medical Science Educator, 30(4), 1633-1638. https://doi.org/10.1007/s40670-020-01049-1
Leasa, M., & Corebima, A. D. (2017). Emotional Intelligence among Auditory, Reading, and Kinesthetic Learning Styles of Elementary School Students in Ambon-Indonesia. International Electronic Journal of Elementary Education, 10(1), 83-91. https://www.iejee.com/index.php/IEJEE/article/view/301
Mozaffari, H. R., Janatolmakan, M., Sharifi, R., Ghandinejad, F., Andayeshgar, B., & Khatony, A. (2020). The relationship between the VARK learning styles and academic achievement in Dental Students. Advances In Medical Education And Practice, 11, 15. https://doi.org/10.2147%2FAMEP.S235002
NRS 429 VARK Analysis Paper Week 1 Instructions
Learning styles represent the different approaches to learning based on preferences, weaknesses, and strengths. For learners to best achieve the desired educational outcome, learning styles must be considered when creating a plan. Complete “The VARK Questionnaire,” located on the VARK website, and then complete the following:
- Click “OK” to receive your questionnaire scores.
- Once you have determined your preferred learning style, review the corresponding link to view your learning preference.
- Review the other learning styles: visual, aural, read/write, kinesthetic, and multimodal (listed on the VARK Questionnaire Results page).
- Compare your current preferred learning strategies to the identified strategies for your preferred learning style.
- Examine how awareness of learning styles has influenced your perceptions of teaching and learning.
In a paper (750-1,000 words), summarize your analysis of this exercise and discuss the overall value of learning styles. Include the following:
- Provide a summary of your learning style according the VARK questionnaire.
- Describe your preferred learning strategies. Compare your current preferred learning strategies to the identified strategies for your preferred learning style.
- Describe how individual learning styles affect the degree to which a learner can understand or perform educational activities. Discuss the importance of an educator identifying individual learning styles and preferences when working with learners.
- Discuss why understanding the learning styles of individuals participating in health promotion is important to achieving the desired outcome. How do learning styles ultimately affect the possibility for a behavioral change? How would different learning styles be accommodated in health promotion?
Cite to at least three peer-reviewed or scholarly sources to complete this assignment. Sources should be published within the last 5 years and appropriate for the assignment criteria.
Prepare this assignment according to the guidelines found in the APA Style Guide, located in the Student Success Center.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are required to submit this assignment to LopesWrite. A link to the LopesWrite technical support articles is located in Course Resources if you need assistance.
NRS 429 VARK Analysis Paper Rubric Criteria
Collapse All Rubric CriteriaCollapse All
Personal Learning Styles According to VARK Questionnaire
20 points
Criteria Description
Personal Learning Styles According to VARK Questionnaire
- Excellent
20 points
Personal learning style according to the VARK questionnaire is identified and described in detail. Summary offers examples that display personal insight or reflection.
Preferred Learning Strategies
20 points
Criteria Description
Preferred Learning Strategies
- Excellent
20 points
Personal learning strategy is clearly described. A comparison of current preferred learning styles and VARK identified learning styles is detailed. Overall discussion demonstrates insight into preferred learning strategies and how these support preferred learning styles.
Learning Styles
20 points
Criteria Description
Learning Styles (Effect on educational performance and importance of identifying learning styles for learners as an educator)
- Excellent
20 points
Importance of learning styles for a learner, and importance of educator identifying individual learning styles and preferences when working with learners, is thoroughly discussed. The importance of learning styles for learners participating in healthy promotion, and identifying them as an educator, is clearly established. Strong rationale and evidence support discussion.
Learning Styles and Health Promotion
20 points
Criteria Description
Learning Styles and Health Promotion (learning styles and importance to achieving desired outcome for learners, learning styles and effect on behavioral change, accommodation of different learning styles in health promotion)
- Excellent
20 points
Understanding the learning styles of individuals participating in a health promotion, and the correlation to behavioral change and achieving desired outcomes is discussed in detail. A strong correlation has been established. Accommodation of different learning styles is discussed. The narrative demonstrates insight into the importance of learning styles to health promotion and behavioral outcomes.
Thesis Development and Purpose
5 points
Criteria Description
Thesis Development and Purpose
- Excellent
5 points
Thesis is comprehensive and contains the essence of the paper. Thesis statement makes the purpose of the paper clear.
Argument Logic and Construction
5 points
Criteria Description
Argument Logic and Construction
- Excellent
5 points
Clear and convincing argument that presents a persuasive claim in a distinctive and compelling manner. All sources are authoritative.
Mechanics of Writing (includes spelling, punctuation, grammar, language use)
5 points
Criteria Description
Mechanics of Writing (includes spelling, punctuation, grammar, language use)
- Excellent
5 points
Writer is clearly in command of standard, written, academic English.
Paper Format (use of appropriate style for the major and assignment)
2 points
Criteria Description
Paper Format (use of appropriate style for the major and assignment)
- Excellent
2 points
All format elements are correct.
Documentation of Sources
3 points
Criteria Description
Documentation of Sources (citations, footnotes, references, bibliography, etc., as appropriate to assignment and style)
- Excellent
3 points
Sources are completely and correctly documented, as appropriate to assignment and style, and format is free of error.
Your VARK Results
Your scores were:
- Visual 0
- Aural 6
- Read/Write 3
- Kinesthetic 8
Your learning preference:Mild Kinesthetic
Share
People with your preference like:
practical exercises, experiences, examples, case studies, trial and error, things that are real, …Full information about your preference is available in your VARK Academic Profile or Business Profile (US$10.57).
View Example Profile
Use the following helpsheet for strategies that apply to your VARK preference:
- Kinesthetic Strategies
- Understanding the results
- NEW! VARK and Online Learning
- NEW! Read about the experiences of others with the same learning preference as you – and add your own experiences.
Next, fill in the Current Strategies Questionnaire to find out whether the learning strategies you currently use are the best for your learning preference.
NRS 429 Week 3 Assignment Social Determinants of Health Sample Solution
The World Health Organization ascribes the social domain of health as an important determinant of an individual’s well-being. The social determinants of health (SDOH) are economic and social factors that influence the health of an individual or a group of people (Schroeder et al., 2019). The distribution of social and economic conditions contributes to health disparities between rich and poor people. While focusing on a specific family, this paper aims to provide insight into the SDOH, appropriate health-promoting activities, and a health model that lays out a concrete plan for carrying out the activities.
Description of the SDOH Affecting John’s Family
The SDOH has an impact on John’s family, just like it does on any other family. SDOH components affecting the family include economic stability, healthcare and quality, social and community context, education, neighborhood, and the environment. John is a structural engineer, and her wife is an accountant at a five-star restaurant nearby. When they pool their resources, they are capable of providing basic needs such as food, clothing, housing, health, and education to their children. In terms of literacy, John and his wife have completed tertiary education. Their perception of health is positive, as evidenced by Anne having a cervical cancer screening and John taking his antihypertensive medications and monitoring his blood pressures daily.
The neighborhood and environment in which they live are urban. The city has a consistent supply of safe drinking water and electricity, residents rarely suffer from illnesses caused by contaminated water. The only issue may be the continuous air pollution caused by gases emitted by motor vehicles and the numerous factories in the area. In the long run, the emitted gases may endanger the family of respiratory illnesses.
In terms of healthcare and quality, the city is brimming with health facilities offering diverse services, as Anne discovers when she walks into a cervical cancer screening clinic. Furthermore, the surrounding community is supportive, with numerous health-promoting facilities such as gyms, swimming pools, and football fields. However, as evidenced by their sedentary lifestyle, John’s family does not routinely use the resources that put them at risk of diseases like hypertension, which John has, and obesity, which his wife has.
Age-Appropriate Screening for Each Family Member
Health promotion encompasses a wide range of activities and interventions aimed at lowering disease risks. While primary health prevention and promotion strategies aim to prevent disease before it occurs, secondary strategies aim to reduce the impact of a disease that has already occurred, which is accomplished through early disease detection and treatment to halt progression.
Tertiary strategies, on the other hand, seek to reduce disease complications and long-term effects (Kisling & Das, 2022). Because it aims to detect and treat diseases in their early stages, screening is a component of secondary health prevention and promotion. John, who has hypertension, may benefit from screening for the other components of metabolic syndrome, including hyperlipidemia, diabetes, and obesity. Measurements of lipid levels, random blood glucose levels, and body mass index are used to screen for hypercholesterolemia, diabetes mellitus, and obesity, respectively.
Anne would benefit similarly from screening for other components of the metabolic syndrome, such as hypertension, diabetes, and hyperlipidemia. Furthermore, since her mother succumbed to cervical cancer, she had undergone a cervical cancer screening, which turned out negative. Obtaining Abi’s height and weight would be critical in calculating his body mass index, which determines whether he has a healthy weight or not. Moreover, due to Abi’s family’s history of metabolic syndrome, blood pressure, random blood sugar levels, and lipid levels must all be obtained. Sophy and Amor will be subjected to the same screenings as Abi. Because they live in a densely populated city with a recent high Covid19 transmission risk, all family members require a Covid-19 screening.
Health Model to Create an Action Plan
The health belief model is one of the earliest and most widely used models in matters of health prevention and promotion. The model focuses on an individual’s beliefs and how they impact their behaviors. The model encompasses six factors that impact an individual’s behavior. The factors include (1) perceived susceptibility, in which a person is subjectively aware of the risk of his illness, (2) perceived severity, in which a person is fully aware and feels the severity of his/her illness, and (3) perceived benefits, in which an individual consciously perceives the effectiveness of a behavior change, (4) perceived barriers, which define the obstacles to the action plan, (5) a cue to action which is a stimulus that prompts a decision-making process and (6) self-efficacy, which is the level of confidence a person obtains following achievement of their health promotion goals (Green et al., 2020). Concerning his family, John is aware that physical inactivity and alcohol consumption are risk factors for his illness-hypertension. He is also aware of the severity of his condition-hypertension-and has identified the barriers to achieving healthy blood pressure.
Steps for a Family-Centered Health Promotion
The vast majority of family-friendly interventions are behavioral. First, the family must engage in sweat-inducing physical activity for at least 30 minutes per day, five times per week, for a total of 150 minutes per week, as per the American Heart Association’s recommendation. Second, a dietary plan that meets the goals of John and Anne, as well as the children, is required. The DASH diet will benefit John, whereas Anne should avoid junk food and limit her calorie intake.
Reducing risk behaviors like alcohol consumption and cigarette smoking is an important step in family-centered health promotion and contributes significantly to the reduction of cardiovascular disorders (Perumareddi, 2019). Medication adherence and regular visits to a primary care physician by all family members are other effective prevention strategies. The family has health communication strategies in place, and the discussions take place during scheduled family time, usually at night, during meal times. Each member is allowed to contribute and express their opinion on the family’s health, as well as make suggestions on how to improve their health.
Conclusion
Whether health prevention and promotion are superior to curative interventions is still contentious. Due to the high prevalence of preventable diseases, it is prudent to prevent their occurrence or halt their progression in their early stages. This heralds the concept of different levels of health prevention, such as primary, secondary, and tertiary. Disease screening is a practice that aims to detect diseases at an early stage so that interventions can be implemented to prevent progression. This approach has significantly reduced morbidity from diseases such as cancer while also relieving patients of the financial burden that would have resulted from treating advanced disease.
References
Green, E. C., Murphy, E. M., & Gryboski, K. (2020). The health belief model. In The Wiley Encyclopedia of Health Psychology (pp. 211–214). Wiley. https://doi.org/10.1002/9781119057840.ch68
Kisling, L. A., & Das, J. M. (2022). Prevention Strategies. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK537222/
Perumareddi, P. (2019). Prevention of hypertension related to cardiovascular disease. Primary Care, 46(1), 27–39. https://doi.org/10.1016/j.pop.2018.10.005
Schroeder, K., Garcia, B., Phillips, R. S., & Lipman, T. H. (2019). Addressing social determinants of health through community engagement: An undergraduate nursing course. The Journal of Nursing Education, 58(7), 423–426. https://doi.org/10.3928/01484834-20190614-07
NRS-429 Week 4 Health Promotion in Minority Populations
Select an ethnic minority group that is represented in the United States (American Indian/Alaskan Native, Asian American, Black/African American, Hispanic/Latino, Native Hawaiian, or Pacific Islander). Using health information available from Healthy People, the CDC, and other relevant government websites, analyze the health status for this group.
In a paper of 1,000-1,250 words, compare and contrast the health status of your selected minority group to the national average. Include the following:
- Describe the ethnic minority group selected. Describe the current health status of this group. How do race and ethnicity influence health for this group?
- What are the health disparities that exist for this group? What are the nutritional challenges for this group?
- Discuss the barriers to health for this group resulting from culture, socioeconomics, education, and sociopolitical factors.
- What health promotion activities are often practiced by this group?
- Describe at least one approach using the three levels of health promotion prevention (primary, secondary, and tertiary) that is likely to be the most effective in a care plan given the unique needs of the minority group you have selected. Provide an explanation of why it might be the most effective choice.
- What cultural beliefs or practices must be considered when creating a care plan? What cultural theory or model would be best to support culturally competent health promotion for this population? Why?
Cite at least three peer-reviewed or scholarly sources to complete this assignment. Sources should be published within the last 5 years and appropriate for the assignment criteria and public health content.
Prepare this assignment according to the guidelines found in the APA Style Guide, located in the Student Success Center.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are required to submit this assignment to LopesWrite. A link to the LopesWrite technical support articles is located in Course Resources if you need assistance.
Health Promotion in Minority Populations Example Essay
Ethnicity is a medically relevant factor owing to its influence on one’s vulnerability to certain diseases, such as diabetes, as well as its influence on the age at which a disease occurs, such as breast cancer, which occurs at a relatively younger age in Blacks than in Whites. Poverty rates among ethnic minorities are significantly higher than among dominant racial groups, demonstrating the impact of ethnicity on an individual’s social status (US Census Bureau, 2021).
However, disparities in access to medical care exist across multiple contexts, including residence, gender, and age. The Hispanic population is an ethnic minority group that faces social disadvantages and thus suffers disproportionately from health issues when compared to other dominant racial groups (USDHHS, 2021). This group, however, is cognizant of their societal status and engages in health promotion activities to improve their physical and psychological health. This paper aims to describe this group in various contexts, such as health disparities, health barriers, health promotion activities, and cultural activities that may influence their health plan.
Description of the Ethnic Minority: Hispanics
In terms of ethnic and racial fragmentation, the United States is very diverse. According to the 2019 US Census Bureau, the Hispanic population accounts for 18.4% of the total population of the United States, or 60.5 million people (US Census Bureau, 2020). The group includes people of Mexican, Cuban, Puerto Rican, South or Central American, or other Spanish origins, with Mexicans constituting the majority (61.4%) of the population (US Census Bureau, 2020). More than half (55%) of the US Hispanic population lives in three states: California, Texas, and Florida, with California having the nation’s largest Hispanic population of approximately 145.57 million (World Population Review, 2022).
The statistics further show that 71.1% of Hispanics speak a language other than English (Us Census Bureau, 2020). In terms of health, this population’s life expectancy is 82.1 years, which is slightly higher than the projected 80.6 years for non-Hispanic Whites (US Census Bureau, 2020). Health in this group is influenced by cultural/language factors, access to preventive healthcare, and a lack of insurance coverage, with statistics showing that 18.7% of the Hispanic population were uninsured by 2019, which is higher than the 6.3% percent of the non-Hispanic population (US Census Bureau, 2020). The group’s low insurance rates exacerbate its disadvantages in accessing healthcare.
Health Disparities for the Group
The population faces a high burden of health problems, which have been attributed to a variety of factors. Nota
READ MORE >>
